For the past two decades, an important psychiatric rationale for involuntary hospitalization has been that patients who initially object to being hospitalized change their views after receiving hospital treatment
(1,
2). It has been argued that patients may even be grateful that clinicians overrode their initial refusals of hospital treatment. Stone
(1) called this rationale for involuntary hospitalization the “thank you” theory. In the current article we examine how patients’ evaluations of a psychiatric hospitalization changed between admission and a period approximately 1 month after discharge.
There have been few attempts to learn whether patients actually change their views about the necessity for hospitalization after they have experienced it. Kane et al.
(3) interviewed 75 involuntarily hospitalized patients after their admission to the hospital and then selected 35 patients who strongly objected to one or more aspects of their commitment and reinterviewed them before discharge. At each interview, Kane et al. asked patients several questions about their hospitalization, including, Should you have been committed? Patients gave significantly more positive responses to this question during the interview near discharge than during the admission interview. Kane et al. noted, however, that their results need to be interpreted cautiously because patients were selected for reinterview because of their strong objections to commitment; therefore, a regression to the mean, in which strong opinions ameliorated over time, would register as a shift toward more positive attitudes toward commitment.
Beck and Golowka
(4) interviewed 104 state hospital patients about their hospitalization and reinterviewed 60 of them at discharge. They found that, although many patients expected little or no benefit from hospital treatment at admission, a large proportion reported at discharge that they had received benefit from treatment. Beck and Golowka noted, however, that their data may have been biased in the direction of overreporting patients with good outcomes, because the latter were inadvertently more likely to be reinterviewed.
In this study, we examined whether patients revised their beliefs after they were discharged from the hospital and returned to the community. We used a larger study group of reinterviewed patients than previous studies, as well as recently developed instruments for eliciting patients’ views about their hospital admission
(5–
7).
METHOD
Study Group
Between July 1992 and August 1994, we studied 293 voluntary and 140 involuntary patient admissions (total N=433) at two university-based psychiatric hospitals: one in Pennsylvania (N=237) and one in Virginia (N=196). Patients were interviewed within 48 hours of admission to one of the hospitals. (Additional details, including a description of the differences between the study groups at the two sites, have been reported elsewhere [
5,
8,
9].) We selected the study group consecutively except when so many patients were admitted that they could not be interviewed within the time limit or when patients’ involvement with treatment precluded their taking time for the interview.
Patients with diagnoses of dementia or more than mild mental retardation were excluded because they had difficulty completing the interview. The Pennsylvania and Virginia interviewers were trained together, including observing each other’s interviews and periodically reviewing audiotapes of each other’s interviews. Patients gave written informed consent to participation after hearing a complete description of the study.
The Virginia and Pennsylvania sites were slightly different in the ways in which they regulated short-term commitments. Pennsylvania allowed the emergency detention of patients for 5 days for observation before a longer-term commitment hearing. Virginia restricted their short-term commitments to 72 hours. Both states require that, to be committable, an individual must be mentally ill and either dangerousness to self or others or unable to care for himself or herself. In addition, Virginia permits commitment of individuals who are mentally ill if they are at risk of substantial deterioration. In neither site was there significant use of outpatient commitment. Moreover, none of our study subjects was committed as an outpatient after the index admission. Of the 270 subjects whom we followed, 47 (17%) were committed for a longer period of time than the brief emergency commitment. In this article, when we refer to “legal status” or “commitment,” we are referring to legal status at admission—either voluntary or emergency committed—as opposed to the patient’s status after any later commitment hearing.
We interviewed patients after admission to the hospital and then reinterviewed them between 2 and 6 weeks after discharge, when they were in the community and under no legal compulsion to receive psychiatric treatment. Follow-up interviews were obtained for 270 (62%) of the 433 patients interviewed the first time. The primary reason for not interviewing patients the second time was the difficulty in locating them.
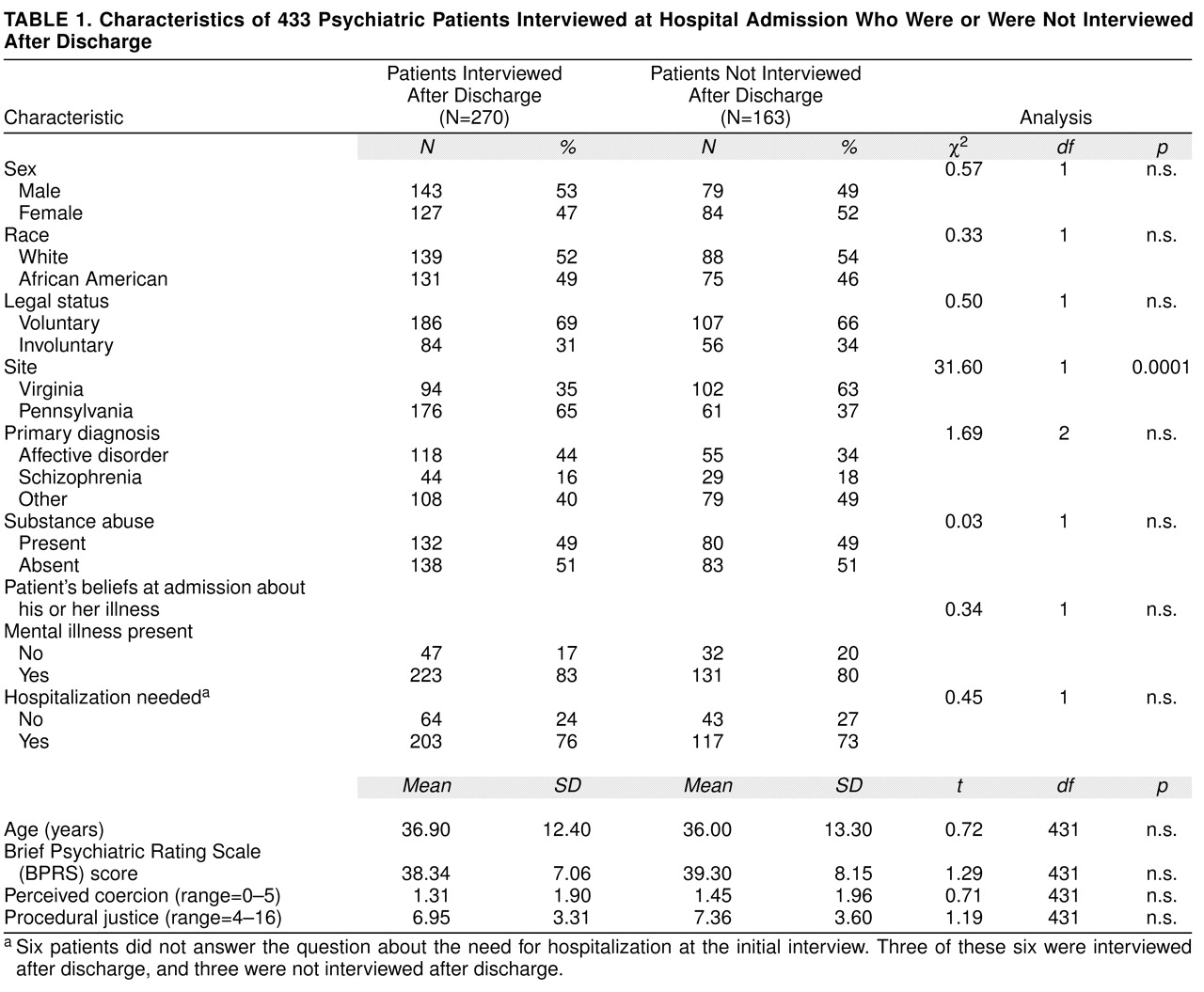
Table 1 shows that patients with follow-up interviews did not differ from those without interviews on age, sex, race, legal status after admission, primary diagnosis, or whether a substance abuse diagnosis was present. Most important, they did not differ on perceived coercion—whether they believed that hospitalization was needed or whether they had a mental illness. The patients from Pennsylvania, however, were significantly more likely to have a follow-up interview. The difference in follow-up rates was largely attributable to the urban versus rural character of the sites: patients released from the rural (Virginia) hospital dispersed to a much larger area and were therefore harder to locate and reinterview.
Measures
Each interviewee was administered a semistructured interview, the MacArthur Admission Experience Interview
(7). This interview focused on the interviewee’s perceptions of 1) coercion in the decision to be admitted, 2) any pressures to be hospitalized brought to bear on the patient, and 3) how the patient was treated by others while coming to the hospital and being admitted. The interview included structured questions for which the patient chose from predetermined answer sets. These questions yielded several scores reflecting the three listed aspects of the admission process.
Perceived coercion
In a previous article
(5), we reported psychometric analyses of four questions in the Admission Experience Interview that make up the MacArthur Perceived Coercion Scale. These questions focus on influence (What had more influence on your being admitted: what you wanted or what others wanted?), control (How much control did you have?), choice (You chose or someone made you?), and freedom (How free did you feel to do what you wanted?). These questions were weighted by using a principal components analysis to yield a 0–5 scale of perceived coercion on which higher values indicated more perceived coercion (mean=1.75, SD=2.07).
Pressures
We also asked about the occurrence of several different ways in which others might have tried to influence the decision about hospitalization (“pressures”). The pressures included persuasion (Did anyone try to talk you into going to the hospital or being admitted?), inducement (Did anyone offer or promise you something?), threats (Did anyone threaten you?), and force (Did anyone try to force you?). All of these questions had dichotomous yes-or-no answers. Pressures were summarized by variables indicating whether the patient reported any persuasion or inducement (positive pressures) or any threats or attempts to force admission (negative pressures).
Procedural justice
Patients were asked four questions about their perceptions of the procedural justice administered to them during their admission
(7). These questions involved patients’ perceptions of validation (How seriously did people consider what you had to say?), process satisfaction (How satisfied were you with how people treated you when you were coming into the hospital?), fairness (How fair was the process of coming into the hospital?), and voice (How much chance did you have to say everything you wanted about coming into the hospital?). Patients responded by using 4-point scales (e.g., for fairness, 4=very fair, 3=mostly fair, 2=mostly unfair, 1=very unfair). Procedural justice was the sum of the scores for each question. (This is a slightly different scoring of this variable than was reported previously
[7].)
Need for hospitalization
During the admission interview, patients were asked, Do you believe that you need to be in a hospital? Patients responded to these questions on a 6-point scale (definitely no, probably no, a little no, a little yes, probably yes, definitely yes). To simplify this presentation, and because the variable is bimodally distributed, we recoded the following responses as no: definitely no, probably no, a little no; all yes responses were similarly recoded as yes.
RESULTS
For this article we focused on patients’ beliefs about their need to be hospitalized. First, we examined factors that were associated with patients’ judgments at the initial interview about whether they needed to be hospitalized. Then we examined changes in patients’ views and factors associated with these changes. In what follows, our statistical tests were divided into three groups. For each group, the Bonferroni test procedure was used to ensure that the group-wise chance of at least one falsely significant result was less than 0.05.
Admission to the Hospital
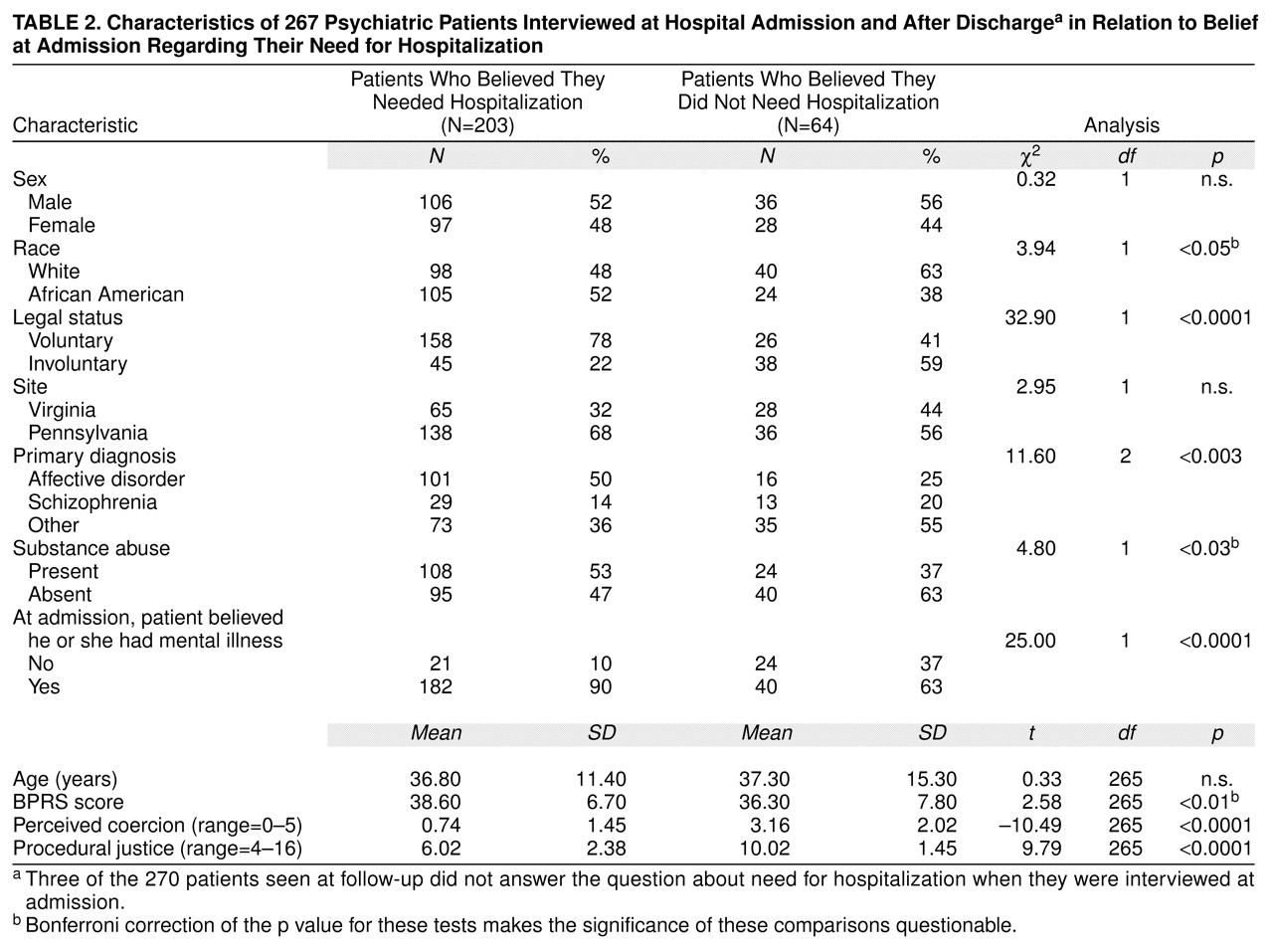
Table 2 shows that most patients (76%) believed that they needed to be hospitalized. Patients who reported at admission that they needed hospitalization were not different from those who said that they did not in sex, site, or age. White patients were slightly less likely to report that they needed hospital treatment than African American patients did. Individuals with affective disorder were much more likely to say that they needed to be admitted than patients with other diagnoses. We speculate that the depressed patients (who made up most of the affective category) were in pain and wanted help. Patients who believed that they did not need to be hospitalized had lower BPRS severity scores than those who believed that they needed hospitalization. Similarly, patients who believed that they did not need to be hospitalized were less likely to have a substance abuse disorder.
Not surprisingly, patients who reported that they needed hospital treatment were substantially more likely to say that they had a mental illness. Patients who said that they needed hospital treatment also reported much less coercion and much more procedural justice during the admission. Patients who stated that they did not need hospitalization were more likely to be admitted involuntarily than patients who endorsed a need for hospitalization. Were these patients admitted involuntarily just because they stated that they did not need hospitalization? Although our data provide no further insight into the reasons for involuntary admission, it is natural that patients who did not see the need for hospitalization would be less likely to enter the hospital voluntarily. Nevertheless, believing that one did not need hospitalization was not a sufficient or automatic ground for commitment, because 41% of patients who did not believe they needed hospitalization entered voluntarily anyway.
Change From Admission to Follow-Up
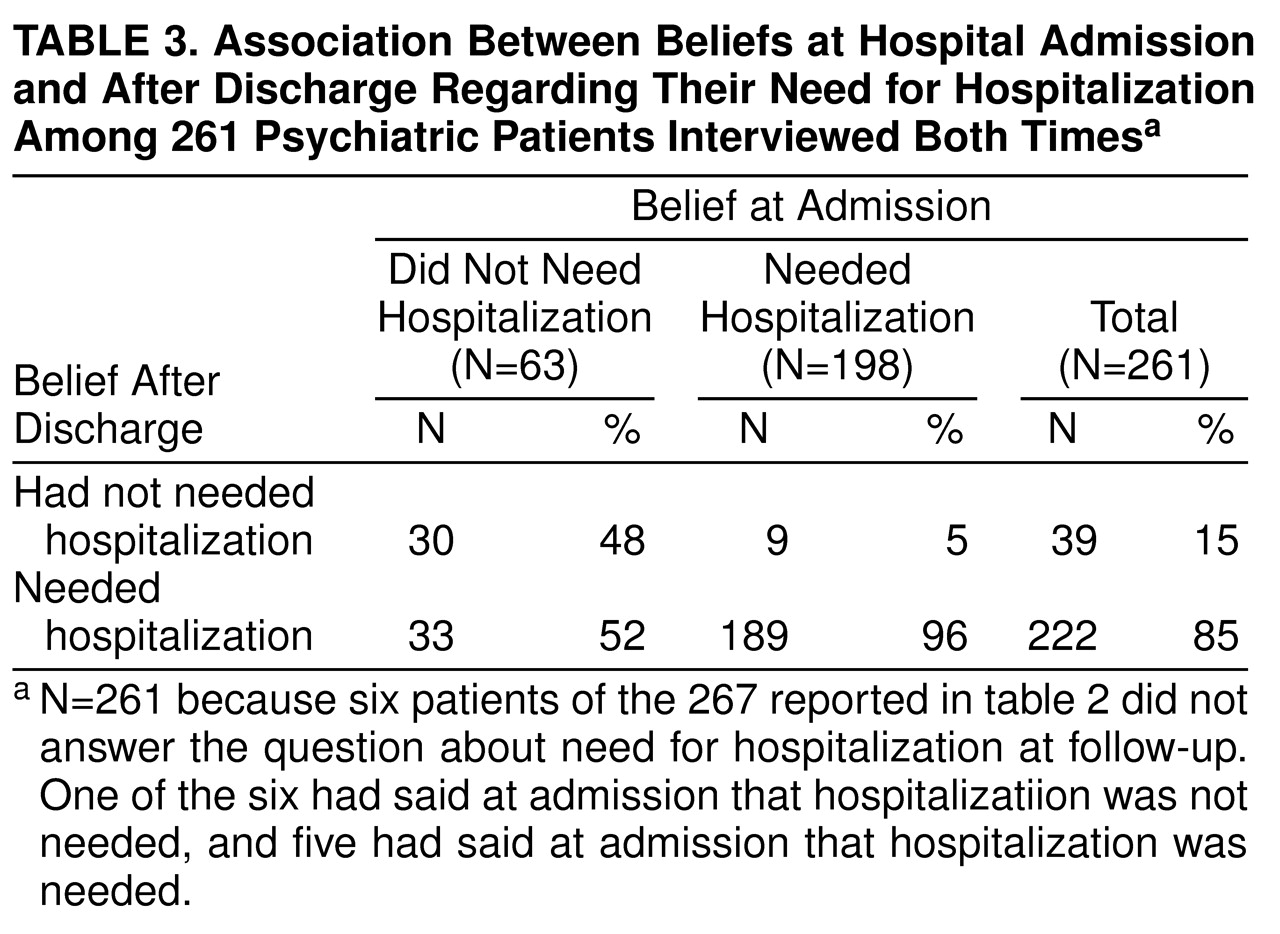
Table 3 shows that about half of the patients (52%) who said that they did not need hospitalization at admission changed their views at the follow-up interview. In contrast, only 5% of the patients who stated at admission that they needed to be hospitalized changed their views. The comparison between the rates of change in beliefs was significant by McNemar’s test (χ
2=12.59, df=1, p<0.001)
(10).
Covariates of Changes in Belief
It is important to see what patient characteristics might be associated with changes in beliefs about the need for hospitalization. Whether patients who initially believed that they did not need to be hospitalized changed their views was not significantly associated with the patients’ race, sex, age, or the site at which the patient was hospitalized. Neither was it associated with whether the patient was angry about the admission at the time of the admission interview or felt deceived during the admission. Interestingly, patients who changed their views did not differ in the severity of their illness at admission as measured by BPRS scores (mean=36.97, SD=8.28) from patients who did not change their views (mean=36.67, SD=7.89) (t=0.15, df=64, p<0.88).
Change in the belief that one needed to be hospitalized had an important but complex relationship to legal status.
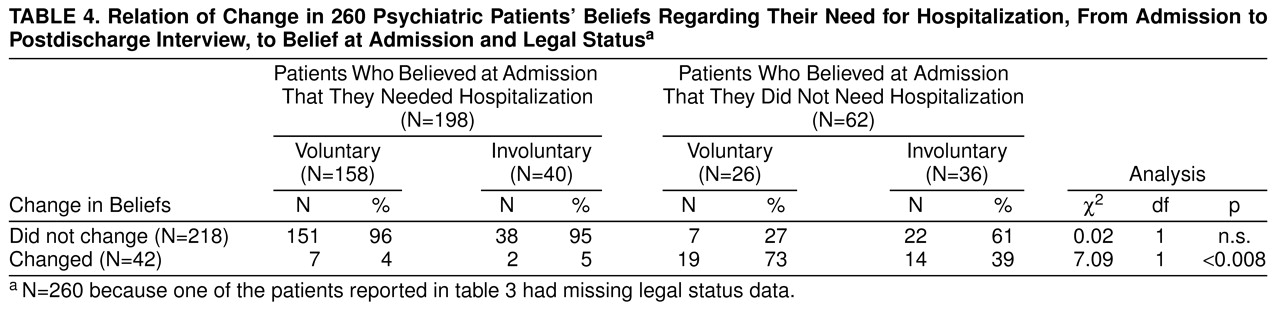
Table 4 shows that among those patients who believed at admission that they needed hospitalization, legal status was not associated with change in belief. However, among those patients who believed at admission that they did not need hospitalization, voluntary legal status was associated with a change to the belief at follow-up that they needed hospitalization.
Change of belief was also related to believing at admission that one had a mental illness. Of 39 patients who believed that they did not need hospitalization but that they had a mental illness, 25 (76%) subsequently changed their views about the need for hospitalization, compared with only eight (35%) of 23 patients who did not believe they needed hospitalization and did not believe they had a mental illness. One patient who believed that he had a mental illness but did not believe that hospitalization was needed did not answer the need for hospitalization question at follow-up. Similarly, of the 45 patients who believed at admission that they did not need to be hospitalized but who felt that they had been coerced, 20 (44%) changed their belief in the need for hospitalization, compared with 13 (72%) of 18 patients who believed at admission that they did not need to be hospitalized but who did not feel that they had been coerced (χ2=3.97, df=1, p<0.05).
Alternative Interpretations of Patients’ Revisions of Beliefs
There were some plausible reasons why patients might respond differently at admission than they do after hospitalization that did not involve changes in belief. For example, patients might have described their admissions in positive terms at follow-up because they perceived a risk of being rehospitalized if they were critical. We think that this was unlikely. The interviewer was identified to the patient as a member of a research team rather than clinical staff, and patients were assured that responses would be kept confidential. The interviewers also believed that patients responded candidly. More plausibly, patients in a community setting might have responded positively to questions about their hospital admissions because they were being interviewed in a noncoercive setting and at a less stressful point in their lives than at admission. The effect of treatment might have been to render the patient more likely to respond positively to any evaluative question about hospitalization. Thus, a tendency to agree that treatment was necessary might have reflected a general brightening of mood rather than a change in belief about the necessity for hospitalization.
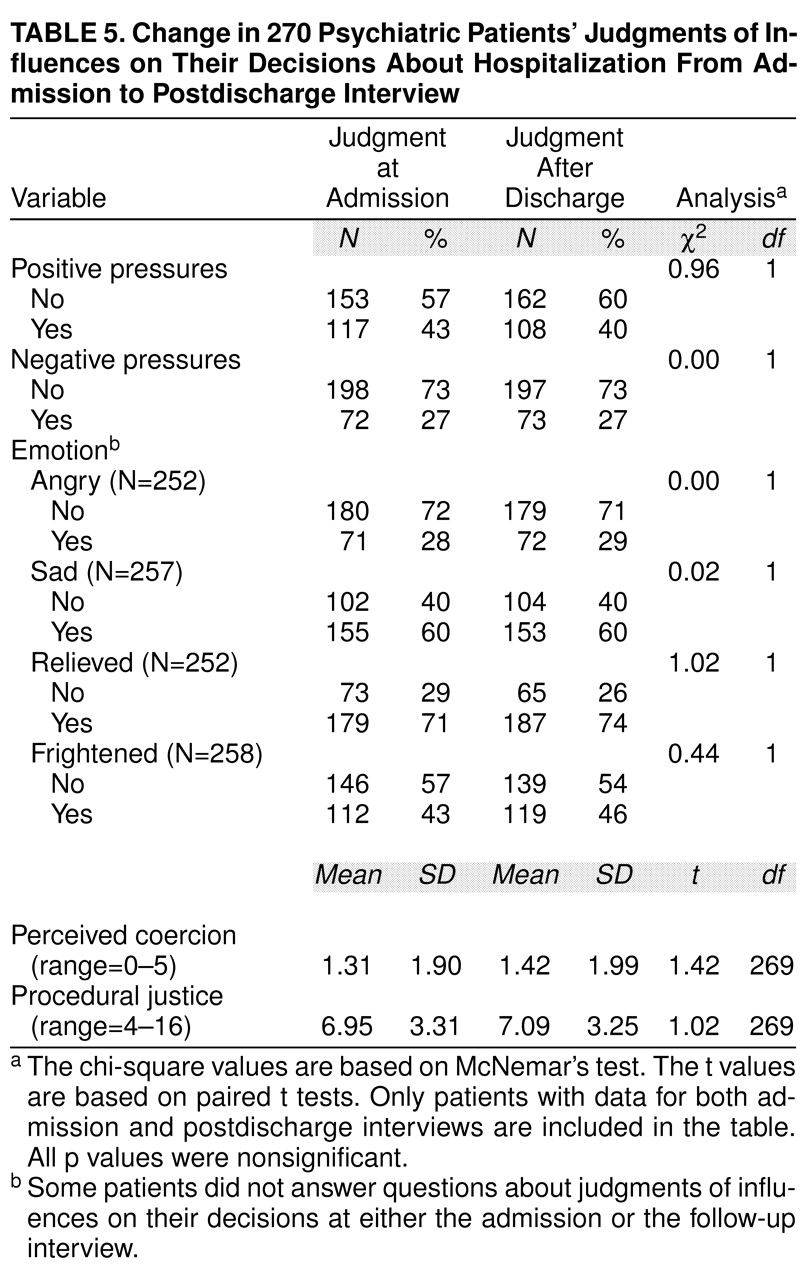
These alternative interpretations of the shift in beliefs about need for hospitalization were testable because they both implied that patients would have responded more positively at follow-up to any retrospective question that evaluated their admission. However, patients held stable views on most evaluative questions (
table 5). Patients’ judgments of perceived coercion, procedural justice, negative pressures, and positive pressures did not change from admission to follow-up. The small and nonsignificant differences in the means were toward patients reporting more coercion and less procedural justice during the follow-up interview. Nor did patients’ reports about their emotional responses to the hospital admission change. None of these responses changed significantly from the admission to the follow-up interview. Therefore, there is no evidence that patients were changing their responses because of a brightening of mood.
Another alternative explanation for these data is that there was a selection effect influencing which patients participated in the follow-up interview. Patients who did not return for the second interview might have had a different pattern of changes in belief. Had we been able to interview those patients, their data combined with those of patients whom we did interview might have altered our conclusions. Because we do not know how the patients who were not interviewed would have responded to our questions, we cannot rule out this possibility with certainty. However, it seems unlikely, given that none of the differences between follow-up participants and nonparticipants presented in
Table 1 was statistically significant, except for the site where the patient was admitted. It is important that how patients responded to the question about the need for hospitalization was not associated with whether a follow-up interview occurred.
A final possibility is that the shift in views was less dramatic than it appeared and that many patients who expressed the view that they did not need hospital treatment were actually more ambivalent than they stated when being pressured to come into the hospital. It may be that the “change” in attitude was less a change than a willingness to admit ambivalence in a less confrontational situation. This is consistent with our findings, which, however, contain no clear evidence to support this view. Further research will be needed to clarify this issue.
DISCUSSION
Patients’ posttreatment reports of changed beliefs in their need for hospitalization can best be understood by considering Alan Wertheimer’s analysis of what he called the “retrospective” rationale for psychiatric coercion
(11):
What, then, does the retrospective theory show? If a reasonable number of patients come to retrospectively approve of CT [coercive treatment], retrospective approval may show that it was reasonable for us to have imposed CT in the first place. Not because the later consent removes the force of the earlier refusal to consent, but because it shows us that we may have been right not to place excessive value on the earlier refusal in the first place. (p. 254)
There are two critical points here. First, how one interprets our results is likely to depend on whether one believes that a “reasonable” number of patients changed their views about their need for hospitalization. More than half of the patients who initially judged that they did not need hospitalization revised their beliefs and later reported that they had needed hospital treatment. This was far more than the number of patients who initially judged that they needed hospital care and later said that they did not need it. On the other hand, 61% of those involuntarily committed patients who initially judged that they did not need hospitalization continued to believe that they had not needed it despite their hospital care.
A second point of Wertheimer’s is important here as well. A patient’s retrospective acknowledgment of a need for hospitalization may help justify a coercive admission, but it does not abolish the moral fact that the patient was coerced. Moreover, it does not imply that the patient will forget or forgive the coercion after treatment. On one hand, patients who felt coerced during hospital admission were less likely to revise their views about their need for hospital treatment than were other patients. On the other hand, patients’ perceptions of coercion were stable across the admission and follow-up interviews: we did not see evidence of more positive feelings about the experience. So it may be somewhat misleading to call a retrospective rationale for hospitalization a “thank you” theory—there was not much evidence that coerced patients were later grateful for the experience of hospitalization, even if they concluded that they needed it. We expect that psychiatric patients are similar to the rest of the population in this regard. Many of us can recall ordeals that we were forced to undergo at the hands of people we perceived as unjust, disrespectful, or insensitive. We may well believe that we are stronger, healthier, or wiser for the experience; but are we truly grateful to the person who coerced us?
This suggests that patients’ aversion to commitment is a moral response to the loss of dignity and respect implicit in the deprival of autonomy. Mental health professionals have often justified commitment in terms of its consequences for the patients’ health. However, patients’ retrospective evaluations of these consequences apparently do not change their feelings about coercion. Looking back on their hospitalization, coerced patients are likely to continue to be offended, even if they now view the hospitalization as a necessity.
An important issue for future research concerns why some patients who initially do not view themselves as needing hospitalization later revise their views but others do not. Some patients who judge that they do not need hospitalization may indeed be correct; that is, their hospitalization may have resulted from a clinical error. We had no method for assessing such errors in this study. We did find that, compared with patients who believed that they needed to be hospitalized, patients who believed that they did not need hospitalization tended to perceive that 1) they were treated more coercively, 2) they were subject to forceful and threatening pressures to be admitted, and 3) they were treated with less procedural justice. Some of these patients were presumably coerced into the hospital by staff or family members because they needed but resisted hospitalization. However, it is also possible that some patients developed a resistance to hospitalization because of unnecessarily forceful and insensitive pressure from family members or staff. Further detailed studies of coercion in psychiatric hospital admission would be useful to clarify these processes.