Suicide is the third leading cause of death in younger adolescents in the United States (10–14 years) and the leading cause of death in this age group in other countries such as China, Sweden, Ireland, Australia, and New Zealand
(1) . The enormous human cost of suicide in youth makes research and prevention a national priority. Biological, psychological, social, and cultural factors affect the risk of suicide; however, about 90% of youth suicides in the United States are associated with psychiatric illness
(1 –
3), most commonly a mood disorder
(4 –
9) . There is little difference in depression rates between older and younger teen suicides. Although most seek professional help within 1 month before death
(10), most are not being treated at the time of death
(11 –
14) . Only 2% of youth suicides are receiving medication at the time of suicide
(15,
16) . Poor treatment compliance in youth aggravates the problem. For example, in a study of 49 adolescent suicides in Utah, 24% had been prescribed antidepressants, but
none tested positive for SSRIs at the time of their death
(17) . In a postmortem study of 54 youth suicides
(15), only four had positive serum toxicological analysis for antidepressants within 3 days of death.
Depression annually occurs in 3%–5% of youth and accounts for about 60% of suicides for all ages. Suicide is rare in youth (12-month incidence among ages 15–19: 0.008%
[18] ). However, suicidal thinking or attempts are relatively common. Every year, 19% of teenagers (ages 15–19) have suicidal ideation, and 9% of teenagers make a suicide attempt
(19) . Among youth receiving care for depression, 35%–50% have made, or will make, a suicide attempt
(20 –
22), and 2%–8% will commit suicide in a decade
(20,
21,
23) .
The observation that almost all youth suicides are not taking antidepressants at the time of death, even when thought to be depressed, suggests that lack of treatment contributes to suicide risk, and that more widespread antidepressant treatment may reduce suicide rates
(24) . At the same time, concerns have been raised about the effect of some medications such as SSRIs on the risk of youth suicide. Antidepressants appear to be associated with adverse event reports regarding suicide attempts or ideation, with absolute rates of 0%–2% higher than placebo
(25) . There is a paucity of randomized, controlled clinical trials evaluating the safety and efficacy of any antidepressant medication in depressed subjects at risk for suicide because of a history of suicidal behavior. Tricyclic antidepressants do not appear to be effective in children and adolescents, and data for the efficacy of other types of antidepressants are only convincing for fluoxetine
(26,
27), in part because of unpredictably variable placebo response rates
(24) .
Given the low incidence of suicide, alternative approaches are needed to assess the relationship of antidepressant treatment to suicide. One approach involves large-scale naturalistic studies of at-risk populations, such as those conducted to examine lithium treatment of bipolar illness, which demonstrated reduced suicide rates
(28 –
33) although results varied across studies
(34 –
36) . Valuck et al.
(37) examined data from 24,119 adolescents with a first diagnosis of major depression and with at least 6 months of follow-up data. Treatment with antidepressant medication for at least 6 months reduced the likelihood of a suicide attempt compared with 2 months of treatment, both for single and multiple antidepressant prescriptions
(38) . Treatment with SSRIs, other antidepressants, or combinations of antidepressants resulted in no increased risk in suicide attempts. Simon and colleagues
(39) reported that the period of highest risk for suicidal behavior in depressed adults getting treatment with antidepressants is immediately prior to starting treatment. Thus, three large population studies in adults or adolescents
(37 –
39) have provided evidence consistent with antidepressants reducing risk of suicidal acts and no evidence of an increased risk during the initial treatment phase.
Although a number of epidemiologic studies have identified a negative correlation between antidepressant prescriptions and suicide rates
(40), only one focused on youth (10–19 year olds). Given that the suicide rate is six times higher in older adolescents and approaches adult rates, we decided to examine younger children (5–14 years) where little is known of either SSRI efficacy or safety.
Method
The National Center for Health Statistics of the Centers for Disease Control and Prevention (CDC) maintains the National Vital Statistics
(41) database, which includes suicide rate data. Suicide rates for 1996–1998 were obtained from the CDC for each U.S. county by sex, race, and age. The focus of this analysis is on the 5–14 age group. County-level antidepressant prescription rate data came from a random sample of 20,000 pharmacies (stratified by type, size, and region) from the 36,000 pharmacies in the database of IMS Health (Plymouth Meeting, Pa.), which represents over half of all retail pharmacies in the continental United States. The data do not include hospital prescriptions. For each county, prescription rates (number of pills per county) were obtained for SSRIs (citalopram, paroxetine, fluoxetine, fluvoxamine, and sertraline).
To relate SSRI antidepressant prescriptions to suicide rate adjusting for county-specific case mix (sex, race, and income), we used a mixed-effects Poisson regression model (
1 [Appendix A], 42–45). This model is suitable for rare event data in which the observed number of suicides in a given county may be small (including zero), and the number at risk (i.e., population size) may vary from county to county. The model estimates overall suicide rate conditional on sex, race, income, and antidepressant prescription and can also be used to estimate covariate-adjusted county-specific estimates of suicide rates. In terms of antidepressant drug prescription, we used the natural logarithm of number of pills per person per year to adjust for differential population size of counties and to eliminate excessive influence of counties with extremely high or low antidepressant prescription rates. In the model, sex, race, and income were considered fixed effects, and the intercept and antidepressant SSRI prescription effects were treated as random effects. This model specification allows the suicide rate and the relationship between antidepressants and suicide to vary across counties. As such, we can estimate county-specific changes in suicide rates attributable to changes in SSRI prescriptions, adjusted for the sex and race composition of each county. The effect of policy changes (e.g., adding or eliminating SSRIs) can be estimated by accumulating the county-specific estimates over all counties. To test the possibility that the observed associations are simply due to access to quality health care, we included median county-level income and number of psychiatrists and child psychiatrists in the county as covariates. To break down the overall relationship into within- and between-county components, a model was fitted using the county mean SSRI prescription and yearly deviation from the mean.
Parameters of the models were estimated using the method of Hedeker and Gibbons (
1 [Appendix A], 46). The computer program MIXPREG (www.uic.edu/labs/biostat) was used for these analyses.
Results
We have previously established goodness of fit of the mixed-effects Poisson regression model to the nation’s suicide rates, conditional on age, sex, and race
(40) . In the general population, suicide rate increases with age, is higher in males, and lower in African Americans.
Similar excellent fit of the mixed-effects Poisson regression model was seen for children. The observed number of childhood (ages 5–14) suicides from 1996–1998 was 933 (
Table 1 ), and the estimated rate (based on actual SSRI use) was 836, a difference of 97 (10%) or approximately 32 suicides per year.
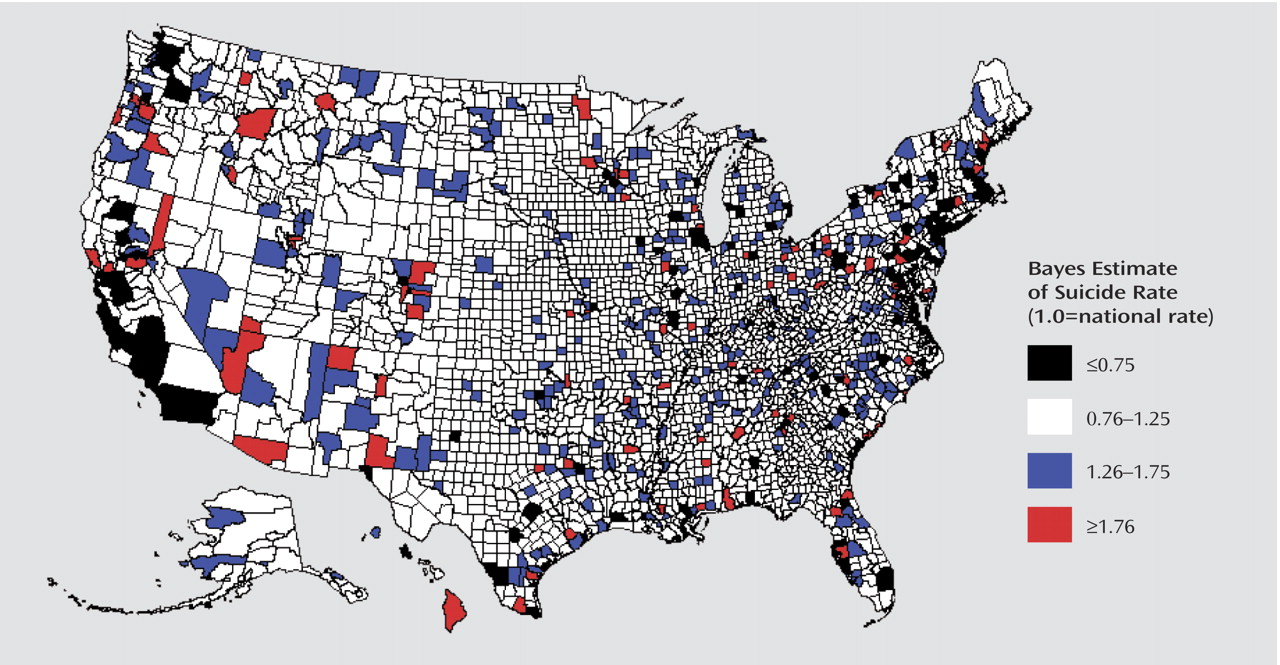
Bayes estimates were obtained of county-level suicide rates adjusted for effects of race and sex (
Figure 1 ). A Bayes estimate of 1.0 represents an adjusted rate equal to the national rate, a Bayes estimate of 2.0 represents a doubling of the national rate, and a Bayes estimate of 0.5 represents half of the national rate. Similar to the adult population, highest adjusted rates were typically found in some of the less densely populated areas of the western United States, such as Arizona, Utah, and Montana, many of which include areas with Indian reservations. For example, Apache County in Arizona includes Hopi Indian reservations, Uintah county in Utah includes Ouray, and Rosebud and Yellowstone counties in Montana include Northern Cheyenne. By contrast, adjusted suicide rates are lowest in the large cities such as Chicago, New York, Boston, Los Angeles, San Diego, Seattle, Miami, and the eastern seaboard in general. There are a few exceptions, such as Laredo, Texas, which has a low adjusted suicide rate. As seen in
Table 2, the overall relationship between prescribed SSRIs and suicide rate was statistically significant (maximum marginal likelihood estimate=–0.17, p<0.004). The negative maximum marginal likelihood estimate indicates that SSRI prescriptions are associated with a decrease in suicide rate.
The average population of children aged 5–14 in 1996–1998 was 38,812,743, and the number of suicides over this 3-year period was 933 (0.8 per 100,000 per year). If there were no SSRI prescriptions, the model estimates 253 more suicides per year (an 81% increase). These effects are apparent in the raw data (
Figure 2 ). For the lowest deciles (low SSRI prescription rate), the overall observed suicide rate is as high as 1.7 per 100,000, whereas for the highest deciles (high SSRI prescription rate) the suicide rate is as low as 0.7 per 100,000.
To control for access to quality mental health care, two additional analyses were performed. First, median income for each county from the 2000 U.S. Census was included as a predictor in the model. While income was inversely related to suicide rate (maximum marginal likelihood estimate=–0.01, p<0.0006), the SSRI effect remained significant (maximum marginal likelihood estimate=–0.12, p<0.04). Second, we adjusted for access to mental health care by including the number of psychiatrists and child psychiatrists per county in the model
(47) . Again, the SSRI effect remained significant (maximum marginal likelihood estimate=–0.14, p<0.02).
Finally, the SSRI effect was broken down into between- and within-county effects. A significant between-county effect was observed as before: namely a negative association between SSRI prescriptions and suicide (maximum marginal likelihood estimate=–0.15, p<0.007). Within-county effects were not significant, indicating that fluctuations in SSRI prescriptions for children over the 3-year time interval within counties were not associated with either increases or decreases in suicide rate.
Discussion
Our analysis revealed that counties with higher rates of SSRI prescriptions had lower rates of suicide in children and young adolescents. We previously found both significant between-county and within-county effects of SSRIs on suicide rate in the general population
(40) . However, in this study of children and young adolescents, we only found a significant between-county SSRI effect. One possible explanation for this finding is that there are far fewer suicides in children, and therefore less power to detect a within-county effect.
Olfson and colleagues
(48) did a similar study in the United States but included an older age range (10–19 years), focused on antidepressants in general (not just SSRIs), and performed cross-sectional analyses of suicide rates in 1990 and 2000 and on the change in suicide rates versus change in prescription rates between the 2 years. Their prescription data were obtained from a different source, for different years, and were based on only 1 month in each of 2 years. We used data from the entire year. Using a fixed-effects linear regression model, they adjusted for race, median income, and physicians per capita. Effects of other variables such as sex and age were examined through stratification. Their cross-sectional analyses revealed a positive association between antidepressant prescriptions and suicide rates. However, they found a negative correlation between changes in antidepressant prescription rates and changes in youth suicide rates between the years 1990 and 2000. Using a quite different methodology (case-mix adjusted random-effects Poisson regression model), a completely independent data set, and focusing on SSRIs in particular, we have demonstrated that this general relationship extends to early adolescents. The difference in our results for the cross-sectional analysis (they found a positive association and we found a negative association) could be due to the fact that they combined all antidepressants and we focused exclusively on SSRIs. The difference in our results for the within-county effect (they found a negative association and we did not find an association) could be due to their use of a two-point difference in rates from 1990 to 2000 (i.e., going from a time of low to high utilization) versus our use of three sequential years of data, where rates of prescriptions of SSRIs fluctuated more modestly.
Our results are consistent with those reporting SSRI efficacy for major depression in children and early teens. Randomized controlled trials have demonstrated efficacy for fluoxetine in children and adolescents, but none have specifically examined the 5–14 year age group, so randomized controlled trials are needed in this age group to test this possibility. One psychological autopsy in adolescents
(49) reported comparable rates of mood disorders in younger adolescent versus older adolescent suicides, but other differences may exist affecting relative efficacy of antidepressants
(2,
49 ε1), including a greater risk of mania with SSRIs
(52,
53), although bipolar disorder is uncommon in youth suicide, with the highest rate reported at 13%
(54) . Other possibilities are 1) the relationship between youth suicide and prescription rates may be due to more use of antidepressants in the depressed parents of depressed children and that improvement in the parent results in improvement in the depressed child or 2) SSRI use for anxiety disorders in children, although psychological autopsies indicate that anxiety disorders are uncommon in suicides
(49,
54 ε8) . Regardless, our findings suggest that the risk benefit ratio in 5–14 years olds may be favorable.
A more conservative conclusion is that our results and those of Olfson et al.
(48) undermine the view that SSRIs cause suicide, which was the concern that arose from the higher frequency of suicide attempt-related adverse events reported with antidepressants relative to placebo among children and adolescents in randomized controlled trials
(24,
59) . It is noteworthy that no difference was observed on suicide-related ratings systematically scored on the depression rating scales
(24,
59), raising a question about an ascertainment bias in the adverse event reports.
Our results are in agreement with pharmaco-epidemiologic studies reporting a decline in suicide attempts and suicide in adults and adolescents prescribed antidepressants
(37 –
39) and with adult national population studies in other countries reporting that a decrease in suicide rate correlated with increased antidepressant use over a period of time
(60 –
65), including two studies that linked the greatest fall in suicide rates to the segment of the population (older men and women) that had the highest exposure to antidepressants
(66 –
69) . Despite the proportion of the outpatient depressed U.S. population receiving at least one antidepressant prescription increasing from 37.3% to 74.5%
(10,
12,
48) from 1978–1997, suicidal behavior correlates with inadequate prescription of antidepressants
(70) .
This study has limitations. Medication estimates were based on outpatient prescriptions and not actual use. There is some uncontrolled variability in the suicide rate data due to regional differences in 1) the definition of suicide; 2) qualifications of the coroner or medical examiner; 3) the extent to which cases are investigated; 4) the relationship between prescription rates and taking of medication, which may be weaker in high-risk groups; and 5) the quality of preparation of official statistics, which can lead to differential underreporting of suicide rates
(1) . Despite this potential variability, strong associations between SSRI prescription rates and suicide rates were observed.
The FDA’s meta-analysis
(71) was based on the synthesis of randomized clinical trials and less subject to bias due to confounding but was based on nonfatal suicide attempts and suicidal ideation (both common in adolescents and children) and only surrogate endpoints
(24,
72) . Our results are based on suicide completion, which is too rare to study in randomized controlled trials. Moreover, randomized clinical trials analyzed by the FDA attempted to exclude subjects at highest suicide risk. The FDA found more suicide-related adverse event reports, retrospectively abstracted from the medical records in the medication groups. However, when comparing an active medication that has side effects with placebo, there may be more expansive medical records for the active treatment subjects and therefore a greater likelihood of reported suicidal thoughts. This type of ascertainment bias is not avoided in randomized studies and may contribute to the difference between our results and the FDA’s results and between the prospective and retrospective results obtained by the FDA.
Our results suggest that availability of psychiatric services and prescription rates of SSRIs are associated with lower suicide rates in very young adolescents and indicate the need for controlled clinical trials to determine the safety and efficacy of antidepressants in major depression in this age group.