The biopsychosocial model was conceptualized as a medical model that allowed for mutual interaction between the biological and the psychosocial aspects of a person’s life
(1) . Modern biological research has elucidated how psychosocial factors influence gene expression
(2) and how psychosocial treatments change brain activity
(3) . More recently, the concept of “the social brain” has been put forward as a unifying model for how the environment shapes brain development
(4) . In these models, the family environment is the most immediate psychosocial milieu. Research on the role of the family environment in both the genesis and the treatment of illnesses has become a significant body of work spread across many medical disciplines. This article examines the current state of family research in psychiatry as well as reviewing relevant studies of family factors in these other medical disciplines.
Examples of Family Research in Medical Practice
Studies from medicine and pediatrics demonstrate the importance of family support in achieving optimal outcome from medical treatment. For example, good marital quality is associated with better outcomes for cardiovascular disease and reduced all-cause mortality, especially for women
(5) . Interview and observational measures of marital quality obtained from 189 patients with congestive heart failure (139 men and 50 women) and their spouses were examined as predictors of patient survival up to 48 months after assessment and compared with predictions based on illness severity (from a New York Heart Association class). Marital quality predicted 4-year survival rates just as well as the patient’s current New York Heart Association class. Similarly, a study of 194 elderly patients hospitalized for acute myocardial infarction found that those with strong emotional support had significantly better outcome at 6 months than patients who lacked social support
(6) . By the end of the first year, 55% of those with no support had died, compared with only 27% of those with two or more social supports. These effects are not limited to cardiac illness. A study of 90 women with stage II and stage III breast carcinoma
(7) showed that dependable social relationships predicted overall survival measured 18 months after diagnosis.
On the other hand, family stress can increase the risk of illness. Women who cared for a disabled or ill spouse for at least 9 hours per week had an increased risk of coronary artery disease
(8) . In a prospective study of 54,412 female registered nurses ages 46 to 71 who did not have diagnosed coronary heart disease, stroke, or cancer at baseline, there were 321 incident cases of coronary heart disease at the 4-year follow-up. The relative risk (RR), defined as the rate of incidence of coronary heart disease among those who provided care divided by the corresponding rate among women who did not provide care, was 1.93 (95% confidence interval [CI]=1.16–3.20) in women who provided care ≥9 hours per week to a disabled or ill spouse, compared with women with no caregiving responsibilities. Of interest, caring for an ill or disabled parent was not associated with an increased risk of coronary heart disease.
Pediatrics has historically had a negative bias toward the study of the family, which was seen as “the breeding ground for somatic complaints”
(9) . Current family research in this discipline, however, ranges from the study of family risk factors to sophisticated studies of effects of family interventions in disease outcome. Researchers at the Joslin Diabetes Center developed a low-cost intervention to reduce family conflict in the management of diabetes in adolescents. One hundred and five children and adolescents, ages 8 to 17 years, who had insulin-dependent diabetes for at least 6 years were randomly assigned to a family-focused teamwork intervention or to standard multidisciplinary diabetes care. Patients in both groups were seen at 3- to 4-month intervals and were followed prospectively for 1 year. The family-focused intervention group was educated on setting goals, informed about identifying tasks regarding diabetes health maintenance, and instructed on effective problem solving in the area of diabetes-related concerns. The intervention emphasized family teamwork, particularly in the area of insulin injections and the measurement of blood glucose. At each visit, one of four modules was implemented: 1) communicating about diabetes, 2) reviewing educational materials pertaining to the disease, 3) encouraging family discussion regarding elevated blood sugar, and 4) facilitating the use of a log to regulate blood sugar levels that were out of range. The outcome was a significant decrease in the expected deterioration and complications from the illness in adolescence
(10) .
Another study from Boston’s Children’s Hospital found improved patient outcome, increased patient and family satisfaction, and decreased health costs when the family is involved in postsurgical care
(11) . Children cried less (>20% of the children reduced to <5% of the children) and required less medication (20%–30% of the children reduced to <5% of the children) when their parents were present and assisted in postoperative pain assessment and management.
A preventive educational-behavioral intervention program called the Creating Opportunities for Parent Empowerment (COPE) program provides support to parents of children who require intensive medical care
(12) . A randomized, controlled trial was conducted with 163 mothers and their 2- to 7-year-old children. Mothers in the experimental (COPE) group participated in a three-phase educational-behavioral intervention program and were compared to control mothers who were administered a control program. The COPE program focused on increasing parents’ knowledge and understanding of the range of behaviors and emotions that young children typically display during and after hospitalization and encouraged direct parent participation in their children’s emotional and physical care. One year after discharge, a significantly higher percentage of children in the control group (25.9%) exhibited clinically significant behavioral symptoms compared with the COPE children (2.3%).
An Institute of Medicine report
(13) summarized family factors that have been shown to influence chronic medical illness and reviewed the family-focused interventions for chronic medical illnesses. The family protective factors that are identified are family closeness, mutuality, connectedness, caregiver coping skills, mutually supportive family relationships, clear family organization, and direct communication about the illness and its management. The family risk factors that are linked to poorer outcome in the management of chronic illness are intrafamilial conflict, criticism and blame, perfectionism and rigidity, delayed family developmental tasks, lack of an extrafamilial support system, and psychological trauma related to diagnosis and treatment. The report points out that family-focused interventions are common in geriatrics and pediatrics, in which the family members play an important role in decision making and in the delivery of care. Many families report that weathering a crisis together makes relationships richer and more loving than they had previously been
(14) .
Family Research in Psychiatry
Twin and adoption studies have been used to identify the biological basis for psychiatric illness. However, this research is also important in identifying environmental and family factors in psychiatric illnesses. In an adoption study of schizophrenia spectrum disorders, Finnish investigators found that adoptees at high genetic risk for schizophrenic spectrum disorders are more sensitive to adverse rearing patterns in their adoptive families compared to adoptees without such risk
(2) . Adopted offspring of mothers with diagnoses of schizophrenia spectrum disorders were compared with adopted offspring of biological mothers without schizophrenia spectrum diagnoses. The family environments of the adoptive parents were evaluated by experienced psychiatrists. In the group with a high genetic risk, there was a significant association between disordered rearing and adoptee diagnosis of schizophrenia spectrum disorder. This influence was not seen in the group with a low genetic risk. Three domains of family functioning were identified as being associated with unhealthy rearing practices: critical/conflictual, constricted, and boundary problems. The authors reported that neither high genetic risk nor dysfunctional family environment alone predicted adoptee illness; rather, genetic risk and the rearing environment had an interactive effect in promoting the emergence of illness or protecting against such an outcome.
An evocative genotype-environment interaction is considered the explanation for the increased harsh and inconsistent behavior and less warmth that adoptive parents display toward adopted adolescents with a diagnosed antisocial or alcoholic biological parent
(15) . The child’s externalizing behavior was identified as one factor that elicits negative parenting
(16) . Parenting behavior directed specifically toward each child in the family also affects symptoms in the children. Almost 60% of the variance in adolescent antisocial behavior and 37% of the variance in depressive symptoms are accounted for by conflictual and negative parental behavior directed specifically at the adolescent. In contrast, when a parent directs harsh, aggressive, explosive, and inconsistent parenting toward the sibling, it has a protective effect on the adolescent, a phenomenon called “sibling barricade”
(17) .
One of the first research measures in family psychiatry is a family construct called “expressed emotion,” which describes the level of criticism, hostility, and emotional overinvolvement in a family
(18) . Although initially developed for patients with schizophrenia and their families, expressed emotion is now studied extensively across the health care spectrum and in many different cultures
(19) . High expressed emotion is a “significant and robust” predictor of relapse in many illnesses
(20), such as schizophrenia
(21), depressive disorders
(22), acute mania
(23), and alcoholism
(24) . Criticalness is one of the essential components of expressed emotion and is associated with the poorest patient outcomes. Relatives who are critical of the patient are more likely to hold patients responsible for their actions rather than the effect of the illness. A relative’s lack of understanding of mental illness is considered to play an important role in the patient’s relapse because it increases criticalness
(25) .
Originally described as a family trait, expressed emotion is now conceptualized as the outcome of a family system. Miklowitz
(26) stated the following:
Consistent with systems views, high-EE [expressed emotion] families have a vulnerability to dysfunction for which the illness serves as a stressor. In turn, the patient has biological and psychological vulnerabilities that are elicited by aversive family interactions. These family interactions are almost certainly stressful for relatives who wish to assist in the patient’s recovery. They also appear to be physiologically compromising for patients. (p. 677)
Miklowitz further suggested that expressed emotion is a fluid process and that family attitudes may evolve during the course of a relative’s illness.
Assessing the family’s level of expressed emotion was originally difficult because the Camberwell Family Instrument took time to administer and some level of training to use
(27) ; therefore, more practical assessments have been sought. For example, predictors of relapse were assessed in a study of 39 patients who had recently been admitted as inpatients for major depression
(22) . Three predictors—expressed emotion, marital distress, and the patient’s perceptions of criticism from a spouse—were significantly associated with 9-month rates of relapse. Expressed emotion and marital distress predicted the same amount of variance in patient outcomes. Perceptions of criticism were assessed on a 10-point Likert scale that asked, “How critical is your family member of you?” This variable accounted for more variance than expressed emotion and the measure of marital distress combined.
Family Environment: Other Aspects
In addition to expressed emotion, other aspects of the family environment have been studied. For example, maladaptive parental behavior is associated with an increased risk for the development of psychiatric disorders among the offspring of parents with and without psychiatric disorders
(28) . In this study, 593 families from upstate New York were studied over two decades. The youths and their mothers were interviewed to assess parental and offspring psychiatric symptoms, parental behavior, and other psychosocial variables. Family assessment included assessment of enforcement of rules, loud arguments between the parents, harsh maternal punishment, parental affection, parental time spent with the child, and poor parental communication with the child. There were effects of the child on the parent and vice versa. Difficult childhood temperament at age 6 was associated with higher levels of maladaptive parental behavior at ages 14 and 16 years. The offsprings’ psychiatric disorders also increased markedly as the number of maladaptive parental behaviors increased, and persistent maladaptive parental behavior was associated with a higher risk in offspring for psychiatric disorders than was episodic maladaptive parental behavior. Maladaptive parental behavior was associated with an increased risk in offspring for anxiety, depression, disruptive personality, and substance use disorders during late adolescence and early adulthood. Maladaptive maternal and paternal behaviors were independently associated with an increased risk in offspring for psychiatric disorders.
Patients with major depression and patients in families with significant family dysfunction have a slower rate of recovery from a major depressive episode
(29,
30) . Family dysfunction was characterized by poor communication, poor problem solving, and the presence of hostility and criticalness. Conversely, good family functioning improves outcomes in major depression
(31) . In a study of 45 inpatients diagnosed with major depression, about 50% of the patients perceived their family functioning at hospitalization to be healthy. These patients were more likely to recover by 12 months than patients with poor family functioning. This was especially significant for three areas of family functioning: the ability to meet practical and emotional needs, the level of interest that family members showed about each other, and the ability to maintain standards of behavior.
Family Interventions
Family-based interventions are the most significant contribution of family research to psychiatric practice. More than 30 randomized clinical trials have demonstrated that family-based interventions reduce rates of relapse, improve recovery of patients, and improve family well-being among participants
(19) . Successful family intervention reduces rates of relapse and improves quality of life for patients with schizophrenia
(32), bipolar disorder
(33), major depression
(34), borderline personality disorder
(35), and alcoholism
(36) .
The first such interventions were family psychoeducational treatment for schizophrenia
(37) . Family psychoeducation is based on the premise that families need to be supported in their care of the mentally ill person. It includes the provision of emotional support, illness education, help with finding resources during periods of crisis, and help with problem-solving skills. Among studies of family psychoeducation for schizophrenia, there is a remarkable consistency of effects on rates of relapse, with minimum reductions of about 50% over the rates for control groups. In 11 of the most rigorous designed and conducted studies, with an average study duration of 19.7 months, the average rate of relapse for the groups receiving family psychoeducation was 27%, compared to the rate for control groups of 64%
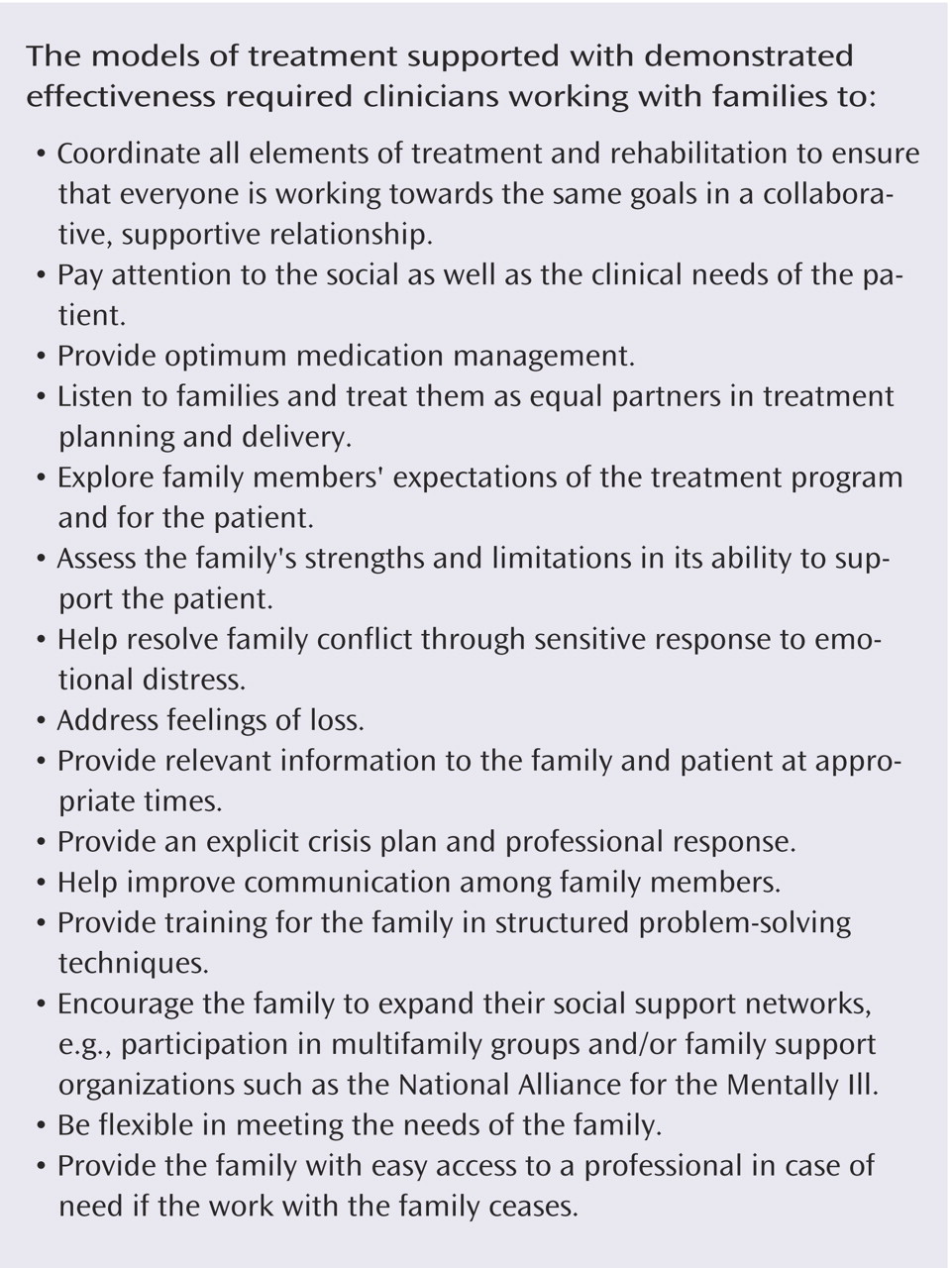
(38) . There are clear principles to be followed in using psychoeducation to successfully work with families, including optimizing medication management and addressing the family’s feelings of loss (
Figure 1 )
(39) .
In bipolar disorder, the results of including family interventions are more varied. A randomized, controlled trial of focused family therapy versus pharmacotherapy alone was conducted among 101 patients with bipolar disorder. Focused family therapy was effective in preventing depressive but not manic relapse
(33) . The patients were assigned to 21 sessions of focused family therapy over 9 months or to a comparison treatment of two family education sessions and crisis management. Both groups received pharmacotherapy. The patients receiving focused family therapy had a significantly better outcome at 1 year (71%) than those receiving crisis management help alone (47%). Another randomized, controlled trial that assigned 92 patients and their families to three treatment conditions—pharmacotherapy alone, pharmacotherapy plus family therapy, and pharmacotherapy plus a multifamily psychoeducational group intervention—failed to find an effect for individual family therapy. The multifamily group treatment consisted of four to six families (including the patients) who met for six sessions with co-therapists focusing on education about the illness and its treatment, coping strategies, and mutual support. The mean number of family therapy sessions was 12, and the number of multifamily group sessions was six. Outcome measures included symptomatic change, recovery status, and family functioning. The proportion of subjects within each treatment group who recovered did not differ.
In major depression, however, the inclusion of a family therapy component led to greater improvement in patients with depression and suicidal ideation than treatment without family therapy
(34) . In this study, 121 patients with major depression who were recently discharged from inpatient care were randomly assigned to one of four treatment conditions that was either “matched” or “mismatched” to their pattern of cognitive distortion and family impairment. The four treatment conditions were 1) pharmacotherapy alone, 2) pharmacotherapy plus cognitive therapy, 3) pharmacotherapy plus family therapy, and 4) pharmacotherapy plus cognitive therapy plus family therapy. Patients who had highly impaired families were “matched” if they received family therapy or “unmatched” if they did not receive this treatment. Matched treatment led to significantly greater proportions of patients who improved than mismatched treatment. Patients receiving family therapy had significantly greater proportions of patients who improved and significant reductions in interviewer-rated depression and suicidal ideation than patients who were treated without family therapy.
For alcoholism, couple’s behavior therapy is effective in reducing alcohol use as well as having positive effects on the spousal relationship, specifically reducing family violence
(36) . Among 303 male alcoholics, 60% of alcoholic patients had been violent toward their female partners in relation to a comparison sample rate of 12%. In the first year after treatment, violence decreased to 24%. For alcoholics in remission, the prevalence of violence dropped to about 12%, nearly identical to the comparison group. The prevalence of violence in the patients who relapsed remained high—30%. The number of days drinking alcohol was correlated with the frequency of violence. Couple’s behavior therapy establishes a daily “sobriety contract” with the patient and spouse in which the patient states his or her intent not to drink or use drugs, and the spouse expresses support for the patient’s efforts to stay abstinent. Couple’s behavior therapy also teaches communication skills and increases positive activities.
In child psychiatry, parent training programs improve parent-child interactions, enhance parenting effectiveness, reduce coercive interactions, and improve internalizing and externalizing problems for children with conduct disorder
(40 –
44) . Parenting interventions and family therapy/psychoeducation are effective for obsessive-compulsive disorder in children and adolescents
(45) . Multifamily groups in the treatment of chronic illness in children, such as bipolar disorder, are also proving effective
(46) . In eating disorders, family treatment that helps parents take an active role with adolescents is most effective
(47), and both family therapy and multifamily psychoeducation group therapy result in weight restoration
(48) .
Implications for Clinical Practice
Improving the family environment has important health implications equivalent to the reduction of risk factors for chronic illness by promoting exercise or a healthy diet. Attention to family resilience offers not just psychiatrists—but physicians in general—new avenues for preventive health care. Patients and families can be given recommendations regarding what constitutes healthy family functioning and referred, if necessary, to workshops or given literature explaining these concepts. Offering early family intervention, such as psychoeducational workshops, is preventative, not just crisis management.
In general psychiatric practice, patients and families can be informed about the role of family factors in the treatment of major mental illnesses and encouraged to seek psychoeducation and support groups. For example, psychiatrists can encourage patients with major depression and their families to obtain family assessment to improve any areas of family functioning that are problematic. The treating psychiatrist can provide this service or refer the family to a family therapist. Such referrals are common for many serious medical illnesses, and it is paradoxical that they are not offered for most major mental illnesses. Family interventions may be overlooked because the psychiatrist may not be familiar with the family research literature. Furthermore, the health care system is structured for individuals, not families. However, in the rest of medicine, family therapists are increasingly becoming part of the medical team in specialties such as rehabilitation, oncology, cardiac rehabilitation, and geriatrics to help bridge the gap between the medical profession and the family’s needs
(49 –
51) .
APA has recognized the importance of family research and includes effective family treatments in its practice guidelines, most notably the practice guideline for schizophrenia
(52) . This guideline states the following:
On the basis of the evidence, persons with schizophrenia and their families who have ongoing contact with each other should be offered a family intervention, the key elements of which include a duration of at least 9 months, illness education, crisis intervention, emotional support, and training in how to cope with illness symptoms and related problems.
The practice guideline for bipolar disorder
(53) and the guideline for major depression
(54) also recommend early family involvement and present the known findings about the efficacy of family-based interventions. Practice guidelines for other disorders, such as panic disorder, eating disorders, and substance abuse disorders, similarly recommend early involvement of the family and provide evidence for the efficacy of marital or family therapy as psychosocial interventions.
When families are asked about what they would like from the mental health system, they state that they do not want lengthy intensive interventions but family care that focuses on building rapport and communication
(55) . Families take issue with poor-quality care, conflict with health professionals about treatment alternatives, and lack of a role for families in the treatment. African American families also identified isolation of their communities from the mental health care system. Family members themselves have attempted to bridge the gap between family research and clinical practice by establishing family- and peer-based education programs such as the Family-to-Family Education Program, sponsored by the National Alliance for the Mentally Ill
(56) .
There still exist substantial barriers to the implementation of family research in psychiatry. First, there needs to be a wider dissemination of family research findings in journals that are easily accessible to psychiatrists, with greater discussion about the complexity of the etiology and treatment of psychiatric illnesses. Second, an organizational commitment through state, hospital, and managed care systems must be made to allow families to more easily participate in the health care system. Psychiatrists need to plan for and advocate for these interventions in the systems of care that they lead. Third, the commitment of monies for preventative care in mental health can help initiate the widespread use of family research findings to benefit our patients and their families.