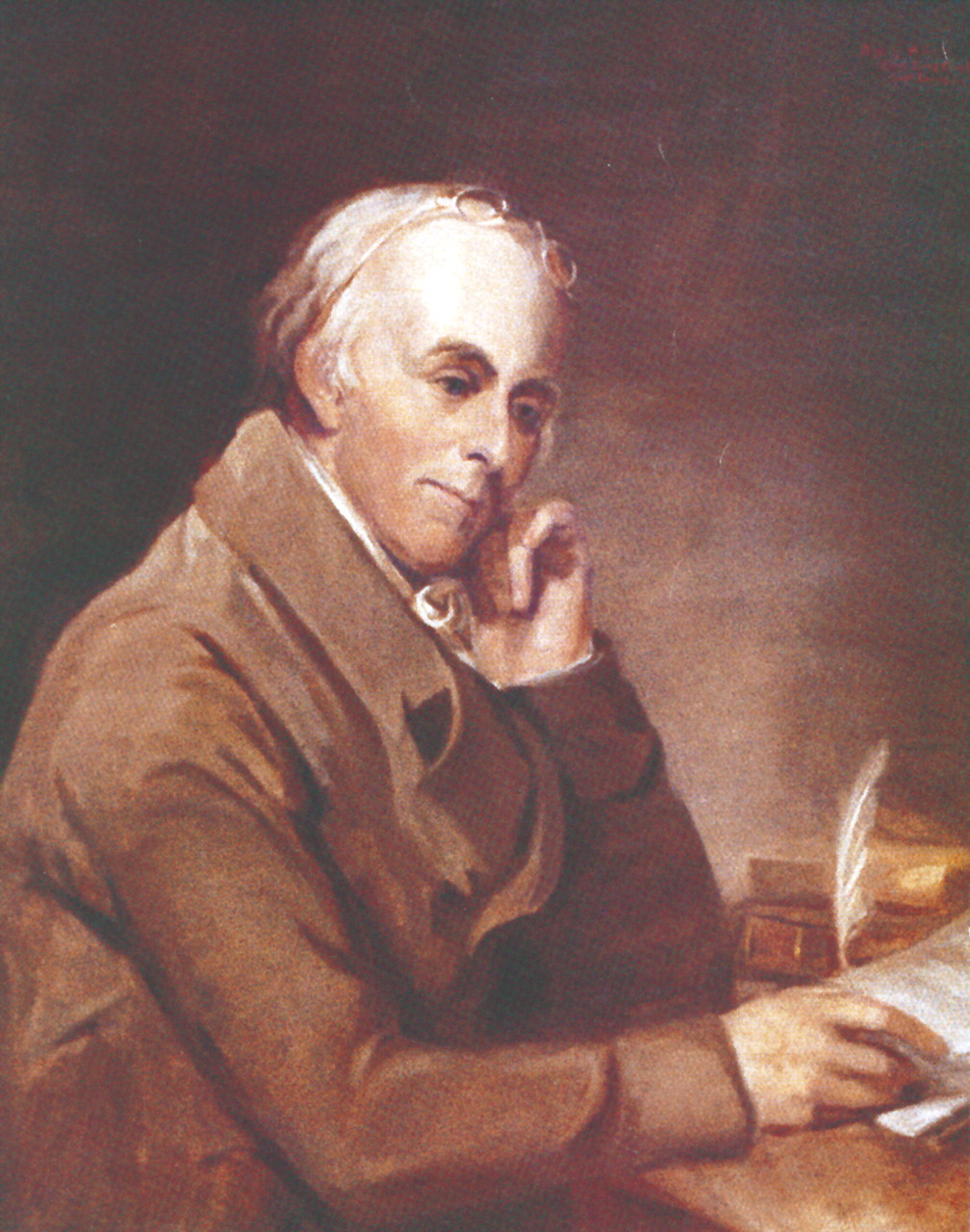
Benjamin Rush, whose silhouette graces the seal of APA, was an extraordinary American by any standard. A member of Congress, he signed the Declaration of Independence; a member of the Philadelphia delegation, he voted to adopt the Constitution of the United States
(1) . He became physician general in George Washington’s army in 1777 in the hope of “being useful to my country” but resigned less than a year later when his protest against the overcrowding and understaffing of hospitals was ignored. Rush was an uncommonly well-educated American physician for his time. He had earned a university degree in medicine from the University of Edinburgh, Scotland, in 1768, whereas most colonial doctors learned their trade by apprenticeship. He became professor of chemistry at the Philadelphia College of Medicine, the first medical school in the colonies, now the University of Pennsylvania, and was promoted to professor of the theory and practice of medicine in 1789. In 1812, the year before his death, he published
Medical Inquiries and Observations Upon the Diseases of the Mind (2), the first American textbook of psychiatry, hence his silhouette on our seal. The failings of this thoroughly estimable man are as instructive as his virtues.
In 1793, the city of Philadelphia was beset by an epidemic of yellow fever
(3) . Philadelphia was the medical capital of the new republic, its physicians the best to be had, but the medical science of the time provided no sure grounds to distinguish between competing theories of cause
(4,
5) . It would be more than another century before the mosquito was identified as the vector of yellow fever and a filterable virus as its agent.
More than one-third of Philadelphia’s population of 50,000 fled the city to take refuge in the surrounding countryside; before the plague was over, more than 4,000 lives had been lost
(3) . Panic beset the community, and doctors were among those who took flight to escape the pestilence. Ten of those who remained died of the disease. After illness and defection, only three physicians were available to treat no fewer than 6,000 cases. Rush, after dispatching his wife and children to a safe area, remained to fulfill his medical responsibilities
(6) .
Rush was an adherent of the Brunonian system of medicine, according to which febrile illnesses resulted from an excess of stimulation and a corresponding excitement of the blood. He ministered to his patients by vigorously bleeding and purging, the latter to “divert the force of the fever to [the bowels], and thereby save the liver and brains from a fatal and dangerous congestion”
(6) . He followed Shippen’s dictum that “desperate diseases require desperate remedies” (
6, p. 442). His desperate remedies, some of his colleagues alleged, were more dangerous than the disease. His convictions were steadfast and were applied to himself no less than to his patients. In his diary, he wrote the following:
On the 9th of October…toward evening, I was seized with a pain in the back….About 12:00, I awoke with a chilly fit. A violent fever followed. At 1:00, I called for Mr. Fisher [his pupil]….He bled me plentifully and gave me a dose of the mercurial medicine….In the morning, the medicine operated kindly, and my fever abated. In the afternoon, it returned….Mr. Fisher bled me again….The next day, the fever left me, but in so weak a state that I awoke two successive nights with a faintness which threatened the extinction of my life….My convalescence was extremely slow. (
6, p. 441)
Rush’s recovery confirmed his conviction that his methods were correct. As the epidemic subsided, he wrote, “Never before did I experience such sublime joy as I now felt on contemplating the success of my remedies….The conquest of a formidable disease was through the triumph of a principle in medicine” (
6, p. 442).
Neither the best education to be had in his day, nor dedication so great that he risked his life to minister to others, nor employing the same remedies on himself when he became ill was sufficient to prevent Rush from committing grievous harm in the name of doing good. Convinced of the correctness of his theory of medicine and lacking means for the systematic study of treatment outcomes, he attributed each new instance of improvement to the efficacy of his treatment and each new death in spite of it to the severity of the disease. I tell this story of Rush’s furor therapeuticus as a cautionary tale. Sympathy for the afflicted and service at personal risk do not ensure good outcomes. Conviction must be tempered by awareness of fallibility.
Drug Discovery by Serendipity
During the first half of the 20th century, psychiatric teaching and practice were entirely occupied with psychoanalytically oriented psychotherapy to overcome the putative poor parenting that was thought to be responsible for mental disorders. This therapeutic furor was replaced in short order by an equally single-minded commitment to biological psychiatry that continues to occupy our profession to this day. Our current psychotropic drugs and the new biological psychiatry that they have engendered arose from a series of chance discoveries: reserpine’s psychotropic effects when it was used to treat high blood pressure, the use of chlorpromazine as a tranquilizer during research on anesthesia, iproniazid as a euphoriant during the treatment of tuberculosis, the antidepressant properties of imipramine when it was employed as a presumptive antipsychotic, and the antimanic effects of lithium when its urate salt sedated experimental animals. The therapeutic effectiveness of these medicines was established by the newly introduced double-blind, randomized clinical trial. Because the new agents seemed to be relatively syndrome specific, diagnosis and classification suddenly became important for clinical management
(7) . Psychiatrists awakened from their overreliance on psychodynamic explanations for schizophrenia to rediscover their medical roots. It became convenient to emphasize licensure for those writing prescriptions; that ability provided an edge in marketplace competition with psychologists and social workers, an edge psychologists are now contesting.
The new medications were given entire credit for the greatly shortened lengths of hospital stays and the successful ambulatory management of psychotic patients. We had failed to understand that the depersonalized and dehumanized mental hospitals had themselves superimposed a “social breakdown syndrome” on the psychiatric disorder that led to the initial admission
(8) . Michael Shepherd and his colleagues
(9) reexamined patient movement in a Buckinghamshire County catchment area of the United Kingdom during two epochs, 1931–1933 and 1945–1947, well before the introduction of drugs. They demonstrated that shorter stays and higher discharge rates were evident a decade before the drugs made their appearance. The change resulted from the introduction of a socially progressive mental health policy: the open hospital and community services. Under those circumstances, the drugs added relatively little. Psychotropic drugs brought relatively little change in hospitals where discharge rates were high before drug use but led to considerable improvements where predrug discharge rates had been low
(10) . Nonetheless, policy and practice stressed drug compliance to the exclusion of almost all other interventions.
Although chlorpromazine, the prototypical first-generation antipsychotic, was unequivocally more effective than placebo or psychotherapy in relieving acute symptoms of schizophrenia and preventing their recurrence, limits to effectiveness and problems with side effects led to a search for “second-generation antipsychotics,” which were greeted with as much enthusiasm as their predecessors and are now shown to be marginally, if at all, superior
(11,
12,
13) and far more costly
(14,
15) . What is striking is the disparity between the early results, albeit hyped by the pharmaceutical industry, and our willingness to switch almost every patient to these new drugs
(16,
17) . The sobering data from current trials, it is hoped, will have provided a brake on this therapeutic enthusiasm.
The
furor therapeuticus for drug treatment has included my own subspecialty, child psychiatry. When my professional career began, what is now known as attention deficit hyperactivity disorder (ADHD) was labeled “hyperkinetic behavior disorder” or “minimal brain dysfunction.” There was one symptomatic treatment: dextroamphetamine. Our Hopkins research group received the first National Institute of Mental Health grant for randomized, double-blind trials of psychotropic drugs in children
(18) ; we documented the efficacy of stimulants for the treatment of hyperkinesis
(19 –
21) . Use of stimulants has exploded in the decades that followed. Although at the 1967 World Health Organization International Seminar on Diagnosis and Classification in Child Psychiatry
(22) Michael Rutter and I had to argue forcefully for the inclusion of “hyperkinetic syndrome” as an entity, current psychiatric drug prescription data for 2005, based on an analysis by Medco Health Solutions
(23), lists 3.6 million children (under age 19) as taking at least one drug for ADHD, with 28% of those children taking two or more. Does this reflect an epidemic of ADHD or an epidemic of diagnostic and therapeutic fashion?
APA meetings are permeated by pharmaceutical companies’ effective marketing. Our enthusiasm for biological psychiatry leads to prescribing the latest drugs, which are also the most expensive and most heavily marketed. Attendees can enjoy three free meals each day by attending sessions sponsored by pharmaceutical companies and “earn” continuing medical education credits (CME), to boot, for sitting through lectures. Although the talks are nominally certified as nonbiased by APA CME regulations, lecturers all too often use company slides, elegantly produced (and subtly slanted). APA has become increasingly dependent on drug company support for its annual meetings through sponsored lectures, rental space for commercial displays, and subsidy of travel expenses and registration fees for foreign psychiatrists.
Conclusion
Since World War II, psychiatry has undergone wild swings in prevailing opinion
(24), from an evidence-free faith in the miracles of psychodynamic psychotherapy to an uncritical belief in the wonders of psychopharmacology (as though patients no longer needed to be listened to), from dismissal of the brain in favor of the mind to a dismissal of mind in favor of the brain (as though they were not inextricably intertwined), from refusal to countenance genetics to worship at its altar (as if there were genes “for” schizophrenia or “for” depression). As an antidote to
furor therapeuticus, it is essential that we not forget Sir Aubrey Lewis’s admonition:
The philosophers thought it proper to put not one but two mottoes on the Temple at Delphi: one, the better remembered, was “Know Thyself”: but the second, equally imperative, enjoined “Nothing in Excess.” It might be worth inscribing that over the Temple of Psychiatry.
(25)