Pneumocephalus, also known as pneumatocele or intracranial aerocele, is the presence of air in the intracranial space. The most frequent cause is trauma, but there are many other etiological factors, such as surgical procedures, iatrogenic causes, and tumors (
1). A vast majority of cases present asymptomatically; however, symptoms can include nausea, vomiting, confusion, dizziness, seizures, and rare cases of cranial nerve palsy, delirium, and cognitive impairment (
2).
The management of pneumocephalus is usually conservative: elevation of the head and abstinence from maneuvers that cause an increase in intrasinus pressure, such as sneezing, coughing, and the Valsalva maneuver. Pneumocephalus usually resolves after 1 week, and surgical intervention is not required unless complications arise (
3).
To our knowledge, there has been no known reported case of cognitive impairment and psychosis due to the presence of pneumocephalus, as reported in this case presentation. This case illustrates the unusual neuropsychiatric sequelae after various neurosurgical interventions.
Case
Mr. B is a 67-year-old Caucasian male with a history of hypertension, hyperlipidemia, asymptomatic atrial fibrillation, diabetes mellitus type II (non–insulin dependent), and chronic back pain. Of note, he had a pertinent surgical history of intrathecal morphine pump placement 3 months before the acute presentation to manage chronic back pain and then removal due to infection approximately 4 weeks before presentation. His psychiatric, social, and family history were noncontributory to the acute presentation.
Mr. B presented to the hospital via ambulance, with a 1-week history of confusion, agitation, and transient psychosis. On presentation, he was alert and oriented to person and place only, with a minimal recollection of the events that brought him to the hospital. He stated, “That nurse is part of the FBI and is here to take me in.” Delirium was suspected; however, there were no fluctuations in mentation noted. As per collateral information, 3 weeks prior to the presentation, he lived independently and performed activities of daily living.
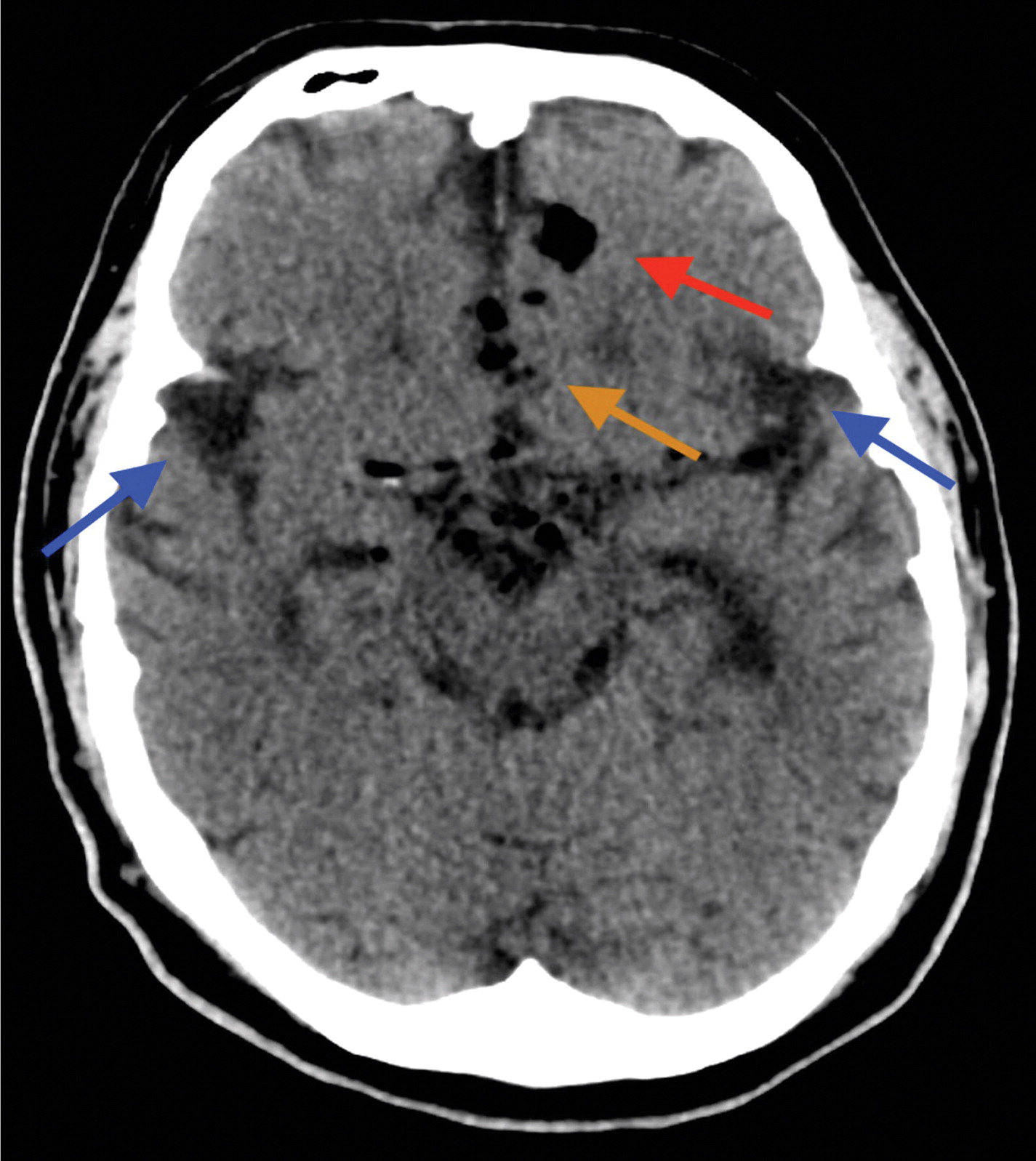
Mr. B’s vital signs, hematologic and biochemical panels, urinalysis, and urine toxicology were within normal limits. The physical exam was unremarkable. High-resolution computerized tomography (CT) of the brain showed multiple areas of intraparenchymal pneumocephalus, with air recognized within the ventricular system bilaterally, the circle of Willis, left frontal lobe, interhemispheric fissure, and temporal fossa bilaterally (
Figure 1). In comparison, a brain CT obtained postsurgery was unremarkable.
Mr. B was admitted to the medical service for further management and resumed home medications. The psychiatric consultation-liaison team was requested to manage ongoing psychosis and behavioral disturbances. On further assessment, he underwent the Montreal Cognitive Assessment (MoCA) and scored a 12/30, suggestive of severe neurologic deficits in executive functioning, working memory, and recall (
4). Additionally, he continued to display new-onset paranoid delusions, which included, but were not limited to, accusing hospital staff of being part of law enforcement.
New-onset psychosis was managed with divalproex sodium (delayed-release) 250 mg by mouth twice daily and haloperidol 5 mg by mouth at bedtime. This combination was started to address irritability, agitation, and delusions. Divalproex level on day 3 was 30.3 mcg per ml. The patient was monitored with serial MoCA assessments throughout hospitalization, which continued to reflect severe neurologic deficits in executive functioning, working memory, and recall, with no significant improvement (
4). One month later, a repeat brain CT showed persistent pneumocephalus, with the continued presence of cognitive deficits. However, the psychosis and mood symptoms, which included paranoid delusions and irritability, were well managed with the continuation of the haloperidol and divalproex regimen. The patient was unfortunately lost to follow-up after discharge.
Discussion
The etiology of new-onset psychosis with cognitive impairment can be related to several factors, including illicit substances, general medication sequelae, and primary psychiatric illness. Mr. B’s medication regimen was thoroughly reviewed for possible neuropsychiatric side effects but was unremarkable. Medications commonly associated with psychiatric side effects include isotretinoin, interferons, corticosteroids, metronidazole, anabolic steroids, and beta-blockers (
5). In addition, other known causes of neurocognitive disorders, such as vascular dementia, Alzheimer’s dementia, Lewy body dementia, frontotemporal dementia, and encephalitis (
6), were considered but did not fit his clinical presentation. Dementia usually presents as chronic and gradual as opposed to the rapid decline with an inciting event noted in this presentation.
On initial review of his medical records and examination, we suspected that the psychiatric symptoms and neuroimaging findings could be due to neurosurgical complications from the placement and removal of the morphine pump. Comprehensive studies have reported that complications of intrathecal pumps can be categorized into mechanical, surgical, and medical. Medical complications include edema and infections, most notably methicillin-resistant
Staphylococcus aureus (
7). Surgical complications include neurological injury, cerebral spinal leaks, and malpositioned subcutaneous pockets. Neurological complications that can arise from intrathecal morphine pump placement and removal include spinal cord injuries, myelopathies, and dysesthesias’ damage to nerve roots resulting in pain, sensory loss, or weakness (
8). Other rare complications include intraparenchymal injury and progressive necrotic myelopathy in a reported case. Neuropsychiatric complications can occur later, as evident in this case presentation of pneumocephalus after a week (
9). Therefore, clinicians should obtain serial head and spinal CT or MRI scans to check for neurological or psychiatric sequelae.
Mr. B had episodes of agitation throughout hospitalization. Several case reports have suggested that agitation can occur in some patients with pneumocephalus, especially if present in the frontal lobe region. A prospective cohort study indicated that bifrontal pneumocephalus was an independent risk factor for postoperative agitation. The frontal lobe involves emotion and cognition; air in this region may result in abrupt changes in behavior, including agitation. This hypothesis requires further research, because it is only a presumptive mechanism (
10). New-onset psychosis and agitation were managed effectively with divalproex and haloperidol. Extensive studies have shown that haloperidol can treat acute psychosis and has proven efficacy for agitation. However, studies have shown that a combination of divalproex and an antipsychotic produce quicker initial resolution of psychotic symptoms, compared with monotherapy (
11).
Unfortunately, the patient’s severe cognitive impairment showed no improvement, and there were concerns about the long-term ramifications. Cognitive dysfunction is usually associated with morphological changes within the cortex. A study found that aging, combined with lesions to the frontal lobe, affects the ability to complete executive tasks (
6). Compared with healthy controls, patients with frontal lesions performed poorer on tests of executive functions (
12). In addition, lesions in the temporal lobe would likely present with dementia-like symptoms affecting memory. Studies in Alzheimer’s groups found that reduced connectivity networks in the temporal lobes and the subcortical regions were associated with rapid memory decline, poor memory performance, and emotional dysregulation (
13).
Furthermore, the location of the pneumocephalus could also have another random effect on the brain morphology, disrupting the dopamine pathways that transcend the prefrontal cortex and midbrain. This effect is illustrated clinically with the presence of new-onset psychotic symptoms (
14). However, these are speculative mechanisms and require further investigation.
We believe that neurocognitive decline and psychosis were secondary to pneumocephalus in this case (
Figure 1). The most likely etiology was iatrogenic, resulting from the placement and removal of the epidural morphine pump for back pain management. Although an overwhelming majority of pneumocephalus resolves within a week, if symptoms persist, we speculate that pneumocephalus can cause transient psychosis and contribute to long-term cognitive impairment, which may be irreversible, as in this presentation (
2).
A limitation is that no presurgical formal testing was available for comparison. We recommend that psychiatrists and primary care providers obtain neurological imaging or serial cognitive assessments after neurosurgical interventions, especially when psychosis or sudden cognitive impairments are apparent.
Conclusions
The combination of pneumocephalus, cognitive impairment, and new-onset psychosis is exceedingly rare. To our knowledge, this is the only case report that indicates such a presentation. Sudden cognitive deterioration is undoubtedly an ominous sign, and if not resolved quickly, pneumocephalus can have long-lasting deleterious effects on the quality of life. Besides the presence of air causing an effect within the brain parenchyma, one needs to consider whether an inflammatory process is present. It is unclear how pneumocephalus alters the brain morphology or has an overall impact that leads to this clinical presentation. In this case, the diffuse nature of the pneumocephalus and the involvement of the frontal lobe, temporal lobe, and interhemispheric fissure were associated with alterations in the patient’s behavior and cognitive function.