Here, we present a case exemplifying the diagnostic challenges of identifying OCD in a patient who presented with a history of psychotic symptoms and polysubstance use. This case also demonstrates the importance of maintaining a high suspicion for OCD among patients with less apparent compulsions and the presence of psychotic features.
Case Presentation
A 21-year-old male patient with a history notable for attention-deficit hyperactivity disorder, multiple substance use disorders, and psychosis was admitted from his psychiatrist’s outpatient office because of concerns of decompensated psychosis. He reported excessive time spent ruminating over traumatic vivid thoughts, difficulty sleeping, difficulty concentrating, low energy, poor appetite, and suicidal thoughts without a plan. His intrusive thoughts were centered around “false memories” stemming from a night of heavy alcohol consumption with his friends that took place about one year before admission. He was concerned about the possibility of having sexually violated women while being intoxicated. He stated that he repeatedly shared these concerns with his friends, who reassured him that the events did not actually take place. These thoughts occurred constantly for several months and acutely worsened during the weeks preceding admission, causing him to sleep for a maximum of 3–4 hours each night compared with his baseline of 6 hours.
The patient had been hospitalized twice and received care at an intensive outpatient program during the previous year because of similar symptoms. A psychiatrist at an outpatient facility suspected that he had bipolar disorder because of signs of distractibility, disturbed sleep, increased goal-directed behavior, and psychomotor agitation. Additionally, he had a history of substance use disorders involving alcohol use since the age of 16, with an average consumption of 14 drinks per week, daily cannabis use, and tobacco use exceeding 100 pulls from a vaporizer daily. His current medications were extended-release divalproex (750 mg) as a mood stabilizer and quetiapine (50 mg nightly) for insomnia. He was previously treated with ziprasidone for unspecified psychosis (although this was discontinued when he was reconceptualized as having bipolar disorder), aripiprazole for unspecified psychosis (but this was discontinued because of akathisia), and escitalopram for depression (but this was discontinued because of concern for acute mania). He had no history of suicide attempts or self-injurious behavior.
The patient exhibited severe disorganization on initial examination. He frequently stopped speaking, gazed into the distance, and remained unresponsive for periods of 10–20 seconds. He was aware of these interruptions and attributed them to anxious ruminations. His thought content included ruminations that he had sexually violated women one night when he was intoxicated. During subsequent interviews, his ruminations about that night included having legal concerns, making homophobic remarks, engaging in conflicts with a friend, and displaying generally aggressive behavior. Additionally, he displayed psychomotor agitation, characterized by constant fidgeting, playing with his hair, pacing the room, and picking at his clothes.
On the basis of his disorganized thought process and behavior, along with his false memories that were initially thought to represent delusions, the leading diagnosis was substance-induced psychosis. This diagnosis was supported by his history of significant alcohol, nicotine, and marijuana use. Bipolar disorder with psychotic features was also considered based on his decreased sleep, distractibility, and racing thoughts. However, the patient was lacking other key features, such as elevated mood or increased energy. The differential diagnosis also included a schizophrenia spectrum illness (schizophrenia vs. schizoaffective disorder vs. schizotypal personality disorder), as well as reconsideration of a major depressive episode with psychotic features (
2). His examination and laboratory findings were not suggestive of psychosis secondary to a toxic, metabolic, or structural cause. His valproic acid level was subtherapeutic at 25.2
µg/mL.
His divalproex regimen was uptitrated to 1,250 mg daily, and he was started on risperidone that was uptitrated to 3 mg daily, with no improvement in symptoms. As his hospital course progressed, his intrusive, time-consuming, distressing thoughts became better characterized as obsessions. For instance, the themes of aggression, sexual content, and harm to others were more consistent with ruminative symptoms of OCD than the persecutory, referential, somatic, erotomaniac, and grandiose themes commonly associated with delusions (
1). Additionally, his level of anxiety regarding these thoughts was more aligned with obsessions than the paranoia typically associated with delusions (
3). As commonly seen in OCD, he perceived these obsessions as originating from his own thinking, contrary to individuals with psychosis, who often believe external factors influence their thoughts (
4). Overall, he had fair insight that these thoughts were not real. Finally, the patient engaged in behaviors that can be understood as mental compulsions, such as repeatedly seeking reassurance from friends, reviewing memories to alleviate doubts that he harmed others, or trying to suppress these thoughts. He was administered the Yale-Brown Obsessive Compulsive Scale (Y-BOC), which indicated severe symptoms (obsession subtotal score: 14; compulsive subtotal score: 15; total score: 29) (
5).
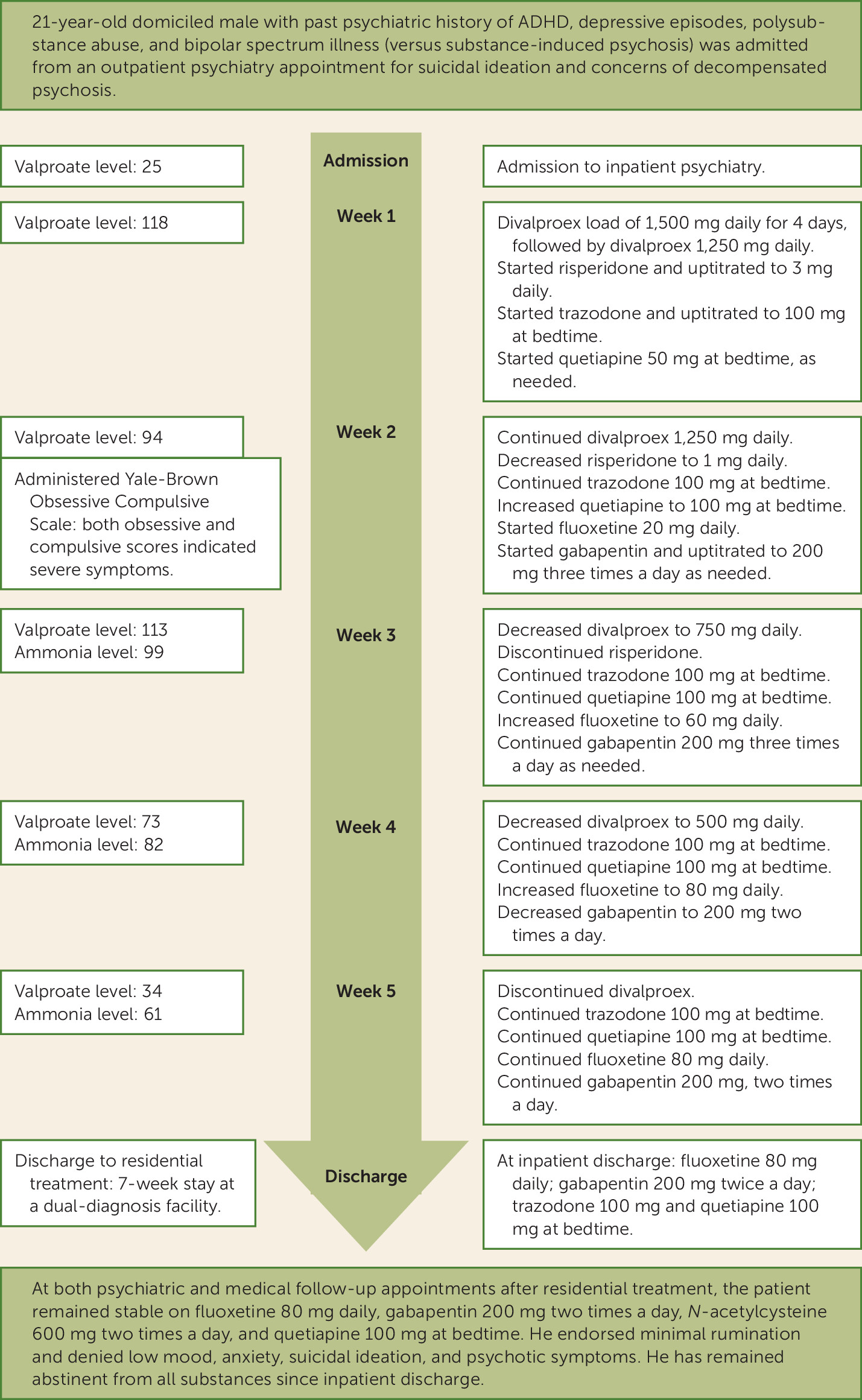
As his diagnosis shifted from bipolar spectrum disorder with psychotic features and substance-induced psychosis toward OCD, his risperidone was slowly discontinued. Divalproex was ultimately discontinued because of a lack of improvement complicated by rising ammonia levels. There was no evidence of emerging mania after divalproex was stopped. He began treatment with fluoxetine, which was gradually increased to 80 mg daily, with improvement in symptoms. He was also started on gabapentin (200 mg twice daily) to treat his anxiety and alcohol use disorder.
By the end of the patient’s 36-day admission, his thoughts became more organized, and he no longer exhibited signs of psychosis. Per the patient’s report, the frequency of his obsessions decreased, and he was able to dismiss them more easily. Furthermore, he was able to actively participate in group activities and sustain attention. On discharge examination, he displayed cooperation, maintained good eye contact, and did not exhibit psychomotor agitation, and his speech appeared normal. His thought process was logical and linear, and he reported a positive mood. There was no evidence of suicidal intent. He was discharged to a dual-diagnosis residential treatment facility where he stayed for 7 weeks. While at this facility, he was started on
N-acetylcysteine, which has been shown to have positive preliminary findings in the treatment of cannabis use disorder and OCD (
6). Since then, he continues to exhibit positive clinical progress, with no signs of psychosis and the ability to manage intrusive thoughts. The patient’s full clinical presentation and course are summarized in
Figure 1.
Discussion
In this case report, we described the challenging diagnosis of OCD with fair insight in a patient who exhibited psychotic features in the context of polysubstance abuse. The complexity of this case is evident in the patient’s lack of improvement despite multiple hospitalizations and medication trials, necessitating extensive investigation to reconceptualize his psychosis as OCD. One of the primary difficulties stemmed from the patient’s “false memories” and whether they should be characterized as intrusive thoughts or delusions. Additionally, his ruminations resulted in frequent interruptions during examinations, which appeared to be consistent with internal preoccupation and thought blocking associated with psychosis, complicating the diagnostic picture.
Previous studies have demonstrated that uncertainty regarding one’s memories may influence OCD symptom severity (
7). For instance, the lack of confidence in one’s memories may lead a patient to experience constant anxiety or a sense of incompleteness, which can trigger compulsive rituals such as checking, seeking reassurance, or mental reconstruction of events (
8). This pattern aligns with our patient’s behavior because he frequently spoke with friends and mentally replayed events to reassure himself that they did not happen. In contrast, patients with delusions more often hold strong conviction about false beliefs despite contradictory evidence. Additionally, the prevalence of substance use disorder is significantly higher among men with OCD than among men with other psychiatric disorders (
9,
10).
Distinguishing between OCD symptoms and psychotic symptoms can pose challenges in certain cases. For instance, both obsessions and delusions involve persistent and distressing thoughts that are hard to manage. However, there are important distinctions to consider, including differences in insight and content as well as whether the individual believes that the thoughts are true. Additionally, when a patient is preoccupied with mental compulsions, it can be challenging to distinguish these from symptoms of a thought disorder, such as thought blocking (
11). There are several conditions that demonstrate overlapping psychotic and OCD features, such as schizo-obsessive disorder (
12), OCD with poor insight, schizophrenia with antipsychotic-induced obsessive-compulsive symptoms, and OCD with prodromal schizophrenia (
13). Such overlapping features can complicate diagnosis because patients may not exhibit distinct symptoms that distinguish one diagnosis from another. Acute substance intoxication or withdrawal may further induce debilitating anxiety with severe disorganization that interferes with diagnostic clarity.