Affective disorder and alcoholism are each highly associated with attempted suicide
(1,
2). A few studies have looked at the impact of the comorbidity of bipolar disorder and alcoholism on the risk of suicidal behavior. Two studies have found a significantly increased rate of attempted suicide in subjects with bipolar disorder and comorbid substance use disorders, including alcohol abuse and illicit substance abuse
(3,
4). Morrison
(5), studying inpatients with bipolar disorder, observed more suicide attempters among the alcoholics than among the nonalcoholics, but this difference did not reach statistical significance. Understanding the relationship between bipolar disorder, alcoholism, and attempted suicide has important clinical implications and, if the relationship is familial, might have etiologic implications as well. A familial relationship was suggested by a study that found a higher percentage of subjects with a family history of suicide among those with bipolar disorder and comorbid alcoholism than among those with bipolar disorder alone
(6).
We report here an analysis of suicide attempts, affective disorder, and alcoholism in a family sample ascertained for a genetic study of bipolar I disorder. We hypothesized that subjects with affective disorder and comorbid alcoholism would have higher rates of attempted suicide than those without this comorbidity. We also hypothesized that the co-occurrence of alcoholism and attempted suicide would be familial.
Method
Aspects of family ascertainment are described in detail in an earlier publication
(7). Study subjects were members of 71 families ascertained for a genetic linkage study of bipolar I disorder. After a complete description of the study to the subjects, written informed consent was obtained. All available first- and second-degree relatives, as well as the probands with bipolar I disorder themselves (a total of 337 subjects) were interviewed by psychiatrists using the Schedule for Affective Disorders and Schizophrenia—Lifetime Version
(8). Affective disorder diagnoses according to Research Diagnostic Criteria
(9) were made with a best-estimate procedure that used data from medical records and interviews with subjects and family informants. Lifetime diagnoses of alcoholism were made on the basis of direct subject interview and family informant data. A history of attempted suicide was determined from direct subject interview.
Pearson’s chi-square and Fisher’s exact tests were used to test group differences in history of attempted suicide. Logistic regression was performed to control for the effects of sex and age at interview. An analysis was performed with the generalized estimating equation approach
(10), which uses logistic regression but also takes into account potential correlation between observations when multiple members of the same family are considered. Tarone’s one-sided score test for binomial distributions was employed to assess within-family clustering of attempted suicide in alcoholics with bipolar disorder (including probands and first-degree relatives)
(11). A further comparison to assess familiality was made between first-degree relatives of two proband groups: 1) probands who were alcoholic and had a history of attempted suicide and 2) all other probands.
Results
Subjects with comorbid alcoholism and a major affective disorder had a 31.7% (40 of 126) lifetime rate of attempted suicide, compared to 17.5% (37 of 211) in those with major affective disorder alone (odds ratio=2.19, χ2=9.04, df=1, p<0.003). Among subjects with bipolar disorder, 38.4% (38 of 99) of those with comorbid alcoholism had made a suicide attempt, compared to 21.7% (33 of 152) of those without alcoholism (odds ratio=2.25, χ2=8.22, df=1, p<0.005). Among subjects with recurrent unipolar depression, 7.4% (two of 27) of those with comorbid alcoholism had made an attempt, compared to 6.8% (four of 59) of those without alcoholism (Fisher’s exact test, p=0.62).
Logistic regression analysis showed an odds ratio for alcoholism of 2.6 in subjects with bipolar disorder (Wald χ2=9.5, df=1, p=0.002). The odds of having made a suicide attempt was significantly higher for subjects with bipolar disorder than for subjects with recurrent unipolar depression (odds ratio=6.2, Wald χ2=15.7, df=1, p=0.0001). The odds for subjects with bipolar I disorder were significantly higher than for subjects with bipolar II disorder (odds ratio=2.2, Wald χ2=6.4, df=1, p<0.02). The odds for subjects with bipolar II disorder were significantly higher than for subjects with recurrent unipolar depression (odds ratio=4.4, Wald χ2=8.5, df=1, p=0.004). Use of the generalized estimating equation did not significantly alter these results.
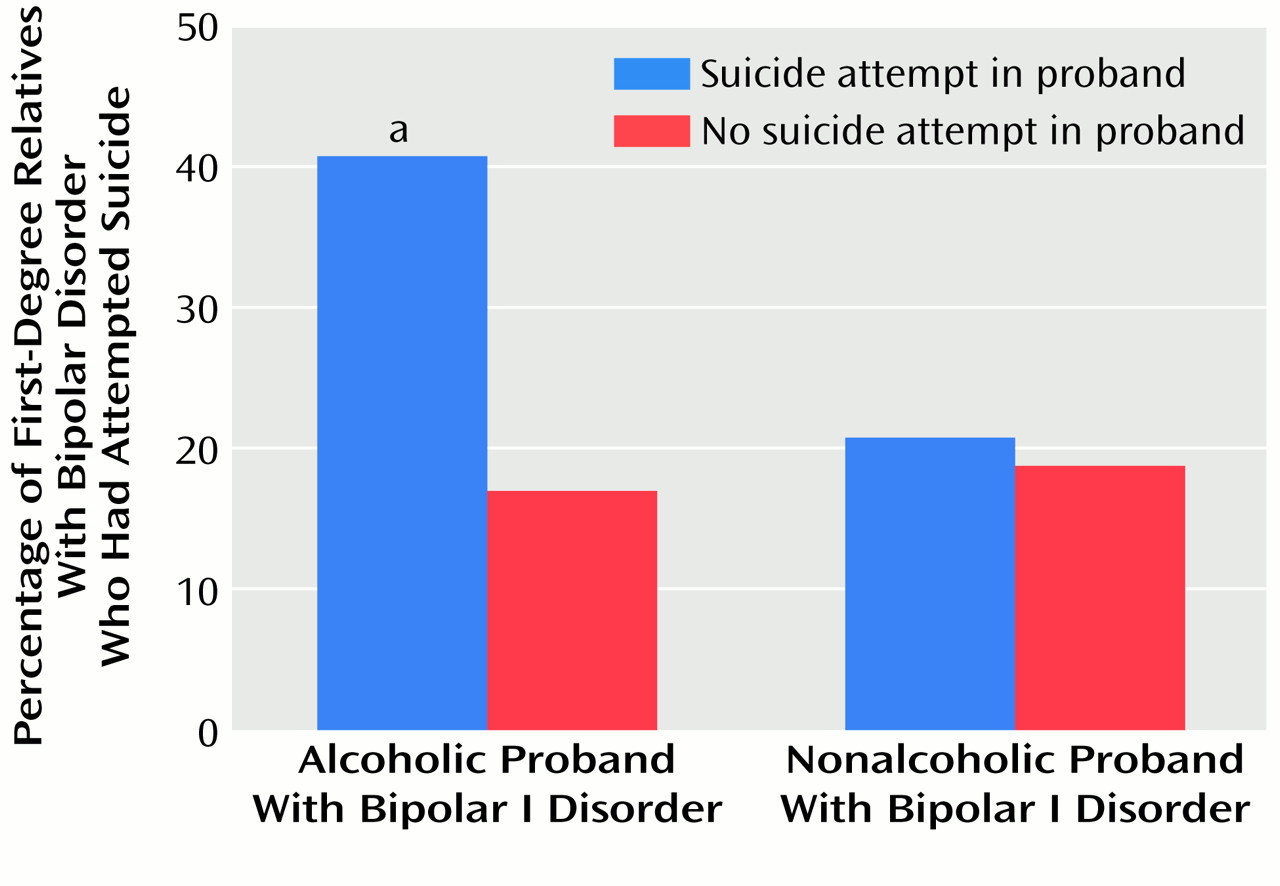
Clustering of subjects with bipolar disorder and alcoholism and a history of suicide attempts occurred in seven of 71 pedigrees. The analysis of familial correlation of attempted suicide in first-degree relatives with bipolar disorder and alcoholism was performed with Tarone’s test and yielded χ
2=4.01 (df=1, p<0.05), suggesting that the null hypothesis of no correlation was unlikely. Analysis by proband group showed that the 11 families in which the proband with bipolar I disorder had comorbid alcoholism and had attempted suicide differed from the other families. Relatives with bipolar disorder in these 11 families had a 40.7% rate (11 of 27) of attempted suicide, compared to 19.0% (22 of 116) in ill relatives of all other probands, a significant difference (
Figure 1).
Discussion
In this study group, 1) alcoholism was associated with a significantly increased lifetime rate of attempted suicide in subjects with bipolar disorder, and 2) alcoholic subjects with bipolar disorder who had attempted suicide clustered in a subset of families.
Two states and a trait may explain the excess suicidal behavior in alcoholic subjects with bipolar disorder. One potentially relevant state is that of transient disinhibition caused acutely by ingestion of alcohol. Disinhibition may increase the likelihood that someone with suicidal ideation would act on self-destructive impulses
(12). A second potentially relevant state is the mixed affective state. The volatile brew of dysphoria, high energy, and agitation may lead to higher rates of suicidal behavior
(13). The trait hypothesis is that comorbid alcoholism and suicidal behavior may occur in a subset of subjects with bipolar disorder who are temperamentally high in novelty seeking, impulsivity, or instability
(14). We had neither temperament data on our subjects, nor data on the subjects’ mood state or alcohol use at the time of their suicide attempts.
We found that bipolar disorder, alcoholism, and attempted suicide cluster in some families. Possible genetic explanations for this clustering are that mixed states and/or temperamental instability or impulsivity may define inherited phenotypic subtypes of bipolar disorder. Nongenetic explanations may include a permissive effect of intoxication on suicidal behavior in individuals with bipolar disorder. The genetic and nongenetic factors that may account for these findings merit further study.