The moral, political, social, and clinical debate engendered by questions of insanity and murder may be traced to the age-old Aristotelian notion of distinguishing actions and actors as either “mad or bad”
(1). Underlying these folk distinctions are two remarkably distinct clinical conditions, psychosis and psychopathy; the former has been historically equated as “mad” and the latter as “bad” by reason of its especially virulent antisociality. Both conditions have distinct patterns of comorbidity and neuropsychology; the latter includes striking clinical differences in social intelligence, reflected by the social anhedonia of schizophrenia and related psychotic conditions, and the superficial, manipulative charm of psychopathy
(2,
3). We examined psychopathy, psychosis, neuropsychology, and murder and report preliminary evidence of two statistically derived clusters of murderers, psychopathic and psychotic, each corresponding to distinct neuropsychological differences in intellectual abilities, learning disabilities, and social intelligence.
Method
Our database (4) consisted of 309 male patients who were committed to Bridgewater State Hospital, referred for neuropsychological testing between 1987 and 1995, and ranged in age from 17 to 80 years (mean=32.7 years, SD=12.3) and in education from 3 to 17 years (mean=10.7, SD=2.7). All subjects had undergone neuropsychological testing with trained technicians under the supervision of a licensed neuropsychologist (P.G.N.). From this database, we identified 26 patients charged with murder who had completed the WAIS-R, the Wechsler Memory Scale—Revised (WMS-R), the Wide-Range Achievement Test—Revised (WRAT-R), and the Wisconsin Card Sorting Test
(4). Subjects were excluded if their records included primary or comorbid medical diagnoses, such as stroke, multiple sclerosis, obstructive cardiopulmonary disease, etc. We then completed Psychopathy Checklist—Revised
(5) ratings on the basis of record review and in the absence of clinical interviews for all 26 subjects charged with murder. In addition, two trained raters independently completed the Psychopathy Checklist—Revised on a randomly selected subset of 15 subjects from the total group of 26. Mean interrater reliability for the total Psychopathy Checklist—Revised was 0.93 when computed across the ratings of these 15 subjects. Mean total score on the Psychopathy Checklist—Revised was 15.4 for the total group of 26 subjects, which is equivalent to approximately the 26th percentile for male forensic patients
(5). We also rated subject records for the presence or absence of a psychotic disorder, defined as a DSM-III-R diagnosis of schizophrenia, schizoaffective disorder, schizophreniform disorder, bipolar disorder with psychotic features, depressive disorder with psychotic features, delusional disorder, or psychotic disorder not otherwise specified
(4). All ratings were performed independently of neuropsychological test data, and raters were blind to the purpose of the study. We then used Ward’s statistical clustering method to compute the squared Euclidean distance between subject profiles as derived from specified rating measures of psychopathy and psychosis
(6).
Results
Ward’s cluster analysis revealed two subgroups of 13 subjects each. Cluster 1 had a higher incidence of psychosis, with 13 of the 13 subjects rated “psychotic” in comparison to none of the 13 subjects in cluster 2. The psychotic subjects of cluster 1 also had lower scores on the Psychopathy Checklist—Revised (total, mean=9.34, SD=6.09; factor 1, mean=4.23, SD=2.62; and factor 2, mean=4.92, SD=4.08) than the cluster-2 subjects. In contrast, the subjects in cluster 2, who were labeled “psychopathic,” scored higher on the Psychopathy Checklist—Revised (total, mean=21.29, SD=7.23; factor 1, mean=10.23, SD=3.32; factor 2, mean=10.36, SD=4.27) than the cluster-1 subjects. Mean years of education were greater (t=2.01, df=4, p<0.06) for the subjects in the psychotic cluster (mean=13.9, SD=2.9) than for the subjects in the psychopathic cluster (mean=11.7, SD=2.4). Subjects in the psychotic cluster were also older (mean=33 years, SD=12), although not significantly so, than the subjects in the psychopathic cluster (mean=36.1 years, SD=2.5).
Multivariate analyses of covariance (MANCOVAs) of WAIS-R psychometric measures (full-scale, verbal, and performance IQs) revealed no significant multivariate cluster effect but a nearly significant interaction effect of cluster and intelligence scale (F=2.96, df=2, 46, p=0.06), which became significant when the covariate of years of education was removed (F=5.57, df=2, 48, p<0.01). Both clusters had similar WAIS-R full-scale mean IQs, but each of the two clusters showed opposite patterns across verbal and performance IQs: Although the psychotic cluster had higher verbal than performance IQs, the psychopathic cluster had higher performance than verbal IQs.
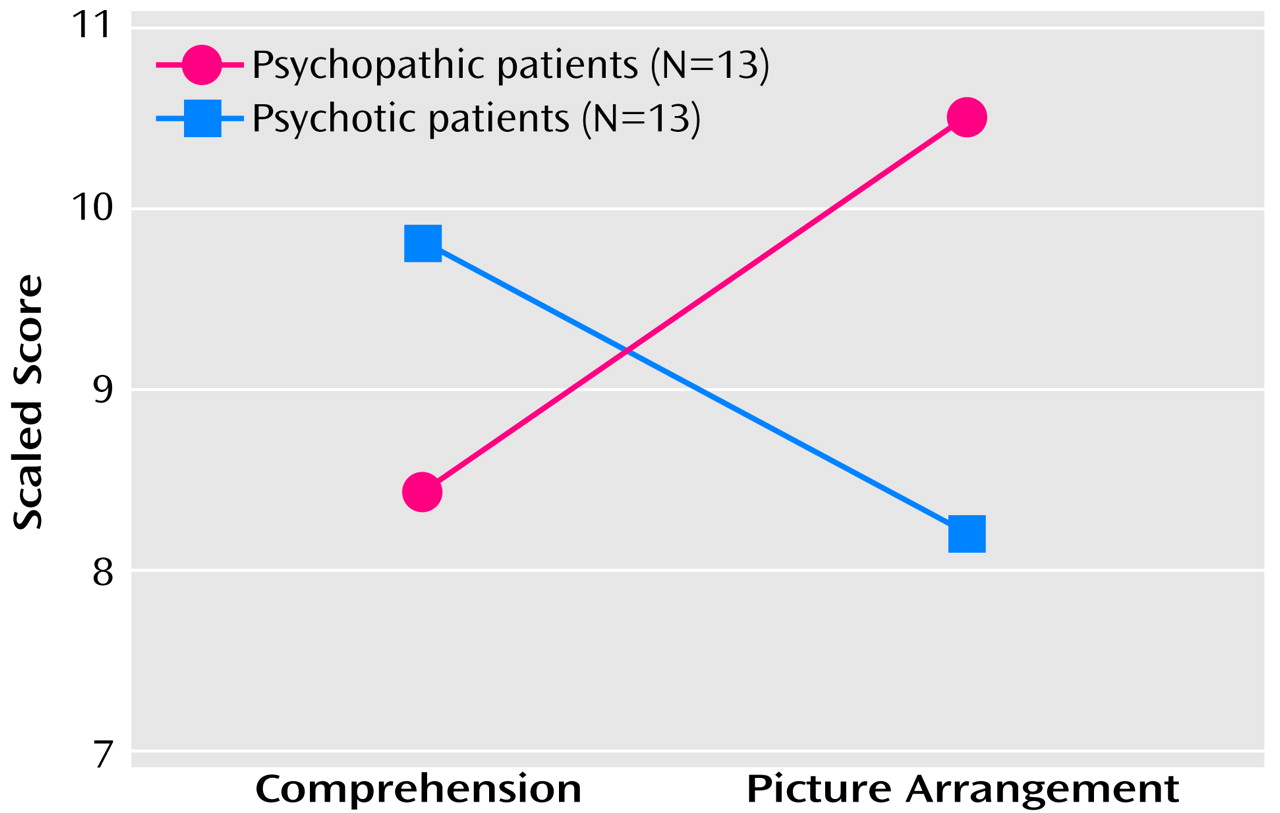
Differences between the clusters emerged, even when we controlled for years of education and for scores on tests of academic abilities such as reading, spelling, and arithmetic (F=3.39, df=3, 19, p<0.05). Scores on follow-up univariate tests revealed a significant multivariate subgroup effect that was largely attributable to cluster differences in scores on tests of written language or spelling (F=6.82, df=1, 21, p<0.02). Likewise, a repeated measures MANCOVA with scores for social intelligence (comprehension and picture arrangement) and with years of education as a covariate revealed a significant cluster-by-subtest interaction effect (F=6.08, df=1, 23, p<0.05). The psychotic cluster scored higher on the comprehension subtest in relation to the picture arrangement subtest, and the psychopathic cluster showed the opposite pattern. The interaction effect remained significant when covariance was for WAIS-R performance IQ (F=7.45, df=1, 23, p<0.05) and for verbal IQ (F=7.86, df=1, 23, p=0.01). These effects remained significant even when WAIS-R summary measures of verbal and spatial abilities were computed without subtest scores for comprehension (F=7.77, df=1, 23, p=0.01) and picture arrangement (F=8.05, df=1, 23, p=0.01) (
Figure 1).
Finally, partial correlation analyses with control for years of education indicated a positive association between psychopathy and scores on the picture arrangement subtest (partial r=0.44, p<0.05) and psychopathy and the number of categories scored correctly, ranging from 0–6, on the Wisconsin Card Sorting Test (partial r=0.61, p<0.05); higher scores on these measures correlated with higher levels of psychopathy. In contrast, higher levels of psychopathy correlated with lower scores on the attention/concentration index of the WMS-R (partial r=–0.53, p<0.05). Psychosis did not correlate with neuropsychological test scores, with the exception of the negative relationship between low subtest scores on picture arrangement with a greater incidence of psychosis (partial r=–0.53, p<0.05).
Discussion
Cluster analysis statistically extracted two subgroups of 13 mentally disordered murderers, one defined primarily by psychosis and the other by psychopathy. Despite similar levels of overall intelligence, verbal intelligence surpassed performance intelligence for the psychotic cluster; the opposite pattern was evident for the psychopathic cluster, along with evidence of a formal language-related learning disability. Differences in social intelligence emerged, even when we statistically controlled for cluster differences in verbal and performance intellectual abilities, which conformed well with descriptions of psychopathy that typically emphasize Machiavellian intelligence in the absence of social emotions such as love, shame, guilt, and remorse
(3). On the other hand, the subjects assigned to the psychotic cluster scored higher on neuropsychological measures than is typical of patients with chronic schizophrenia
(7). However, these scores were consistent with evidence of relative preservation in overall neuropsychology, as demonstrated in other groups of psychotic violent offenders, including those charged with serious felonies as well as those acquitted as not guilty by reason of insanity of murder
(4).
In conclusion, these data are preliminary in nature and are limited by the selection biases inherent in a relatively small group of men who fell within the extreme ranges for crime committed and psychopathology. In addition, formal diagnostic procedures for axes I, II, and III disorders would also be necessary so that comorbidity might also be addressed. Finally, if feasible, better characterization of these clusters by using brain imaging measures in conjunction with the neuropsychological tests employed here (e.g., the Wisconsin Card Sorting Test) may prove beneficial.