Posttraumatic stress disorder (PTSD) is one of the most common mental disorders in the United States
(1,
2) and is particularly prevalent among individuals exposed to war, with conservative estimates suggesting that as many as 22% of veterans who experience combat have clinically significant chronic PTSD
(2). Patients with PTSD have higher rates of health complaints and medical morbidity, including cardiovascular, respiratory, musculoskeletal, and neurological problems, than those without PTSD
(2,
3). Surprisingly few studies have examined the question of how PTSD relates to general health care utilization
(2,
4–6). The majority of studies examining the relationship between PTSD and health service use have focused on the consumption of mental health services and have reported substantial use of those services by individuals with PTSD
(2,
6–10). Still, others have suggested that as a result of associated health complaints and problems, patients with PTSD are more likely to receive care in traditionally nonmental health care settings
(11).
Unfortunately, research examining mental health service use of patients with PTSD, as well as studies of general or physical health service use in these patients, have relied on self-report measures of utilization
(2,
4–
6,
8–10) (compare with reference
7), severely hampering conclusions about the relationship between PTSD and service use. As self-reports are subject to response biases that may limit their validity
(12), objective utilization measures are needed to accurately define the burden of PTSD on the health care system.
The current study was designed to characterize both the physical health and the mental health service use of veterans with PTSD through the use of objective utilization measures. Veterans with a diagnosis of PTSD were compared to veterans without PTSD on objective measures of inpatient and outpatient utilization. We hypothesized that patients with PTSD would exhibit both more physical health service use and more mental health service use than patients without PTSD.
Method
Participants
The study subjects consisted of 996 male combat veterans who were seeking help for PTSD symptoms and were evaluated for PTSD between March 1992 and September 1998 at a Veterans Affairs (VA) specialty PTSD clinic in the southeastern United States. The study group included patients who were new to the clinic and reported having been exposed to combat, as measured by scoring >0 on the Combat Exposure Scale
(13). Patients were both self-referred and referred by primary care clinicians for PTSD evaluation. PTSD diagnoses were based on either the Structured Clinical Interview for DSM-III-R
(14) or the Clinician-Administered PTSD Scale
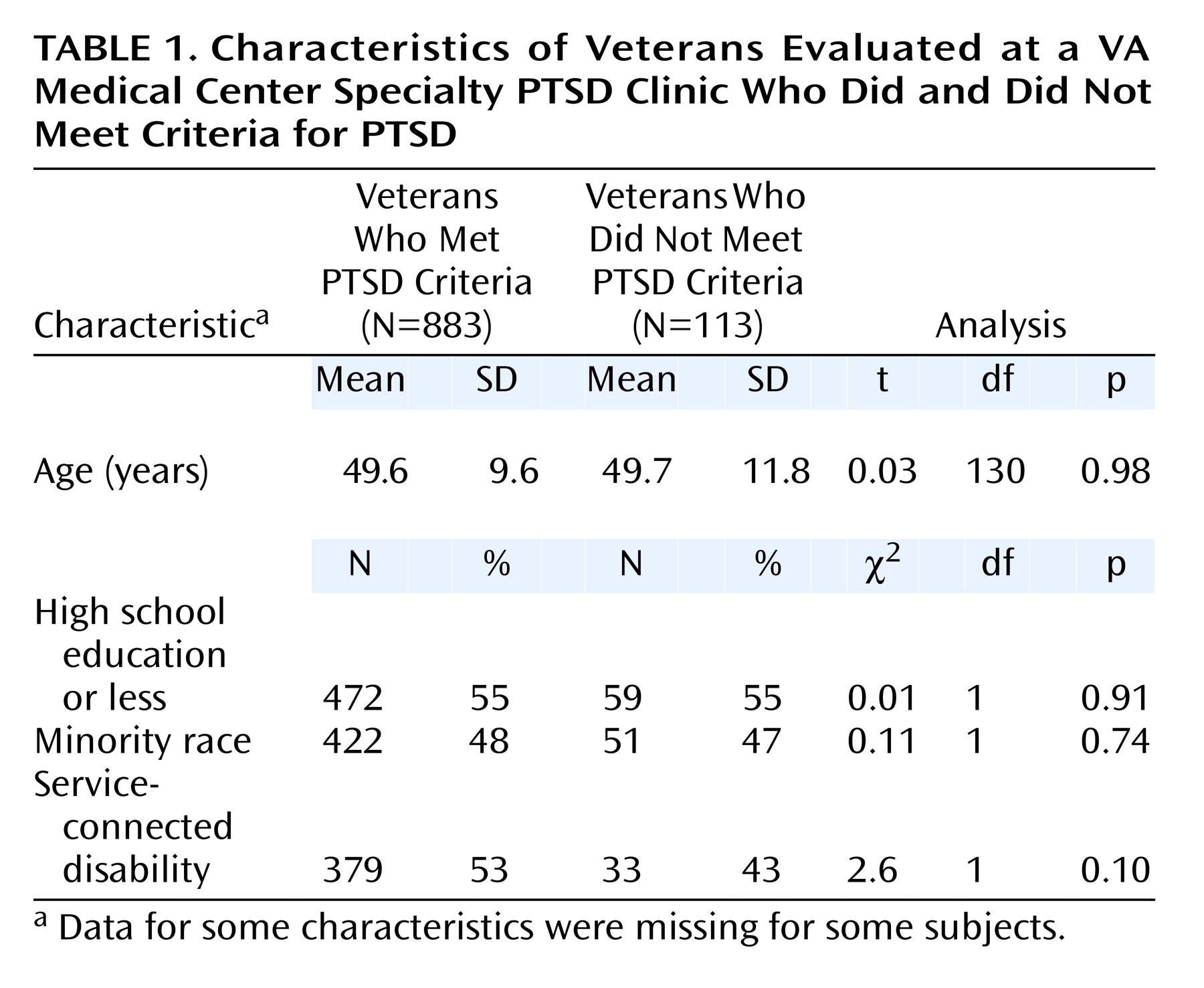
(15). The reliability of the diagnoses between clinicians during the period was good (kappa=0.83). Of the 996 patients seeking an evaluation, 883 (89%) met the full criteria for PTSD and 113 (11%) did not meet the full criteria. The two groups did not differ in age, education, racial composition, or the percentage of patients who had a service-connected disability (
Table 1). The VA defines a service-connected disability as a disability occurring because of injury or disease that was incurred or was aggravated during military service and does not bill for treatment of these conditions.
PTSD Symptom Severity
PTSD symptom severity was assessed with the Mississippi Scale for Combat-Related PTSD, a widely used, valid, and reliable measure of PTSD
(16). This scale consists of 35 items, each rated on a 5-point scale, yielding scores ranging from 35 to 175. Higher scores reflect more severe PTSD symptoms.
Medical Utilization Measures
Data were obtained from centralized VA databases and were collected for a period of 1 year after the date when the patient was evaluated for PTSD. The VA Patient Treatment File, which captures nearly 100% of all VA hospital episodes
(17), and the VA Outpatient Clinic File, which contains information on all ambulatory contact with the VA (18), served as sources for medical service utilization measures. Both of these databases are thought to be valid and accurate and are used routinely for billing purposes
(17,
18). VA clinic “stops,” defined as a patient encounter with one or more health professionals within a particular clinic, were used as the unit of analysis for outpatient services. For both outpatient services and VA hospitalizations, a clinic classification system was used to categorize care into two mutually exclusive types to allow inferences about whether the care was for medical or psychiatric reasons (compare with reference
19). Dependent measures included the numbers of outpatient physical health clinic stops, mental health clinic stops, psychiatric hospitalizations, and medical/surgical hospitalizations.
Analyses
Logistic and negative binomial regression models were used to examine the association between medical utilization measures and PTSD explanatory variables. All regression models were adjusted for demographic factors, including race, age, education, and service-connected disability status. All statistical analyses were performed with SAS PC, Version 8 (SAS Inc., Cary, N.C.). Given the low frequency of inpatient service use, variables measuring hospitalizations were dichotomized (no use, some use) and modeled by using logistic regression. Variables measuring outpatient health service utilization (medical and psychiatric) were recorded as counts of clinic stops.
Methods appropriate for the analysis of count data include Poisson and negative binomial regression
(20). Negative binomial regression, a generalization of the Poisson regression model, is more appropriate when data are overdispersed, i.e., with variance greater than the mean, as overdispersion can produce underestimates of standard errors in Poisson models leading to overstatement of statistical significance. Due to the highly skewed and overdispersed nature of the outpatient utilization counts, these data were analyzed by using negative binomial regression models. As in Poisson regression analysis, each negative binomial regression coefficient, when exponentiated, is an estimate of the incidence rate ratio, e.g., the ratio of the incidence of outpatient physical health clinic stops in the PTSD group to that in the comparison group.
Post hoc analyses examined interactions of each primary independent variable (i.e., PTSD diagnosis and PTSD severity) and all other demographic and disability variables. These models included main effects and all two-way interactions between PTSD and demographic variables. Nonsignificant interaction terms were removed from the final models. Disability status was dichotomized (yes and no), and patients with any medical or psychiatric service-connected disability were assigned a “yes” code for disability status. Race was coded as white and nonwhite. Age was dichotomized at 52 years of age (≤52 and >52 years) on the basis of an empirical assessment of the distribution of age in relation to the medical utilization measures. Education was dichotomized as high school or less versus more than high school. For analytic purposes, the referent categories for the four demographic and disability variables were no disability, nonwhite, young, and high school or less, respectively.
For the analyses of PTSD symptom severity, four groups were created on the basis of the quartiles of the distribution of scores on the Mississippi Scale for Combat-Related PTSD in the PTSD group. The cutoffs for each quartile were as follows: first quartile, 73–114; second quartile, 115–125; third quartile, 126–140; and fourth quartile, 141–170. Patients in the first quartile had the lowest symptom severity, and those in the fourth quartile reported the most severe symptoms. For analytical purposes, the first quartile was used as the referent category. Five participants in the PTSD group had more than 190 outpatient mental health clinic stops over 1 year. Further investigation revealed that these patients were enrolled in a special work-therapy program, which accounted for the unusually high utilization rates. Data for these patients were subsequently removed from the analyses examining mental health service use.
Results
PTSD Diagnosis and Inpatient Service Use
Among the patients with a diagnosis of PTSD, 183 (21%) had at least one hospitalization in the 1-year period after their assessment. A similar percentage of the comparison group (19%, N=21) had at least one inpatient visit. No group differences were found in the percentage of patients who had at least one medical/surgical hospitalization (10% of PTSD patients versus 14% of non-PTSD patients) (χ2=1.66, df=1, p=0.20). The percentage of patients who had at least one psychiatric hospitalization was slightly greater in the PTSD group (12%) than in the comparison group without PTSD (6%) (χ2=3.47, df=1, p=0.06), although PTSD diagnosis failed to reach statistical significance in the logistic regression analysis of inpatient psychiatric use after the effects of the covariates were controlled (Wald χ2=0.46, df=1, p=0.50, odds ratio=1.35, 95% confidence interval [CI]=0.56–3.26). Having more than a high school education reduced the odds of VA psychiatric hospitalization (Wald χ2=4.04, df=1, p=0.04, odds ratio=0.62, 95% CI=0.39–0.99). Similarly, older age was associated with decreased odds of psychiatric hospitalization (Wald χ2=10.65, df=1, p=0.001, odds ratio=0.29, 95% CI=0.14–0.61). There were no significant interactions between PTSD and demographic variables in the analyses examining inpatient service use.
PTSD Diagnosis and Outpatient Service Use
The patients with PTSD had a median of 18 stops in outpatient physical health clinics and a median of seven outpatient mental health clinic stops in the year after evaluation. In contrast, the patients without PTSD had a median of only 10 stops in physical health clinics and 4 mental health clinic stops.
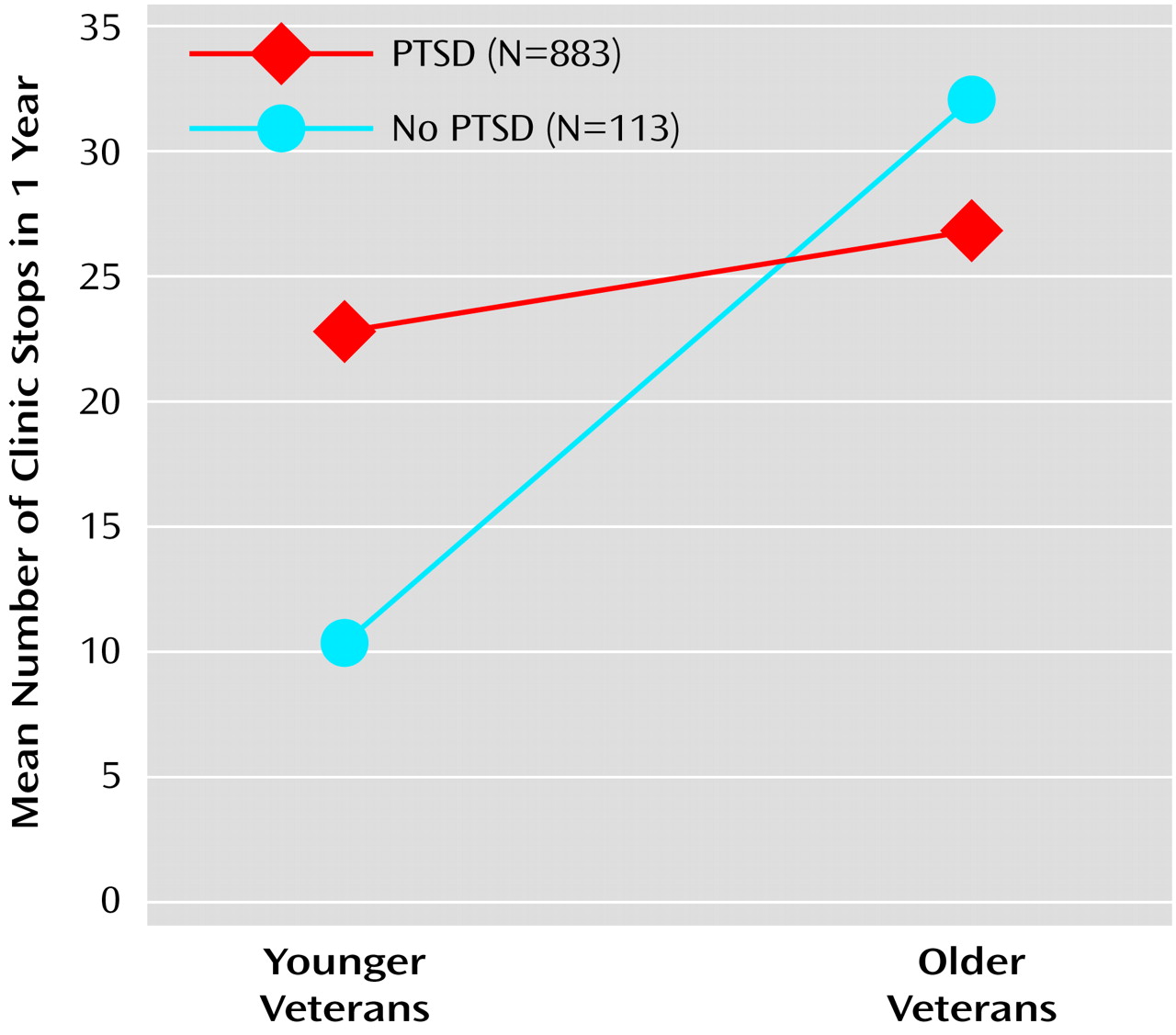
The results indicated significant main effects for PTSD in analyses of both outpatient physical and mental health utilization. However, the post hoc analyses examining two-way interactions between PTSD and the demographic variables revealed significant findings, suggesting that PTSD main effects should not be interpreted. Thus, we report results for the interactions between PTSD and the demographic variables.
Results from negative binomial regression analyses revealed a significant interaction of PTSD and age for the use of outpatient physical health services (
Figure 1). A diagnosis of PTSD was associated with a significantly higher rate of utilization of outpatient physical health services among younger patients. Younger patients with PTSD had an estimated 124% higher rate of outpatient physical health service use than younger patients without PTSD (Wald χ
2=43.11, df=1, p=<0.0001, incidence rate ratio=2.24, 95% CI=1.76–2.85). No significant effect of PTSD among older patients was found (Wald χ
2=1.49, df=1, p=0.22, incidence rate ratio=0.80, 95% CI=0.56–1.15). There was a significant age effect among patients without PTSD, with older patients using physical health services at rates 202% higher than younger patients (Wald χ
2=27.64, df=1, p=<0.0001, incidence rate ratio=3.02, 95% CI=2.00–4.57). However, no effect of age was found in the utilization of physical health services among patients with PTSD (Wald χ
2=1.07, df=1, p=0.30, incidence rate ratio=1.08, 95% CI=0.94–1.24). Patients with a service-connected disability had a significantly higher rate of utilization of outpatient physical health services than those without a service-connected disability (Wald χ
2=78.05, df=1, p=<0.0001, incidence rate ratio=1.69, 95% CI=1.50–1.90).
The results for outpatient mental health utilization revealed significant interactions between PTSD, age, and disability status. These interactions indicated a significant PTSD effect among relatively younger patients. This effect was even greater among patients with a service-connected disability. Thus, relatively young patients with PTSD and without a service-connected disability used mental health services at rates 97% higher than younger patients without PTSD and without a service-connected disability (Wald χ2=14.10, df=1, p=0.0002, incidence rate ratio=1.97, 95% CI=1.38–2.81). However, relatively younger patients with PTSD who had a service-connected disability used mental health services at rates 260% higher than younger patients who had a service-connected disability but did not have PTSD (Wald χ2=41.95, df=1, p=<0.0001, incidence rate ratio=3.60, 95% CI=2.44–5.31). Among relatively older patients, PTSD diagnosis was not significantly associated with mental health service use for veterans with a service-connected condition (Wald χ2=0.11, df=1, p=0.74, incidence rate ratio=1.07, 95% CI=0.72–1.57) and was associated with a decrease in mental health service use among veterans without a service-connected condition (Wald χ2=6.14, df=1, p=0.01, incidence rate ratio=0.58, 95% CI=0.38–0.89).
PTSD Severity and Inpatient Service Use
The analyses of the relationship of PTSD severity with inpatient service use included data only from the patients with PTSD. Logistic regression models indicated that PTSD symptom severity did not significantly increase the odds of medical/surgical hospitalization (results not shown). Severity of PTSD symptoms, however, was associated with a higher likelihood of psychiatric hospitalization. The likelihood of psychiatric hospitalization did not differ between patients in the second quartile of symptom severity and those in the first quartile, who had less severe symptoms (Wald χ2=0.58, df=1, p=0.44, odds ratio=1.46, 95% CI=0.56–3.81). Patients with more severe PTSD, however, were more likely to have one or more psychiatric hospitalizations in the year after receiving the PTSD diagnosis. Patients in the third quartile of severity had 3.89 times the odds of a psychiatric hospitalization, compared with veterans with the least severe symptoms (Wald χ2=10.5, df=1, p=0.001, odds ratio=3.89, 95% CI=1.71–8.87). Patients with the most severe PTSD symptoms had 4.11 times the odds of a psychiatric hospitalization, compared with patients with the least severe symptoms (Wald χ2=11.5, df=1, p=0.001, odds ratio=4.11, 95% CI=1.82–9.29).
PTSD Severity and Outpatient Service Use
The analyses of outpatient physical and mental health service use included data only from the patients with PTSD. There were several significant interactions that were similar to previous findings. For clinics traditionally focused on physical health care, there was a significant age effect, with older patients using outpatient physical health services at a 16% higher rate than younger PTSD patients (Wald χ2=4.29, df=1, p=0.04, incidence rate ratio=1.16, 95% CI=1.01–1.33). The results also indicated a significant interaction of PTSD severity and service-connected disability status. This interaction can be explained by a significant disability effect for all patients with PTSD, except for those with the most severe PTSD. Specifically, among patients with the least severe PTSD, those with a service-connected disability used physical health services at a 113% higher rate than those without a service-connected disability (Wald χ2=35.47, df=1, p=<0.0001, incidence rate ratio=2.13, 95% CI=1.66–2.73). Similarly, among patients in the second quartile of PTSD severity, those with a service-connected disability used physical health services at a higher rate (Wald χ2=29.81, df=1, p=<0.0001, incidence rate ratio=2.00, 95% CI=1.56–2.57), as did those in the third quartile of PTSD severity (Wald χ2=19.05, df=1, p=<0.0001, incidence rate ratio=1.69, 95% CI=1.33–2.13). Disability status, however, was unrelated to the use of physical health service utilization among the patients with the most severe PTSD (Wald χ2=2.22, df=1, p=0.14, incidence rate ratio=1.19, 95% CI=0.95–1.50). Among patients without a service-connected disability, those in the third quartile of PTSD severity (Wald χ2=6.85, df=1, p=0.009, incidence rate ratio=1.38, 95% CI=1.08–1.75) and those in the fourth quartile used significantly more outpatient physical health services than those with less severe PTSD (i.e., compared with patients in the first quartile; Wald χ2=22.66, df=1, p=<0.0001, incidence rate ratio=1.79, 95% CI=1.41–2.27). No other significant severity effects were found.
Results of the regression analyses examining the use of outpatient mental health services as a function of PTSD severity were similar to those in the analyses examining outpatient physical health use. Older age was associated with a 22% higher rate of mental health outpatient service use (Wald χ2=8.96, df=1, p=0.003, incidence rate ratio=0.78, 95% CI=0.66–0.92). The results also revealed a significant interaction of PTSD severity and service-connected disability status. Similar to the findings for physical health service use, symptom severity among PTSD patients without a service-connected disability was associated with a higher rate of mental health service use. Although individuals without a service-connected disability in the third quartile of symptom severity did not differ significantly from those with the least severe symptoms (Wald χ2=3.24, df=1, p=0.07, incidence rate ratio=1.30, 95% CI=0.98–1.72), those in the second quartile (Wald χ2=15.31, df=1, p=<0.0001, incidence rate ratio=1.78, 95% CI=1.33–2.38) used mental health outpatient services at an estimated 78% higher rate and those with the most severe PTSD used mental health outpatient services at an estimated 138% higher rate than patients in the first quartile (Wald χ2=37.34, df=1, p=<0.0001, incidence rate ratio=2.38, 95% CI=1.80–3.15). There were no symptom severity effects among those with a service-connected disability.
Discussion
Younger help-seeking, combat-exposed veterans with PTSD used significantly more outpatient services in the year after their PTSD evaluation than those without PTSD. For older veterans, there was little difference between patients with PTSD and those without PTSD in the rates of both physical and mental outpatient service use. Among patients with PTSD, symptom severity increased the odds of psychiatric hospitalization. Greater symptom severity was also associated with higher rates of outpatient physical and mental health use among veterans without a service-connected disability.
Objective health service utilization data obtained from computerized centralized databases provide further evidence that PTSD is associated with a higher rate of health service use. The results of the current study are generally consistent with the literature examining the self-reported health service use of patients with PTSD
(2). To our knowledge, previous studies examining the health service use of patients with PTSD have not examined or reported possible interactions with demographic factors. The interaction effect of PTSD diagnosis and age in the use of outpatient services may suggest that PTSD is associated with the early development of significant medical conditions. This finding is consistent with a longitudinal study by Elder et al.
(21), which found that the health trajectories of WWII veterans varied significantly as a function of combat exposure. More research is needed to examine the health trajectories of patients who develop PTSD.
Veterans with PTSD use a significant amount of VA services. For comparison purposes, a study by Ashton and others
(19) reported that among all veterans who use VA health services, the national average use of outpatient services for a 1-year period was 17 clinic stops. In comparison, patients with PTSD in the current study had a median of 18 clinic stops in physical health clinics alone. In addition to this use, PTSD patients had a median of seven stops in mental health clinics during the 1-year study period.
The results of the current study are consistent with suggestions that veterans with PTSD are more likely to receive care in traditionally nonmental health care settings within the VA
(11). PTSD patients had more than twice as many clinic stops in nonmental health care settings as in mental health clinics. This finding underscores the potential importance of educating primary care clinicians about the special needs of this patient group and about the factors that may affect compliance with medical treatments in this group (e.g., problems with anger and irritability, concentration problems, poor social support). Primary care clinicians should also explore health risk behaviors, such as smoking and alcohol use, that are prevalent in this population
(2,
3). An important direction for future research is an investigation of the impact of symptom perception and the specific medical conditions that may be associated with this higher rate of medical service use.
The current study had several limitations that warrant discussion. First, although the methods allowed objective measurement of all VA health care utilization, possible service use outside the VA system was not assessed. Thus, the reported volume of service use may be an underestimation of the total medical service use associated with PTSD. Relatively little is known about the cross-system use of VA and non-VA services by veterans
(22).
The possibility that help-seeking veterans who were not diagnosed with PTSD avoid VA health services and use non-VA services at a higher rate than patients with PTSD cannot be ruled out. While the analyses controlled for service-connected disability status assessed at the time of the PTSD evaluation, patients who received a PTSD diagnosis and subsequently filed for PTSD-related compensation may have been more likely to gain access to free mental health care than those without the disorder. The study period of 1 year was chosen to minimize this potential confound. Unpublished data collected at the study site showed that for virtually all patients diagnosed with PTSD in the clinic, a period of >12 months transpired between the time patients were evaluated and the time they received a service-connected disability for PTSD. Specifically, only two (1.6%) of 129 patients received a PTSD-related disability before 12 months (J.C. Beckham, personal communication, 1998). Thus, these data support the belief that the results reflect differences associated with PTSD rather than with eligibility factors. Furthermore, we found evidence that the help-seeking veterans without PTSD were frequent users of VA services. The overwhelming majority of these patients (91%) had at least one outpatient VA visit in the study period, and the overall volume of VA service use by help-seeking veterans without PTSD was comparable to an estimate of the national average
(19).
Greater severity of PTSD increased the odds of both physical and mental health service use among patients without a service-connected disability. These results are consistent with research suggesting that greater PTSD symptom severity increases the risk of poor health
(3). The lack of significant severity effects among those with a service-connected disability is surprising but may be attributable to greater access to care associated with a documented service-connected disability. Any conclusions regarding these findings are limited, however, by the restricted range of PTSD severity in the sample. Although the study group was representative of patients presenting at VA specialty PTSD clinics, these patients tend to have chronic, severe PTSD. Further research is needed to examine the relationship between PTSD and health service use in non-combat-related PTSD populations.
Finally, the unique effects of PTSD on health service use cannot be addressed in the current study because comorbid diseases were not assessed. Both help-seeking, combat-exposed veterans and patients with chronic PTSD often have concomitant or comorbid illnesses, including major depression, alcohol or other substance use disorders, and personality disorders
(2). Previous research has generally supported a relationship between depression and a higher rate of health service use
(23,
24). Similarly, a substance abuse dual diagnosis may be associated with more service use and higher service costs (25), although previous studies have been less consistent on this point
(23). Despite evidence that PTSD is associated with poor health, even after controlling for substance abuse, depression, and other risk factors, including smoking
(3), future research should examine the independent contribution of PTSD to health service use. One recent study by Schnurr et al.
(4) found that PTSD contributed to self-reports of medical utilization, even after accounting for other axis I disorders, including substance abuse. Examination of the specific types of mental health outpatient services used by patients with PTSD (e.g., substance abuse treatment versus treatment for PTSD) would also be informative.
The results of the present investigation have implications for clinical practice. As mentioned previously, these data support the recommendation of several authors for increased collaboration between primary care and mental health professionals
(11). The results support an association between PTSD and a higher rate of health service utilization and suggest the potential importance of screening for PTSD in medical clinics. Given that there are currently safe and effective treatments for PTSD
(26), as well as evidence suggesting that psychotherapy reduces medical costs
(27), further research is needed to evaluate the benefits for screening for PTSD in medical settings.
In conclusion, combat veterans with PTSD had significantly greater outpatient service use than those without PTSD. Among veterans with PTSD, greater symptom severity increased the odds of a VA psychiatric hospitalization and was associated with a higher rate of outpatient service use among patients without a documented service-connected disability. Although the mental health service use of patients with PTSD was substantial, PTSD patients used more services in traditionally nonmental health clinics. This finding underscores the importance of educating primary care clinicians about the special needs of this population. Given the relationship between PTSD and a higher rate of service use, future research should evaluate the potential benefits of screening for PTSD in medical clinics.