Patients
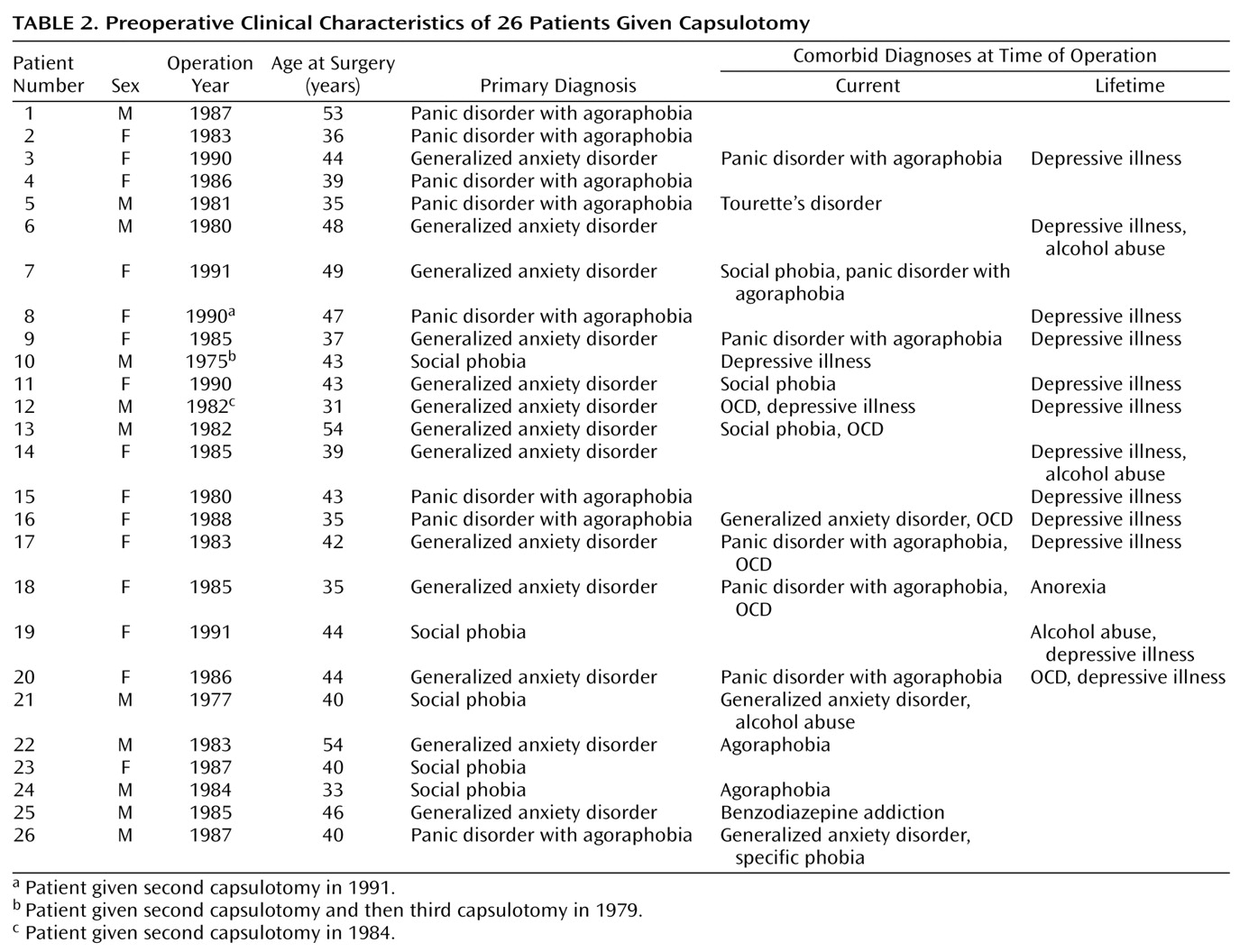
All 26 consecutive patients with anxiety disorders other than OCD who were treated with bilateral thermocapsulotomy between 1975 and 1991 at the Karolinska Hospital in Stockholm were included in the study. Fifteen of the patients were women, and 11 were men.
The patients’ mean age at first capsulotomy was 41.4 years (SD=6.5, range=31–54), and their mean duration of illness at the time of surgery was 18.0 years (SD=9.2, range=5–40). Their mean age at long-term follow-up was 54.5 years (SD=8.3, range=42–71, N=18).
For patients operated on after 1980, the DSM-III or DSM-III-R criteria for anxiety disorders were systematically assessed on the basis of a clinical semistructured interview. At long-term follow-up, the preoperative diagnoses were checked by P.M. and C.R. The patients’ primary diagnoses were generalized anxiety disorder (N=13), panic disorder (N=8), and social phobia (N=5).
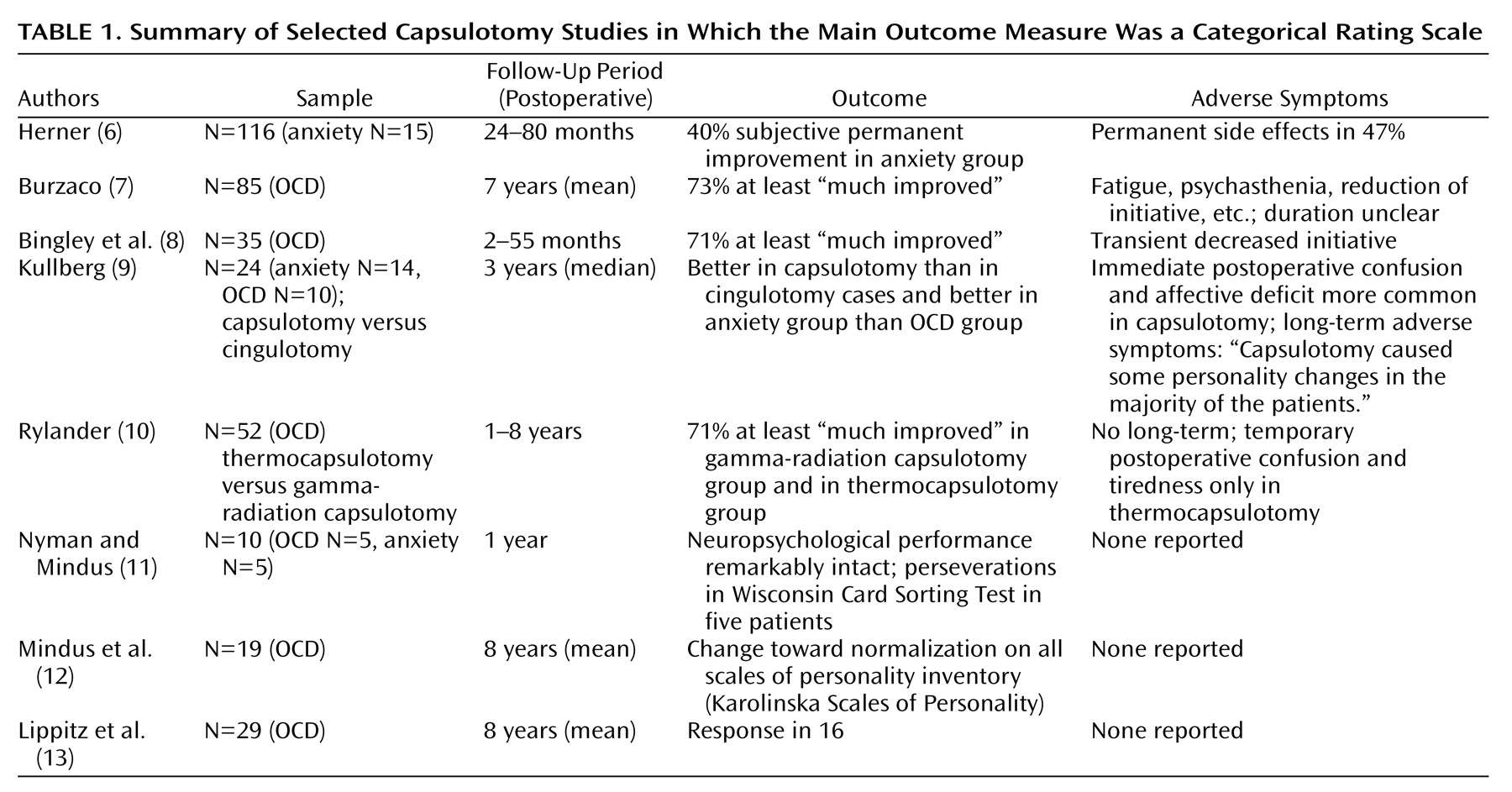
Table 2 shows other current and lifetime comorbid psychiatric disorders at the time of surgery. None of the patients had OCD as their primary diagnosis, although six had OCD of minor severity as a comorbid condition.
Inclusion criteria for capsulotomy have been described elsewhere
(15,
16). In sum, they were 1) illness was chronic (duration ≥5 years), 2) illness caused substantial suffering and considerable reduction in psychosocial functioning, 3) current psychological and pharmacological treatment options were tried systematically for at least 5 years without substantial effect, and 4) the patient provided informed consent.
All patients had participated in psychotherapeutic trials to little or no avail. Nine patients had been treated with individual behavioral therapy, and the remaining patients had received different long-term psychodynamic psychotherapies.
All patients had been treated with benzodiazepines and antidepressants. Eighteen patients had been treated with serotonin reuptake inhibitors (clomipramine, zimelidine, or citalopram), seven had been treated with monoamine oxidase inhibitors, and 16 had been treated with neuroleptics. Thirteen had received ECT.
Eighteen of the 26 patients were available for long-term follow-up; 17 were followed up in person, and one was interviewed by telephone because the illness of a relative prevented her from coming to the interview. Of the eight patients lost to long-term follow-up, three had died (of suicide, chronic alcoholism, and cardiovascular disease, respectively), two were too somatically ill to be interviewed, one refused to participate, and two did not show up. The patient who committed suicide (patient 12) made multiple suicide attempts before the first surgery and had long been suicidal. Relatives of all 18 patients were interviewed.
The ethics committee at the Karolinska Hospital approved the study. After a complete description of the study to the subjects, written informed consent was obtained. Fourteen of the patients were previously included in a 1-year follow-up study of capsulotomy
(14), and five patients were included in an earlier neuropsychological study
(11).
Follow-Up Assessments
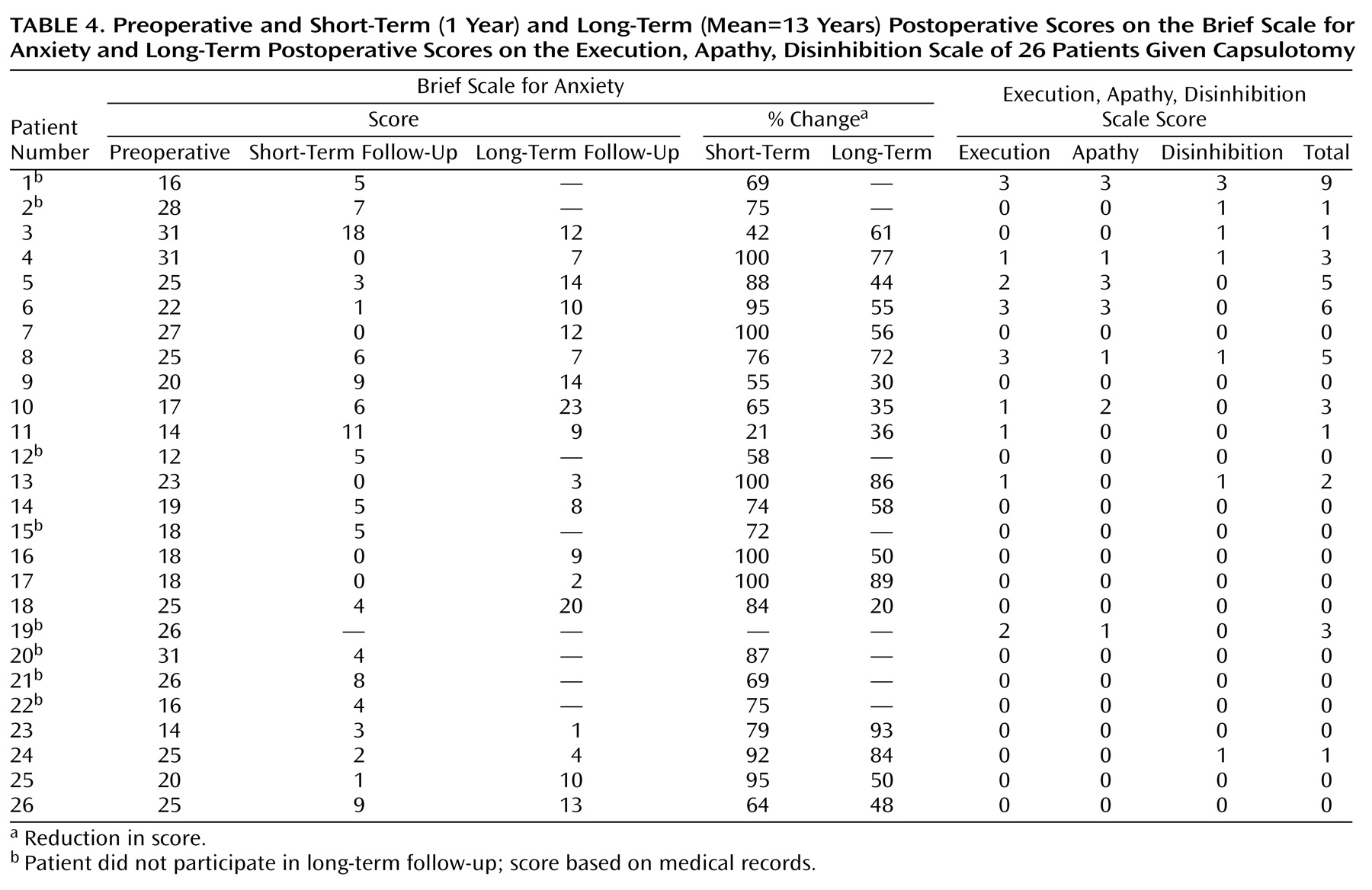
Short-term (1 year after first surgery) and long-term (mean=13 years after first surgery, SD=4.1, range=7–23) assessments were compared with preoperative data. The clinical ratings at the long-term follow-up were done by C.R. or S.A., who were not involved in patient selection or postoperative care. The long-term follow-up was conducted in 1998 and 1999. The preoperative and 1-year ratings were done by P.M.
The Brief Scale for Anxiety
(17) is a rating scale for measuring anxiety symptoms, derived from the Comprehensive Psychopathological Rating Scale
(18). The Brief Scale for Anxiety consists of eight reported and two observed items, scored on a 0–6 Likert scale. In the present study, only the eight reported items were used.
The Montgomery-Åsberg Depression Rating Scale
(19) is a widely used depression rating scale. Global improvement was measured by the investigator on the Physician’s Global Improvement Scale and by the patient on the Patient’s Global Improvement Scale
(20). In the present study an 11-point Likert scale was used on which a score of 10 indicates maximal improvement. The Global Assessment of Functioning Scale, i.e., axis V of DSM-IV (p. 32), is a composite measure of current psychological, social, and occupational functioning. The Physician’s Global Improvement Scale, Patient’s Global Improvement Scale, and Global Assessment of Functioning Scale scales were used only at long-term follow-up.
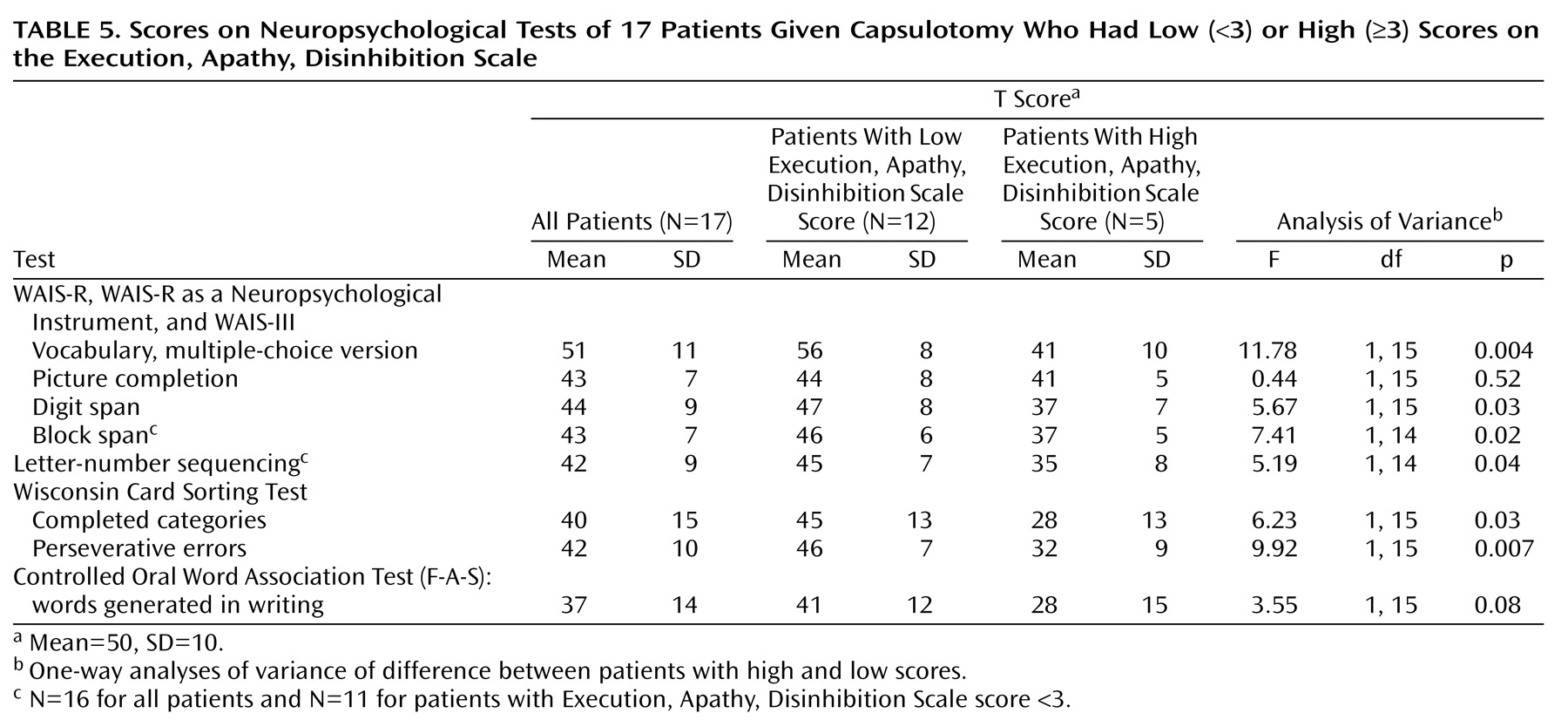
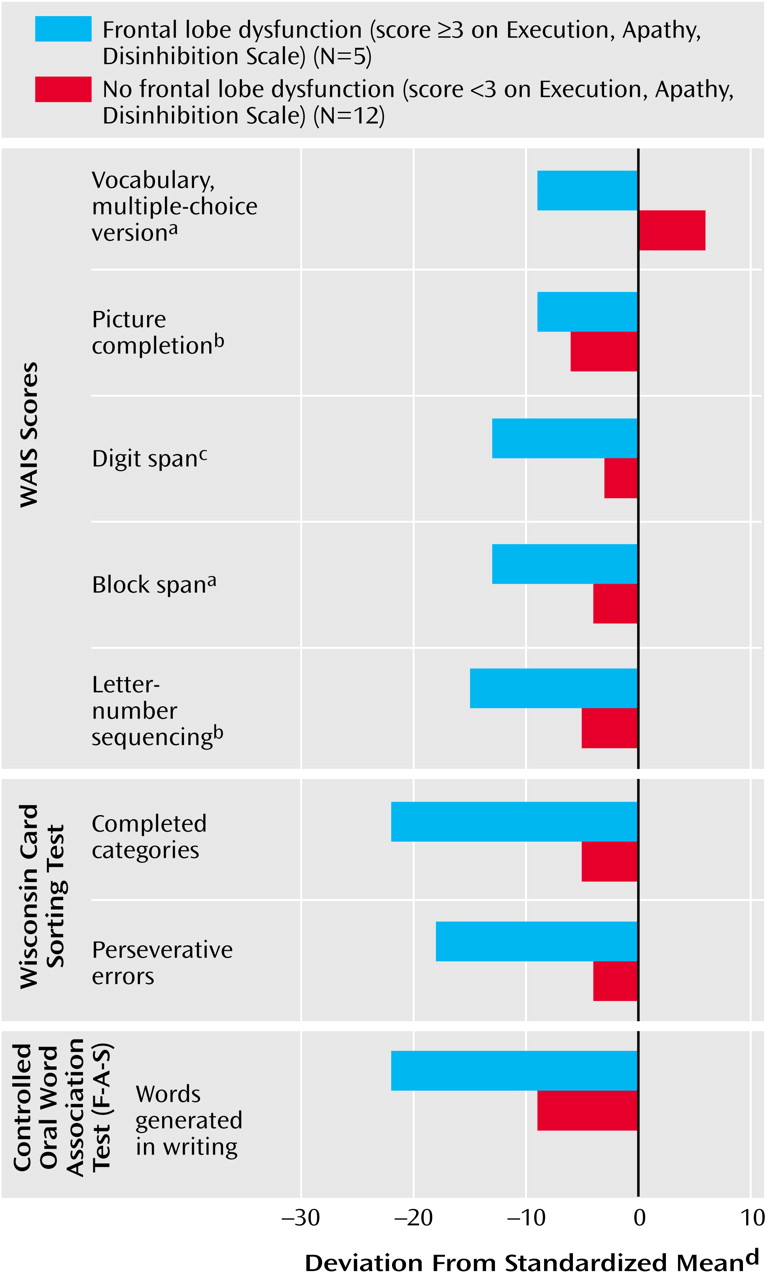
All adverse symptoms were recorded during a semistructured clinical interview at long-term follow-up. Because we were unaware of rating instruments for symptoms of frontal lobe functioning, we constructed a simple rating scale, the Execution, Apathy, Disinhibition Scale, designed to measure three important functions of what has been postulated to be frontal lobe dysfunction, namely, executive dysfunction, apathy, and disinhibition
(21). Severity is rated on a 4-point Likert scale (scores=0–3) for each of the three items. A score of 3 indicates the highest level of severity. Patients with a total score ≥3 were rated as having significant dysfunction. All patients were rated by two psychiatrists (C.R. and S.A.) on the basis of videotaped clinical interviews with each patient and his or her relatives and/or other available material (e.g., patient files). The interrater reliability for the total Execution, Apathy, Disinhibition Scale scores was 0.92 (p<0.001). Disagreement occurred regarding only one patient. For the separate ratings, the interrater reliability varied between 0.72 (disinhibition, p<0.001) and 1.00 (apathy, p<0.001). There were no significant differences between the two raters. Consensus was reached for all ratings before the Execution, Apathy, Disinhibition Scale scores were entered into the raw data matrix.
The Karolinska Scales of Personality
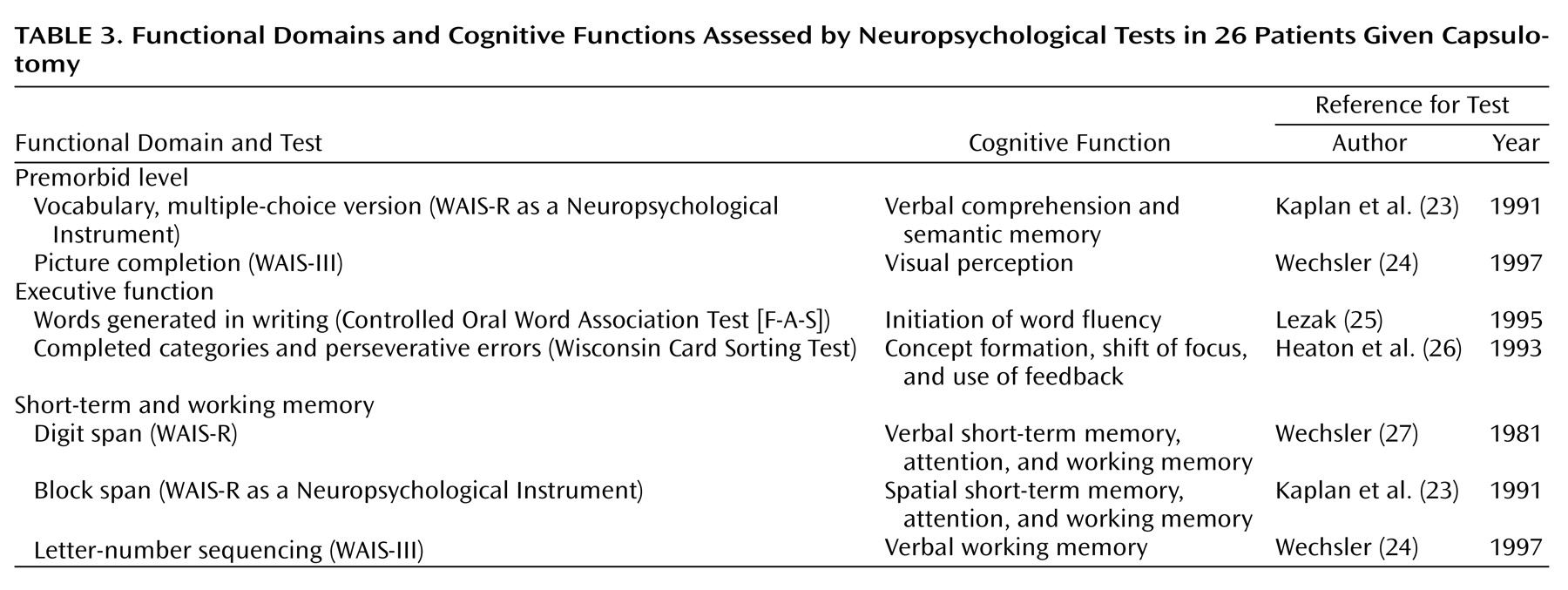
(22) were administered preoperatively and postoperatively. Results for this measure will be presented elsewhere. A battery of neuropsychological tests was applied at long-term follow-up. These tests assess premorbid cognitive function, executive functions, and short-term working memory (
Table 3).
The stereotactic CT scan that preceded the surgical procedure and served to define the coordinates for the intended lesions in the internal capsule also served as baseline examination. CT or magnetic resonance imaging (MRI) scans were obtained to confirm lesion placement in all but two patients (patients 20 and 21). At the time of long-term follow-up, 12 patients were available for a second imaging study with MRI (1.5-T GE Signa scanner [GE Medical Systems, Milwaukee]) that included standard imaging sequences (T
1, proton density, and T
2 weightings). The mean postoperative MRI follow-up duration was 13.8 years (SD=4.4, range=8–23). One of the 12 follow-up MRI data sets was lost. A well-demarcated hyperintense signal change within the anterior limb of the internal capsule on proton-weighted sequences was defined as the lesion. Lesion size and site were quantified on three anatomic levels according to the method described by Lippitz et al.
(13).
Statistical Analyses
All variables were summarized with standard descriptive statistics (frequency, mean, standard deviation, and median). For approximately normal distributions, statistical analyses of continuous variables were performed with parametric statistics (independent and dependent Student’s t test and analysis of variance for repeated measurements). Because of skewed distributions, interrater reliability for the Execution, Apathy, Disinhibition Scale ratings were calculated by the Kendall rank correlation method. If nonnormality and/or outliers were observed, nonparametric methods (Mann-Whitney test and Wilcoxon rank sum test) were applied. For discrete variables, the chi-square method and Fisher’s exact test were used.