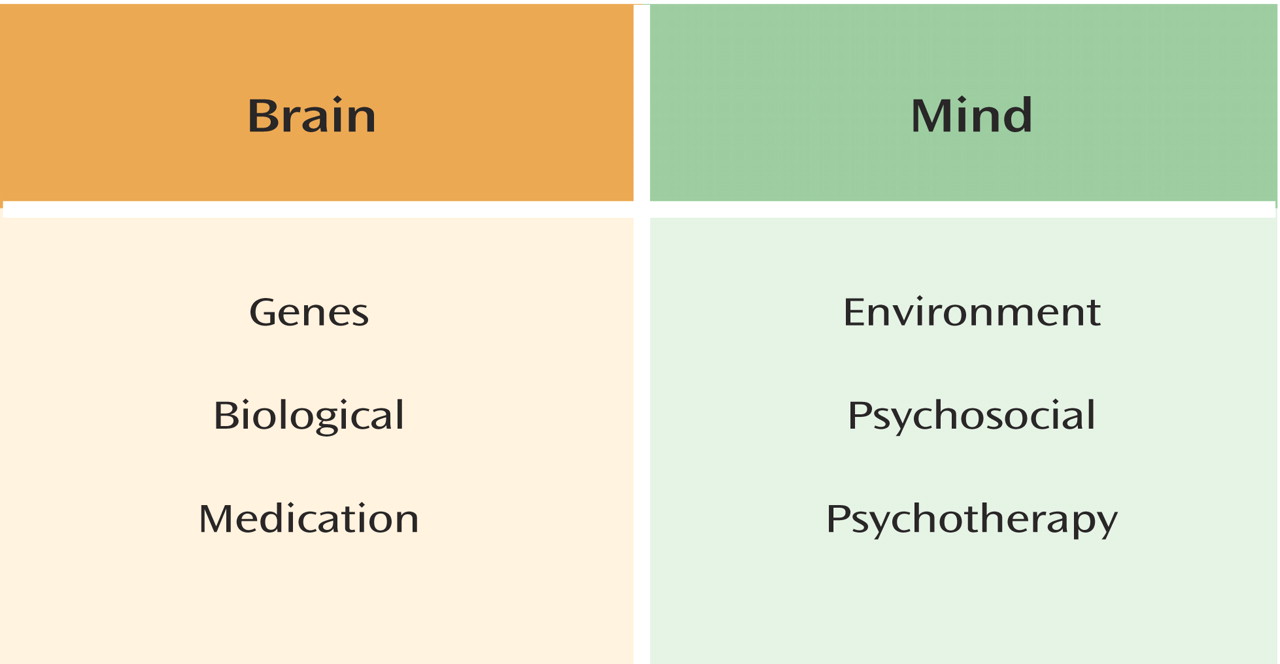
The mind-brain relationship has vexed philosophers for centuries and continues to be the subject of controversy. In psychiatric discourse, we often refer to “mind” and “brain” as though they are separate entities, even though most psychiatrists in the post-Cartesian era regard the mind as the activity of the brain
(1). The persistence of these terms in contemporary psychiatric discussions reflects the fact that references to “mind” and “brain” have become a form of code for different ways to think about patients and their treatment. As Cloninger
(2) noted, “biomedical” and “psychosocial” define two discrete paradigms, and the division into these separate models has had a stagnating effect on the science of mental health. Polarities such as genes versus environment, medication versus psychotherapy, and biological versus psychosocial are often glibly subsumed under categories of “brain” and “mind” (
Figure 1).
Using what we know about personality disorders, we can begin to deconstruct some of these problematic dichotomies while still preserving the broadly biopsychosocial framework of diagnosis and treatment that is essential to the provision of comprehensive and effective intervention for patients with these disorders. Virtually all major psychiatric disorders are complex amalgams of genetic diatheses and environmental influences. Genes and environment are inextricably connected in shaping human behavior. Experience shuts down the transcriptional function of some genes, while turning on that of others
(3). As Michael Rutter has emphasized, “Genetic influences, as they apply to individual differences in the liability to show particular behaviors, are strong and pervasive but rarely determinative”
(4, p. 996). Similarly, psychosocial stressors, such as interpersonal trauma, have profound effects of a biological nature by changing the functioning of the brain. Teasing apart biological and psychosocial phenomena may be a formidable challenge when treating a patient. Finally, to think of psychotherapy as a treatment for “psychologically based disorders” and medications as a treatment for “biological or brain-based disorders” is to make a specious distinction. The effect of psychotherapy on the brain is well established
(5).
A review of recent research on personality disorders suggests that these constructs can be dichotomized only in the abstract. In clinical work with patients, mind and brain are intimately connected and can never be separated. Nevertheless, each domain has its own language
(6). In clinical work with personality disorders, a “bilingual” psychiatrist who understands both the language of “mind” and the language of “brain” may be in a better position to develop a comprehensive biopsychosocial formulation and implement an overall treatment plan. The “theory of mind”
(7,
8) is a particularly useful bridge between the two constructs in the treatment of personality disorders, because it emphasizes the role that psychotherapy plays in creating a sense of mind in the patient.
Genes and Environment
Because of space considerations, this partial review will be limited to antisocial and borderline personality disorders, the two axis II entities with the greatest bodies of research data. Although systematic genetic studies of borderline personality disorder are in short supply, well-designed studies of antisocial personality disorder and criminality consistently show that a genetic diathesis acted on by adverse environmental experience is necessary for the development of the disorder
(9–
12). In an elegant study from New Zealand
(12), for example, a birth cohort of 1,037 children were followed prospectively and assessed at ages 3, 5, 7, 9, 11, 13, 15, 18, and 21 years. Ninety-six percent of the cohort was intact at age 26. Between the ages of 3 and 11 years, 8% experienced “severe” maltreatment, 28% experienced “probable” maltreatment, and 64% experienced no maltreatment. A functional polymorphism in the gene occurring in the neurotransmitter-metabolizing enzyme monoamine oxidase A (MAO
A) was found to moderate the effect of maltreatment. Males with the low MAO
A activity genotype who were maltreated in childhood had elevated scores on measures of antisocial behavior. Males with high MAO
A activity did not have elevated antisocial behavior scores, even when they had experienced childhood maltreatment. Eighty-five percent of males with both the low MAO
A activity genotype and severe maltreatment developed antisocial behavior. These findings suggest that genotypes moderate children’s sensitivity to environmental stressors.
Primate studies have yielded a heuristically valuable animal model that resembles human patients with a diagnosis of borderline personality disorder and antisocial personality disorder. Monkey research has also made it possible to vary specific rearing effects to gain more specific knowledge about the influence of environmental factors. Between 5% and 10% of field populations of rhesus monkeys are unusually impulsive, insensitive, and overtly aggressive in their interactions with other troop members
(13). They make dangerous leaps in trees that result in self-injury. They harass juveniles who are younger and physically weaker. They are also socially inappropriate and may self-destructively challenge a dominant adult male. Males with these characteristics are likely to be expelled from the group before puberty, while females are likely to end up at the bottom of the social hierarchy and are incompetent, neglectful mothers.
Rhesus monkeys, who share approximately 95% of their genes with human beings, also show commonalities in the linkage between impulsive aggression and measures of serotonergic metabolism
(14). An inverse relationship exists between measures of CSF 5-hydroxyindoleacetic acid (5-HIAA) concentration and measures of impulsive aggression. However, the inherited propensity to develop patterns of impulsive aggressiveness can be modified substantially by early experiences involving social attachment relationships. Monkeys reared by peers consistently demonstrate lower CSF concentrations of 5-HIAA, compared to those reared by mothers.
The serotonin transporter (5-HTT) gene has length variation in its promoter region that results in allelic variation in 5-HTT gene expression. A “short” allele (ls) confers low transcriptional efficiency to the 5-HTT promoter, relative to the “long” allele (ll), suggesting that low 5-HTT gene expression may result in decreased serotonergic function.
Bennett et al.
(15) found that CSF 5-HIAA concentrations did not differ as a function of 5-HTT status for mother-reared subjects, whereas among peer-reared monkeys, individuals with the
ls allele had significantly lower CSF 5-HIAA concentrations than those with the
ll allele. Being reared by one’s mother appeared to buffer any potential deleterious effects of the
ls allele on serotonin metabolism. Conversely, peer-reared monkeys with the
ls polymorphism exhibited much higher levels of impulsive aggression than their peer-reared counterparts with the
ll polymorphism, who exhibited low levels of impulsive aggression similar to those of both
ll and
ls mother-reared monkeys, again suggesting a buffering effect of maternal rearing.
Rhesus monkeys with low CSF concentrations of 5-HIAA are also prone to consume more alcohol in a “happy hour” situation where a 7% ethanol aspartame-flavored beverage is available
(13). Here, the data on maternal buffering effects strikingly reflect the role of environment on the influence of genes. Peer-reared monkeys with the
ls allele consumed more alcohol than peer-reared monkeys with the
ll allele. Exactly the reverse was true if the subjects were reared by mothers: the monkeys with the
ls allele had less alcohol consumption than the
ll monkeys. Investigators concluded that the short allele of the 5-HTT gene may well lead to psychopathology among rhesus monkeys who have adverse early rearing histories but could possibly be
adaptive for those monkeys who have secure early attachment relationships with their mothers
(13). Both nature and nurture appear to be at play in the development of most, if not all, of the biobehavioral aspects of rhesus monkey impulsive aggressiveness.
The implications for psychotherapy from this sophisticated understanding of gene-environment interaction are provocative. With the knowledge that genetic “hard-wiring” is a questionable assumption, we have reason to be optimistic about potential consequences of altering early parental and caregiver interactions with children.
Although randomized, controlled trials of therapy with individuals or families at risk for antisocial personality disorder have yet to be reported, a long-term follow-up study of the effect of home visitation by a public health nurse on children’s antisocial behavior
(16) is highly suggestive. The investigators randomly assigned a visiting home nurse to high-risk new mothers. The visits started during pregnancy and continued through the child’s second birthday. The comparison group consisted of mother-child pairs who received standard prenatal and well-child care in the public health clinic. Eighty-five percent of the mothers enrolled were young, unmarried, or from households with low socioeconomic status. The nurses visited an average of nine times during pregnancy and 23 times from birth through the child’s second birthday. Three aspects of maternal functioning were the focus of the home visits: health-related behaviors, competent care of children, and maternal personal development. At 15-year follow-up, adolescents born to women who had received the nurse visits had significantly lower rates of antisocial behavior, relative to the comparison subjects. They also had lower rates of substance abuse and fewer lifetime sex partners.
Results of this nature raise the possibility that early psychotherapeutic interventions might serve to influence the expression of genes that lead to antisocial behavior. A neglected benefit of individual psychotherapy is its positive effect on the
offspring of the patient. After extensively studying genetic and environmental influences on adolescent antisocial behavior, Reiss et al.
(17) made the following observation: “The encoding of genetic information into family processes might rival in importance, and serve in tandem with, the much better known process of RNA encoding—the critical intracellular transduction of genetic information on the road to protein synthesis” (p. 386). In any case, genes and environment are inextricably connected in the pathogenesis of antisocial behavior; a strict “either/or” dichotomy is specious.
The “Biological/Psychosocial” Distinction, Trauma, and Borderline Personality Disorder
The etiology of borderline personality disorder is probably multifactorial, but extensive research supports the notion that early abuse and neglect may be a significant factor in many cases
(18). Early childhood separations, chaotic home environments, insensitivity to the child’s feelings and needs, emotional discord in the family, and trauma of varying degrees have all been implicated in the etiology (see reference
18 for a review of this literature). A genetically based temperament is also probably a key factor
(19,
20). Certain temperamental predispositions may increase the likelihood that negative life events will occur. Borderline personality disorder research documenting early abuse has been controversial because much of it has relied on retrospective methods that must confront the vagaries of memory. However, an elegantly designed prospective study of 639 youths and their mothers demonstrated strong linkage between trauma and borderline personality disorder
(21). These investigators found that both neglect and sexual abuse were associated with greater symptoms of borderline personality disorder.
The effect of early trauma on the developing brain has been a subject of increasing interest in psychiatry. The hippocampus appears to be vulnerable to the effects of stress, in part because it has many glucocorticoid receptors
(22). Some imaging studies have demonstrated reduced hippocampal volume in adult patients with borderline personality disorder
(23,
24).
Preliminary data suggest that early trauma may promote hemispheric lateralization and adversely affect integration of the right and left hemispheres. Auditory-probe-evoked potential attenuation was measured as an index of hemispheric activity in 10 subjects with a history of childhood trauma and 10 matched comparison subjects without such history while they recalled a neutral memory and then a traumatic memory
(25). Abused children used their left hemisphere when thinking about neutral memories, and their right hemisphere for frightening memories. The comparison group used both left and right sides equally regardless of the memory content.
This failure of hemispheric integration may be reflected in the use of splitting as a major defense mechanism by borderline personality disorder patients. To deal with the concern that hate and aggression will destroy all positive qualities, they tend to compartmentalize self and object representations into “all good” and “all bad” categories
(26).
A growing body of research suggests that another consequence of early childhood trauma is persistent sensitization of the hypothalamic-pituitary-adrenal (HPA) axis
(27–
29). Women with a history of childhood abuse and major depression have shown a more than sixfold greater ACTH response to stress than age-matched comparison subjects
(30). The researchers concluded that a persistent consequence of childhood abuse is hyperreactivity of the HPA axis and autonomic nervous system. They inferred that this hyperreactivity was related to hypersecretion of corticotropin releasing factor (CRF).
These findings have now been confirmed in studies of patients with borderline personality disorder who had sustained childhood abuse. Rinne et al.
(31) studied 39 female borderline personality disorder patients who were given combined dexamethasone/corticotropin-releasing hormone (CRH) tests and compared with 11 healthy subjects. Twenty-four of these women had histories of sustained childhood abuse. The chronically abused borderline personality disorder patients had a significantly enhanced ACTH and cortisol response to the dexamethasone/CRH challenge, compared with nonabused subjects. The researchers concluded that a history of sustained childhood abuse is associated with hyperresponsiveness of ACTH release. Their findings suggest that this hyperreactive physiological state is relevant to a subgroup of borderline personality disorder patients, but not all. Sustained childhood abuse appears to increase the CRH receptors’ sensitivity.
Several implications can be derived from these findings. First, these data illustrate why it is problematic to lump together terms such as “genes,” “brain,” and “biological,” as though they are separate and distinct from terms such as “environment,” “mind,” and “psychosocial.” Psychosocial events may result in persisting biological alterations in the brain. Second, because the HPA axis is intimately linked with serotonergic function, these data suggest the possibility of understanding the mechanism of action of serotonin reuptake inhibitors in patients with borderline personality disorder. Third, because internal object relationships are created from the building blocks of self representations, object representations, and the affects that link the two
(32), we can infer that a hypervigilant and anxious affect state will be linked to a perception of objects as persecuting and the self as victimized. Appreciation of this internal object relationship and its affect connection may influence the clinician’s psychotherapeutic approach.
The Role of Psychotherapy: Mentalization and Theory of Mind
The capacity to mentalize, or have a “theory of mind,” involves being able to recognize that someone else has a different mind from one’s own
(33,
34). These terms also imply the ability to infer what is going on inside someone else’s mind by their facial expression, tone of voice, and other nonverbal communications. In essence, it is the ability to understand one’s own and others’ behaviors in terms of mental states such as beliefs, feelings, and motivations
(35). Inherent in mentalization are an appreciation and recognition that the perceived states of one’s self and others are fallible and subjective and are representations of reality that reflect only one of a range of possible perspectives. Mentalization is created in the context of secure attachment with a caregiver who ascribes mental states to the child, treats the child as a mental agent, and helps the child to create internal working models
(35). In other words, one automatically reads the expression on another’s face and knows what that person is feeling without extensive conscious effort to figure out the meaning of the facial expression. Hence it is not the same as conscious introspection. Neither is it identical with empathy. Mentalization refers specifically to the capacity to represent mental states of self and other. Empathy implies emotional resonance with another person. One can conceive of the mental state that may drive a person to murder without feeling empathy for that person.
In the absence of secure attachment, children have difficulty discerning their own mental states or those of others. A securely attached caregiver passes on this secure attachment and capacity to mentalize to the infant. Research has linked borderline personality disorder patients with categories of insecure attachment—either preoccupied or unresolved/disorganized attachment
(36–
39). The failure to resolve trauma appears to distinguish the borderline personality disorder group from others. Early childhood trauma leads to a defensive withdrawal from the mental world on the part of the victim. Hence some patients with borderline personality disorder who have had severe trauma cope with the abuse by avoiding reflection on the content of the caregiver’s mind, which prohibits resolution of abusive experiences
(39,
40). One patient whose mother threatened to cut her hands off when she made a mess said that she stopped thinking about why her mother yelled at her because she was afraid her mother hated her and regarded her as a monster.
Fonagy et al.
(41) studied an inpatient group that consisted predominantly of female patients with severe personality disorders. Using a reflective functioning scale that was developed to measure the capacity for mentalization
(42), Fonagy et al. were able to quantify this dimension. Ninety-seven percent of the subjects with abuse and low reflective functioning met the criteria for borderline personality disorder. However, only 17% of the subjects reporting abuse in the group who had high reflective functioning met the criteria for borderline personality disorder. Hence patients with mentalizing capacity could understand the caregiver’s mind and process what happened so as to resolve the trauma. On the other hand, those who coped with abuse by refusing to think about what was going on in the caregiver’s mind failed to mentalize and therefore could not resolve the abuse experience.
In normal development, mentalization is a psychological achievement. A child younger than age 3 years operates primarily in a psychic equivalence mode
(33). In this mode, the child assumes that perceptions of reality are identical to the reality itself. Around age 4 or 5 years, the child begins to integrate the pretend mode with the psychic equivalence mode of thinking. The 5- or 6-year-old child understands that one’s perception is influenced by subjective factors. This understanding allows for the phenomenon of play, where a child and a playmate can pretend to be others and perceive each other in those roles even though they are aware that the perception is different from the reality. Patients with borderline personality disorder often have great difficulty shifting from the psychic equivalence mode to the pretend mode, and this difficulty interferes with their capacity to recognize transference in psychotherapy. They often hold on to their perception as an absolute fact rather than viewing it as one of several possible alternatives, as the following case vignette illustrates:
Ms. A was a 28-year-old patient with borderline personality disorder in dynamic psychotherapy. About 6 months into the process, an apparently minor event in the therapy session triggered a major reaction in Ms. A. With about 5 minutes left in the therapy session, Ms. A was talking about having visited her family during the Thanksgiving holidays. She felt unimportant to her father because he seemed much more interested in her brother’s activities than in hers. In the course of this discussion, I looked at the clock on my wall because I knew the time was running out and I wanted to see if I had time to make an observation about her assumption regarding her father’s feelings about her. Ms. A stopped talking and looked at the floor. I asked her what was wrong. After a few seconds of silence, she burst into tears and said, “You can’t wait for me to get out of your office! I’m sorry if I’m boring you! I’ve known for a long time that you can’t stand me, and you just do this for the money. I’ll leave now if you want me to.” I was taken aback and replied, somewhat defensively, that I was simply monitoring the time because I wanted to be sure I had time to say something before the session was over. Ms. A replied by saying, “Nice try to get out of it. You think I’m going to believe that?” Escalating in my defensiveness, I stated emphatically, “Whether you believe it or not, that’s the truth.” Ms. A was adamant: “I saw what I saw.” Placing her hand firmly on the wooden table next to her chair, she raised her voice: “It’s like you’re telling me that this table is not made out of wood!” Feeling as misunderstood as she was, I continued: “All I’m saying is this: it’s possible that I looked at the clock for reasons other than the ones you attribute to me—just like you may make assumptions about your Dad.” Ms. A became even more insistent in response to my efforts to offer other possibilities: “Now you’re trying to say I didn’t see what I saw! At least you could admit it!”
One of the greatest challenges for a psychotherapist is managing this almost delusional conviction of some patients with borderline personality disorder that their perception is a direct reflection of reality rather than a representation of reality based on their internal beliefs, feelings, and past experiences. This failure to mentalize may make it extremely difficult for them to work on transference issues because they are convinced that their view of the therapist is “correct” rather than one of a number of possible interpretations of the therapist’s behavior, facial expression, or comments. Fortunately, mentalization occurs on a continuum, and at times patients with borderline personality disorder may be capable of entering the pretend mode and reflecting on their own internal world and that of others. Whereas states such as autism are characterized by complete absence of mentalization on a neurological basis, a patient with borderline personality disorder often retains partial ability to mentalize under some circumstances, particularly when there is not an affectively intense involvement in an attachment relationship.
This vignette reflects how the misreading of the therapist’s mind led to an activation of a trauma-based internal object relationship associated with a hyperreactive HPA axis. I became a potentially malevolent persecuting object; she became a victimized self; and a hypervigilant, anxious, humiliated affect state linked self and object. In this state of feeling terrorized, one cannot think or reflect. The intensity of Ms. A’s accusation also eroded
my capacity to think, and I escalated my defensiveness to the point where I actually
became a version of the persecuting object that she feared. This projective identification process, where the therapist is coerced under pressure from the patient into playing a role in the patient’s internal drama, can cause therapists to temporarily lose their capacity for mentalization, such that they cannot think their own thoughts in a psychotherapeutic role
(43). In other words, I was insisting that only my version of reality was valid. Patients with borderline personality disorder colonize the minds of others as a way of extruding and controlling perceived danger from within. They unconsciously coerce the therapist into taking on the characteristics of an abusive internal object. I had become “bad” in two senses of the word—a bad object and a bad therapist. Although my interpretation that Ms. A’s misreading of me was similar to her misreading of her father may have been accurate, my timing was poor. Neither the patient nor I was in a reflective state of mind where meanings could be entertained. Our research in the Menninger Clinic Treatment Interventions Project
(44) found that transference interpretation may need to be postponed under such circumstances until the patient’s ability to reflect returns.
Neural imaging studies suggest that mentalization entails several different brain structures working in concert
(45–
49). Most of these studies involved asking the subject to perform mental activities that require an understanding of someone else’s inner world. Recently Calarge et al.
(48) asked 13 healthy volunteers to place themselves in another person’s place and attribute mental states to that person by having them describe the experience of a crying stranger met during a chance encounter on a park bench. The authors noted that these capacities are necessary in psychodynamic psychotherapy practice. As in other studies, the medial frontal region was activated when the subjects attributed mental states to others. One of the most significant findings was that the largest activation during the task occurred in the right cerebellum. Like Frith and Frith
(45), these investigators suggested that it is best to think of a “theory of mind” system or network that is widely distributed and made up of interactive nodes, probably in the medial prefrontal regions, the superior temporal sulcus, the inferior frontal region, and the cerebellum.
Mirror neurons may also play a role in a neurobiological basis understanding of mentalization. These neurons in the premotor cortex, first identified in monkey studies, respond when a primate observes certain hand movements performed by another primate or by a human or when the animal performs the same movements itself. In other words, these neurons are encoding object-oriented actions, whether they are performed or observed. This group of neurons in the ventral premotor cortex is activated during observation of an agent acting in a purposeful way upon objects
(50). Fogassi and Gallese
(50) suggested that mirror neurons may have a crucial role in goal detection and therefore in action understanding. They point out that the “mind reading” associated with theory of mind studies involves a series of explicit behavioral signals. They proposed that the capacity to understand another person’s internal world is related to the activation of this shared representation through mirror neurons. In other words, these neurons recognize intrinsically meaningful behavioral signals.
The fact that certain brain areas are activated during theory of mind experiments does not help the psychotherapist much when a patient with borderline personality disorder is sitting in the consulting room. However, the theory of mind construct helps bridge the domains of brain and mind. Within this conceptual model, mind becomes a sense of a subjective internal world accompanied by the recognition that others have internal worlds different from our own. There is no resort to Cartesian dualism in this model, but there is a recognition that subjectivity is extraordinarily complex and involves a language of meanings, perceptions, feelings, intentions, beliefs, and motivations that are not readily reducible to neuroscience constructs. Although the brain is an objective, observable entity, the mind of another is known through empathic connection. The vocabulary of the psychotherapist draws on the lexicon of the mind. To create a “mind” in the patient with borderline personality disorder requires the language of the mind.
Treatment Implications
The American Psychiatric Association (APA) practice guideline for the treatment of borderline personality disorder
(51) suggests that a combination of psychotherapy and medication is the optimal treatment approach. Even though no randomized, controlled trials have compared medication alone with this combination or psychotherapy alone with this combination, the conventional wisdom is that medication may facilitate the psychotherapy of borderline personality disorder patients. The research reviewed earlier suggests ways in which medication and psychotherapy may work synergistically in the subgroup of patients with borderline personality disorder who have severe early trauma. The APA guideline notes that both dialectical behavior therapy and psychoanalytic/psychodynamic therapy are helpful for patients with borderline personality disorder. Here, I will confine my comments to the latter.
The findings of four double-blind, placebo-controlled trials
(52–
55) suggest that patients with serious personality disorders (principally borderline personality disorder) respond to optimal dosages of selective serotonin reuptake inhibitors (SSRIs) with improvements in anger, impulsive aggressive behavior (particularly verbal aggression), and affective lability. These agents may facilitate psychotherapy by reducing “affective noise”—such as intense anger, hypervigilant anxiety, or dysphoria—that prevents patients from reflecting on their internal world and the inner experiences of others. There is also growing evidence that SSRIs may actually stimulate neurogenesis, particularly in the hippocampus, leading to improved verbal declarative memory
(56). In addition, SSRIs may reduce the hyperreactivity of the HPA axis by reducing hypersecretion of CRF. Nemeroff and Owens
(57) reported that in rats, paroxetine reduces the increase in CRF mRNA expression after 3 weeks. As a result, CRF concentration and the increased HPA axis response to stress secondary to early life trauma are also reduced. When treatment with paroxetine stops, these same indices return to their usual abnormal values.
Rinne et al.
(58) studied the effect of fluvoxamine on the HPA axis in 30 female patients with borderline personality disorder. They were given a combined dexamethasone/CRH hormone test. The test was administered before and after treatment with 150 mg/day of fluvoxamine. Seventeen of the patients had a history of sustained childhood abuse, and 13 had no abuse history. Both 6 and 12 weeks of fluvoxamine treatment were associated with a significant reduction of ACTH and cortisol response to the dexamethasone/CRH test. The magnitude of the reduction was directly related to the presence of sustained childhood abuse but not dependent on the presence of comorbid posttraumatic stress disorder or major depression. The investigators concluded that fluvoxamine reduces HPA hyperresponsiveness in borderline personality disorder patients who have a history of sustained childhood abuse.
The reduction of HPA axis hyperresponsiveness may directly affect the patient’s capacity to reflect. As noted earlier, the hypervigilant, anxious affective state is linked to a specific object relations unit in the patient that involves the perception of others as potentially malevolent persecutors and the self as a victim. In the state of being terrorized, one cannot think clearly. One can only react. Turning down the hyperreactivity with an SSRI facilitates thinking and reflecting. Without the intense affective state that existed before treatment with the SSRI, the patient can more easily consider other motives in the therapist. The patient can also have the luxury of reflecting on his or her own internal state. The patient can begin to see the therapist as someone there to help rather than persecute. Similarly, when the hypervigilant state in the patient is reduced, the therapist’s capacity to think psychotherapeutically is less likely to be eroded. When the therapist is on the defensive, as in the case reported earlier, defending oneself may become more prominent than working psychotherapeutically. Indeed, through projective identification the therapist develops a mental state that is similar to the patient’s
(43,
59).
Use of an SSRI may help facilitate psychotherapeutic changes in the brain. The patient’s capacity to perceive the therapist as a helpful and caring figure instead of a persecuting and malevolent figure will serve to build up new neural networks of internal representations while weakening the old ones
(60). Splitting may be reduced as well, because lowered anxiety makes the defense less necessary. Hence better integration of left and right hemispheres may be promoted. Findings from a pilot study in Finland
(61) that used single proton emission computed tomography imaging suggested that psychotherapy may even alter serotonergic metabolism in borderline personality disorder. Kandel
(3) has emphasized that psychotherapy should be regarded as a “biological” treatment in that it leads to anatomical changes at the microcellular level.
These therapeutic changes take time. There is no “quick fix” for borderline personality disorder. Research in which this mentalization-based psychotherapeutic approach was used in conjunction with medication in a day hospital program indicated that it is highly efficacious but requires at least 12 months
(62). However, the time investment is well worth it. A follow-up assessment at 18 months found that patients continue to make improvements after the therapy ends
(63). The duration of treatment necessary in less intensive outpatient treatment will require further study.
In conclusion, personality disorders are best understood and treated without “either-or” dichotomies of brain and mind. Environmental influences on genes make nature-nurture distinctions difficult. Psychosocial factors produce biological changes in the brain. Medication and psychotherapy work synergistically to make changes in the brain over time. The languages of “brain” and “mind” are both necessary in the treatment of personality disorders. The language of “mind” is necessary for psychotherapy, but its effect is on the brain as well as on the creation of a “theory of mind” in the patient. Nemeroff et al.
(64) found that psychotherapy is essential in the treatment of patients with chronic forms of major depression and a history of childhood trauma. The same is probably true for traumatized patients with borderline personality disorder. The model described here is applicable primarily to the subgroup of borderline personality disorder patients with childhood abuse and neglect. Further research is needed to identify models for those without that history.