Measures
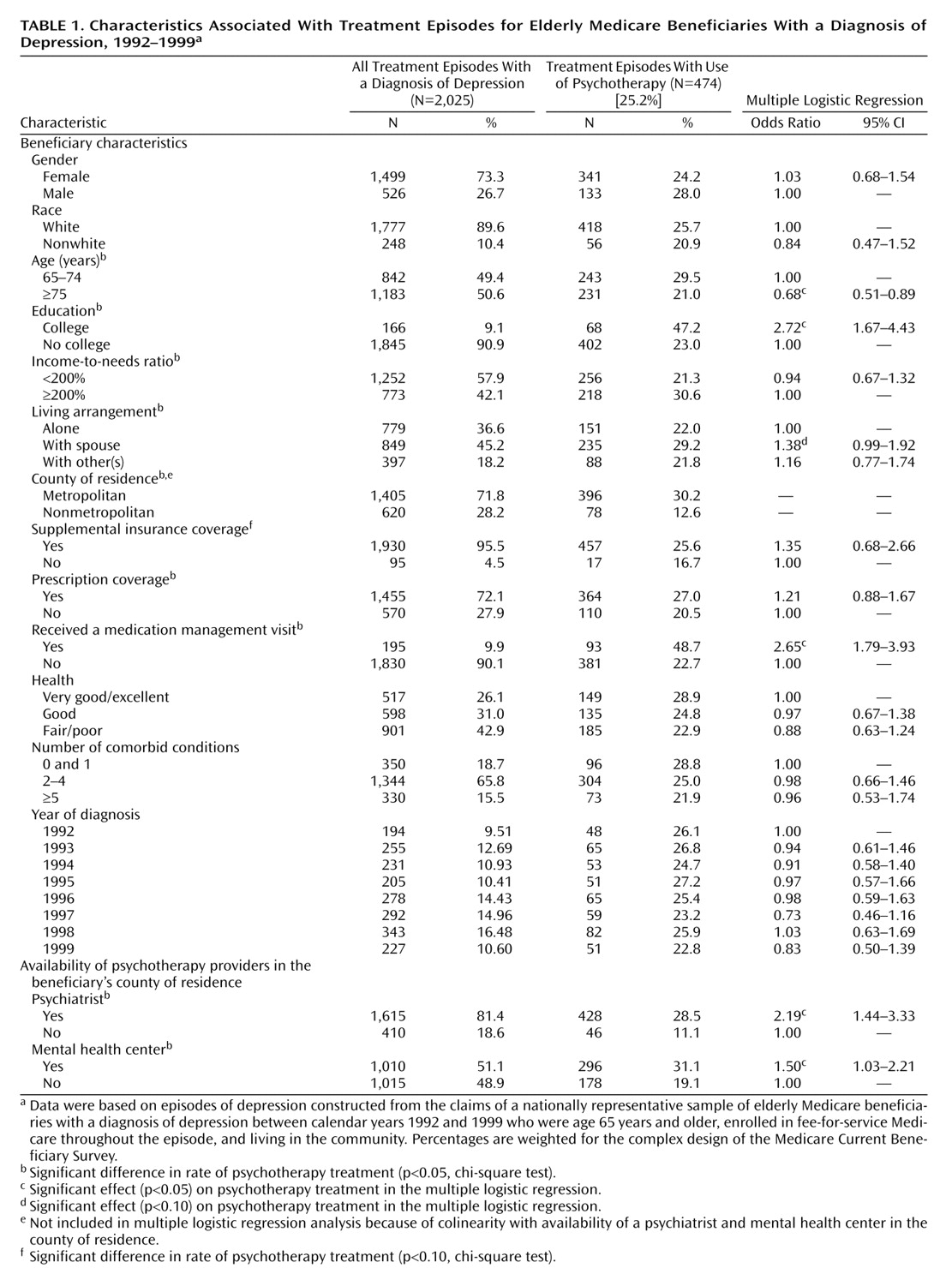
Depression diagnosis was identified through ICD-9-CM/DSM-IV diagnosis codes (296.2, 296.3, 300.4, and 311) recorded in the Medicare claim files. On the basis of our episode-of-care approach, the sampling criteria captured 2,025 episodes.
Use of psychotherapy was identified by using physician’s current procedure terminology (Physician’s Current Procedural Terminology, 4th ed. [CPT-4]) and Health Care Financing Administration Common Procedure Coding System codes in the Medicare physician/supply claims. Psychotherapy was defined broadly, by using codes in the range from 90841 to 90857 for 1992 through 1999. In addition, codes ranging from H5010 to H5025 were included for 1992–1997 data; codes 90875, 90876, and 90880 were included for 1993–1999 data; and codes ranging from G0071 to G0094 were included for 1997–1999 data.
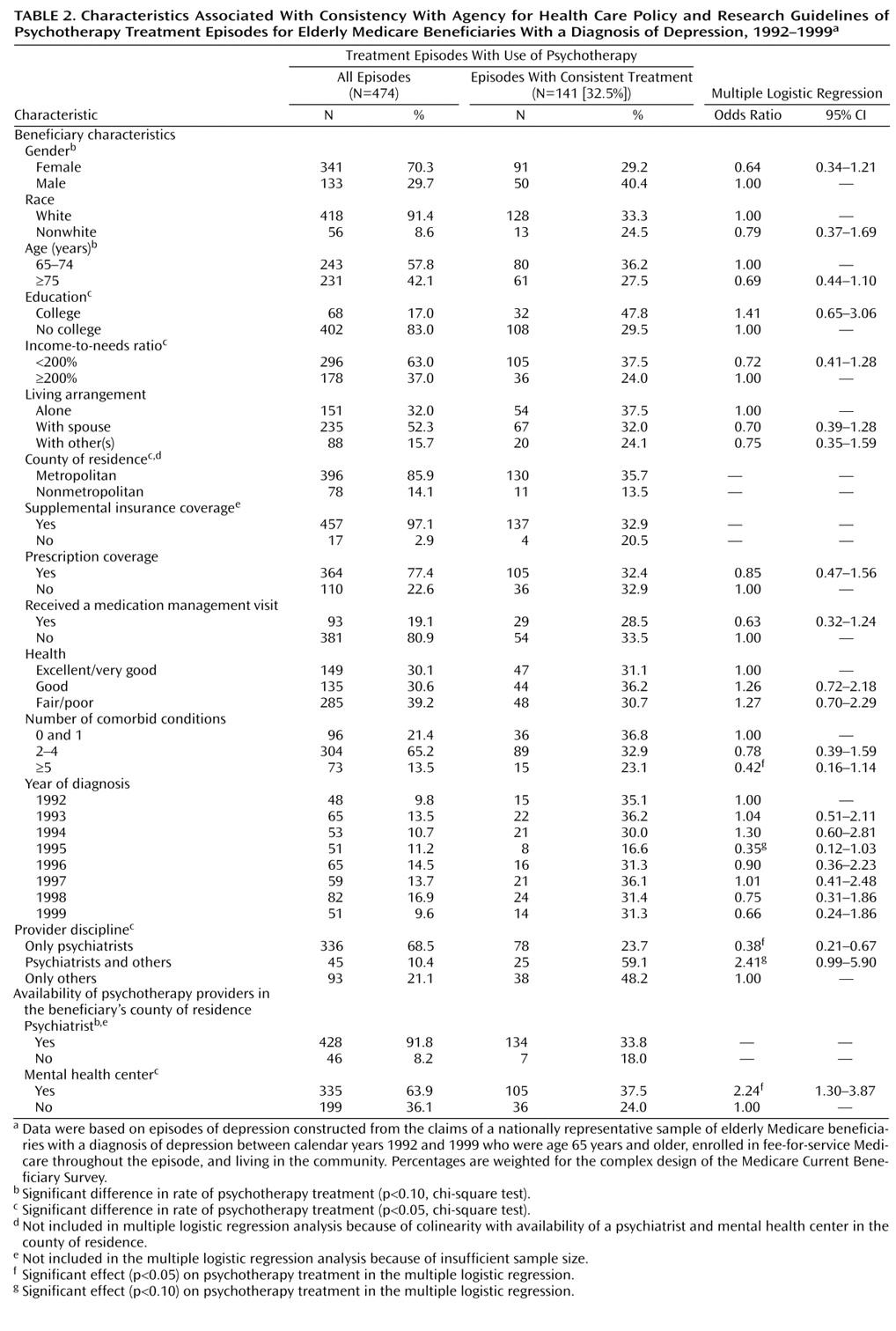
Guidelines recommend that treatment for major depression continue for 4–9 months
(20). Therefore, we defined consistent psychotherapy use as extending for at least two-thirds of the total months of an episode.
Demographic characteristics included gender, age, race, and living arrangement. Patients were categorized into two groups on the basis of age: 65–74 years, and 75 years and older. Race was classified as white versus nonwhite. Living arrangements were categorized as living alone, living with spouse, and living with others.
Economic characteristics included education, poverty status, pharmacy coverage, and supplemental insurance coverage. On the basis of completed years of schooling, education was categorized as no college or college. “Low income” was defined as the respondent’s personal income, or joint income if married, below 200% of the family-size-adjusted federal poverty level
(24). Type of prescription drug insurance coverage was derived from survey responses about monthly drug coverage and included five possible types of private plans, Medicaid, and other public plans. A supplemental insurance variable was created to indicate whether the individual was covered for at least 1 month under any of the following insurance plans: private plans, other public plans, health maintenance organization (HMO) coverage, Medicaid, and Qualified Medicare Beneficiary/Specified Low-Income Medicare Beneficiary coverage.
Environmental variables included characteristics of the health care delivery system, external environment, and community. Person-level area of residence was classified as living in or near “metropolitan” areas versus “nonmetropolitan” areas. Two binary variables were created from Area Resource File data to measure availability of a psychiatrist and a mental health center in the county where the patient lived.
Health care professionals who treated patients during the psychotherapy treatment episodes were categorized by clinical specialty: only psychiatrists, psychiatrists and others, and only others. Other health care professionals included psychologists, social workers, and general practitioners.
Previous studies have suggested that treatment with antidepressant medications increases responsiveness, motivation, and accessibility to psychotherapy
(25,
26). We defined medication management visits (
CPT-4 code 90862) as those including no more than minimal medical psychotherapy.
Health status variables included self-perceived health and number of comorbid conditions. Both are ordinal variables, and higher values imply lower health status. Health perceptions were classified as 1) excellent or very good, 2) good, and 3) fair or poor. The number of comorbid conditions was measured by respondents’ self-reports about whether they had ever been told by a doctor that they had heart disease, diabetes, cancer, stroke, arthritis, hypertension, emphysema, osteoporosis, or Alzheimer’s disease. The number of comorbid conditions was categorized into three groups: 1) none to one, 2) two to four, and 3) five or more.
Year of diagnosis was included to account for changes in available treatments and practice patterns, with 1992 as the reference year.