The literature on suicide demonstrates, on the basis of adoption, twin, and family studies, that suicidal behavior aggregates in families and that the familial transmission of suicidal behavior cannot be explained by the transmission of major psychiatric disorders alone
(1) . However, nearly all of these family genetic studies are cross-sectional, which means that little is known about the precursors of suicidal behavior that place offspring of suicidal individuals at increased risk of suicidal behavior and the causal models to explain how suicidal behavior is transmitted from parent to child.
Nevertheless, the literature provides clues as to the mechanisms and precursors of familial transmission of suicidal behavior. Longitudinal community studies show that precursors of youthful suicidal behavior include depression, suicidal ideation, behavioral symptoms, child maltreatment, and family history of suicidal behavior
(2 –
4) . Cross-sectional studies have shown that the familial aggregation for suicidal behavior is related to the trait of impulsive aggression. Higher levels of impulsive aggression in those who attempt or compete suicide are associated with greater family aggregation for suicidal behavior
(5,
6), and higher levels of impulsive aggression in parents are associated with child suicidal behavior
(7) . In one cross-sectional study, the familial transmission of suicidal behavior appeared to be mediated by the transmission of impulsive aggression from parent to child
(8) .
Another factor identified as a potential precursor of child suicidal behavior is a parental history of child sexual abuse
(8,
9) . Because parental sexual abuse is related to so many other factors that might affect suicidal risk in the child, such as parental aggression, mood disorder, posttraumatic stress disorder, borderline personality disorder, and substance abuse
(3,
10,
11), the salience of parental history of abuse in predicting child-onset suicidal behavior requires clarification from longitudinal studies.
An understanding of the precursors of suicidal behavior in youths is important for the treatment and prevention of suicidal behavior in this population. Moreover, suicidal behavior is recurrent, and it is the single most significant risk factor for completed suicide, both on the basis of longitudinal and case-control psychological autopsy studies
(13,
14) . The identification of precursors of suicidal behavior is the goal of our ongoing two-site longitudinal study comparing the risk and predictors of suicidal behavior in the offspring of parents with mood disorders. Our previously published cross-sectional results
(7) indicated a sixfold increase in risk of suicide attempt in the offspring of suicide attempters compared with nonattempters, and impulsive aggression and sexual abuse in parent and offspring as well as mood disorder in the offspring were significant correlates of suicidal behavior in offspring. We now report the results of our longitudinal follow-up of up to 6 years. We hypothesized that the variables associated with suicidal behavior in offspring in cross-sectional analyses would also predict incident attempts in offspring.
Method
Sample
The sample in this study was drawn from 400 offspring of 212 probands with mood disorders. Just over half (54.2%) of the probands had a history of a suicide attempt. The majority of probands were recruited from inpatient units at Western Psychiatric Institute and Clinic in Pittsburgh and at New York State Psychiatric Institute in New York City. Cross-sectional analyses of a subset of this sample at intake into the study have been reported previously
(7 –
9) .
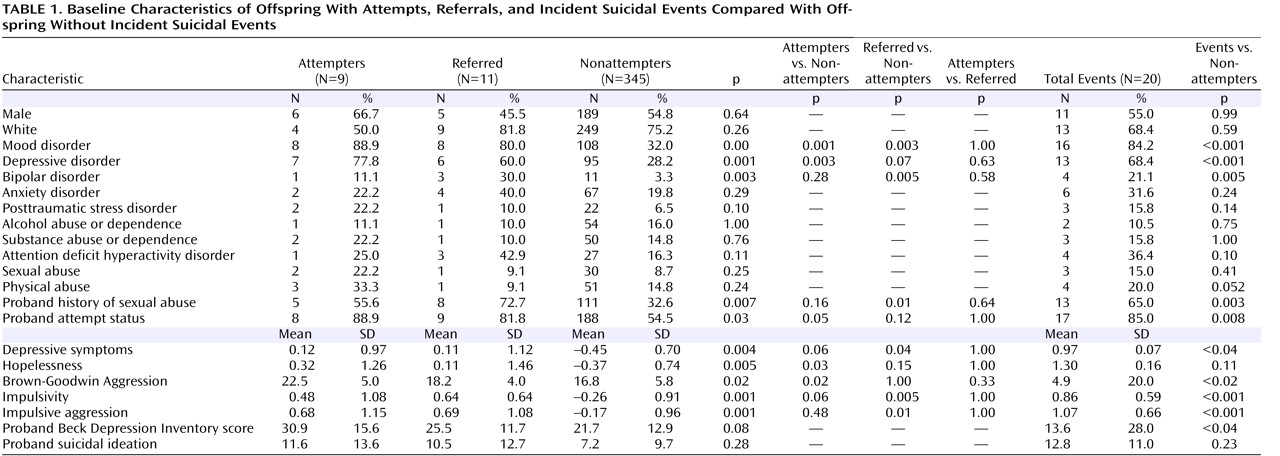
The primary outcome measure in this analysis was a suicidal event in offspring—either a new-onset suicide attempt or suicidal ideation resulting in either an emergency referral or a major change in treatment (such as hospitalization or a change in medication). A suicide attempt was defined as “a self-destructive act with at least either expressed or inferred intent to die.” A consensus group representing both study sites reviewed all attempts and emergency referrals for suicidal ideation. The emergency referral group was more similar to the attempter group than to the nonattempter group (see
Table 1 ). For simplicity, we refer to attempts and referrals as “suicidal events.”
Since the focus of this article is on the predictors of new-onset events, we excluded 35 offspring who had already made a suicide attempt or had an emergency referral by the time of entry into the study. The characteristics of those with a history of suicidal behavior were similar to those who developed suicidal events during follow-up in all demographic and clinical domains except three: those who had suicidal events at intake, compared with those who developed incident suicidal events, were more likely to be female, to have a history of sexual abuse, and to have had an earlier onset of suicidal behavior.
With those 35 excluded, we report the results for a total of 365 offspring who were followed a mean of 2.4 years (SD=1.3, range=1–6) or 857 total person-years. This offspring sample was almost equally distributed by gender (48.3% female) and was mostly in the young adult age range (mean age=20.2 years, SD=9.0 years). The majority of the offspring (75%) were white. As for probands (N=203), the majority were female (84%), in midlife (mean age=46 years, SD=10.5), white (75%), and with an average annual household income between $30,000 and $40,000.
Assessment
Recruitment of participants and the informed consent or assent process were conducted in accordance with the guidelines of the institutional review boards of University of Pittsburgh School of Medicine and New York State Psychiatric Institute, both of which approved the study. A direct interview was conducted with probands and offspring participating in the study at intake and at yearly follow-ups. For participants age 18 and older, lifetime and current axis I disorders were ascertained with the Structured Clinical Interview for DSM-IV
(15), and for those under 18, the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version
(16) . Axis II disorders were assessed at intake in participants over age 14 with the Structured Clinical Interview for DSM-IV Personality Disorders
(17) . At each assessment point, information about onset, offset, and presence of psychiatric disorder since the last evaluation was ascertained.
The history of suicidal behavior was assessed with the Columbia University Suicide History Form and the Medical Damage Lethality Rating Scale
(18) . Suicidal ideation was assessed with the Scale for Suicide Ideation
(19) . Aggression was assessed at intake with the intake and follow-up versions of the 11-item Brown-Goodwin Lifetime History of Aggression
(20) . A history of physical or sexual abuse was assessed in adults and children with screens from the posttraumatic stress disorder section of the psychiatric interview and the Abuse Dimensions Inventory
(21) .
In addition to the direct interview, a battery of self-report measures was administered. The Buss-Durkee Hostility Inventory
(22), a self-report measure of impulsive aggression, was administered in subjects 14 years of age or older. The Children’s Hostility Inventory
(23), a downward extension of the Buss-Durkee inventory, was administered in children younger than 14 years. Impulsivity was assessed with the Barratt Impulsivity Scale
(24) in participants age 18 or older, and the impulsivity subscale of the Emotionality, Activity, Sociability, and Impulsivity
(25) scale in those under age 18. Depressive symptoms and hopelessness were assessed with the Beck Depression Inventory (BDI)
(26) and the Beck Hopelessness Scale
(27) . Intercurrent negative life events were assessed with the Lewinsohn et al. shortened version of the Social Readjustment Rating Scale
(28) in those over age 18 and the Life Events Checklist
(29) for offspring under age 18. When different measures to assess the same domain were used for children and adults, standardized scores were computed to allow for comparisons across the life span.
Statistical Analysis
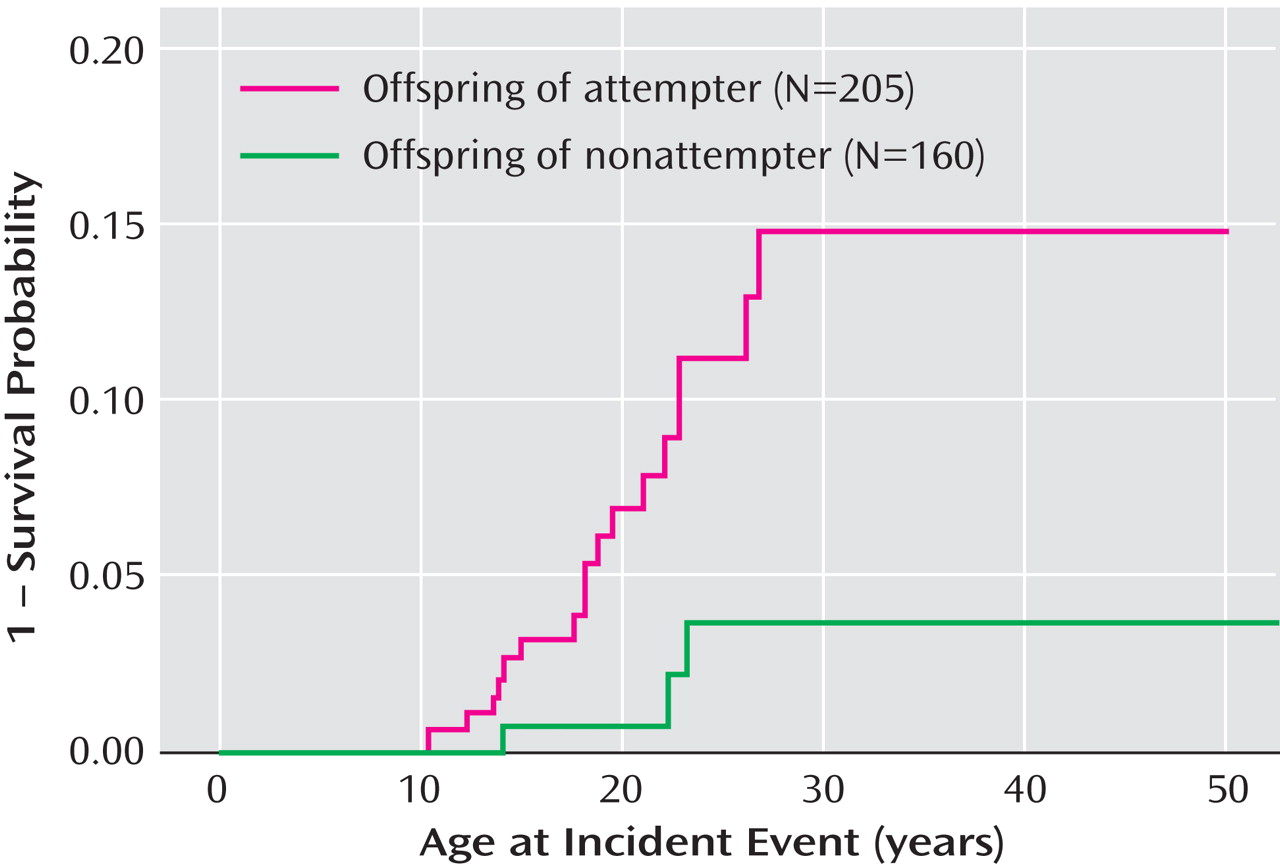
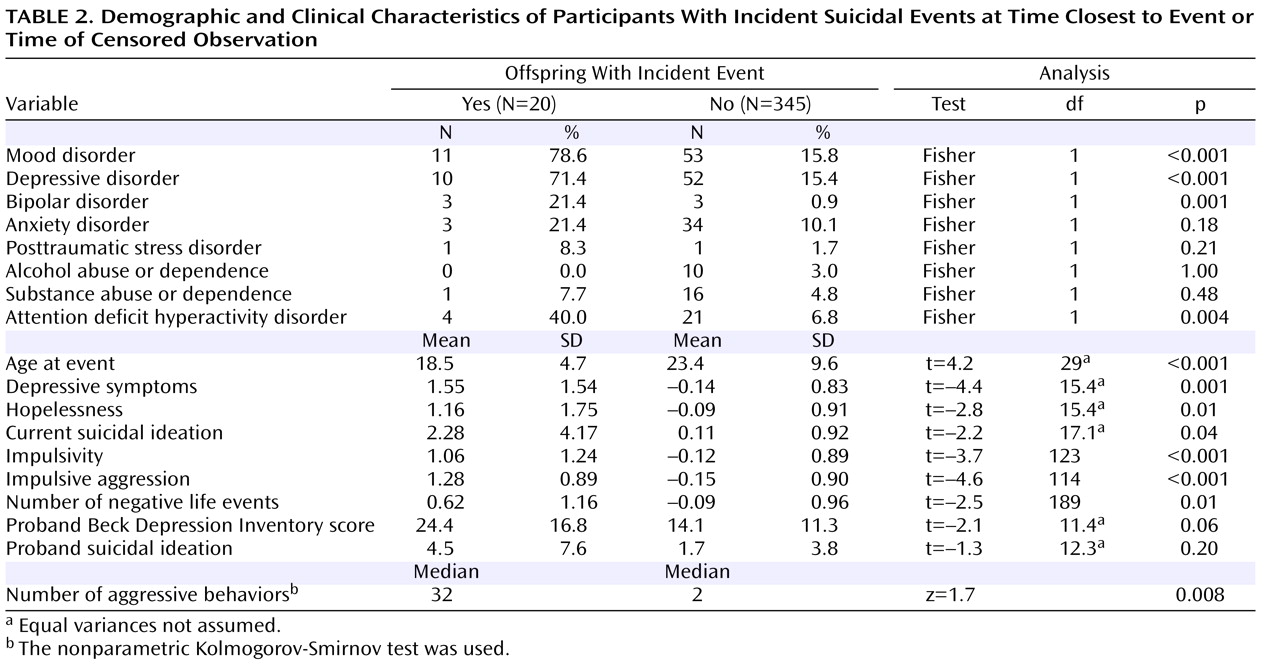
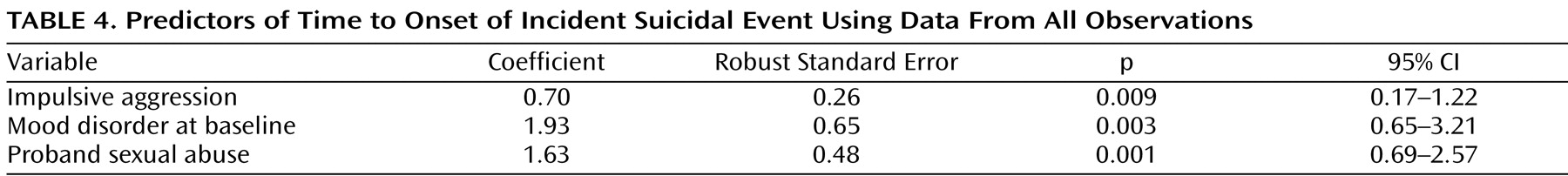
We compared offspring of proband attempters and offspring of proband nonattempters on suicidal event incidence rate using relative risk and the time to onset of an incident event using Kaplan-Meier survival analysis. The equality of survival functions was tested using the Wilcoxon and log-rank tests. We then compared participants with an incident suicidal event to those without an event or a lifetime history of such an event on demographic characteristics and clinical characteristics at baseline and at the time of the event or of censored observations. We used standard parametric and nonparametric univariate statistics and logistic regression to identify the most parsimonious set of variables that were related to incident events.
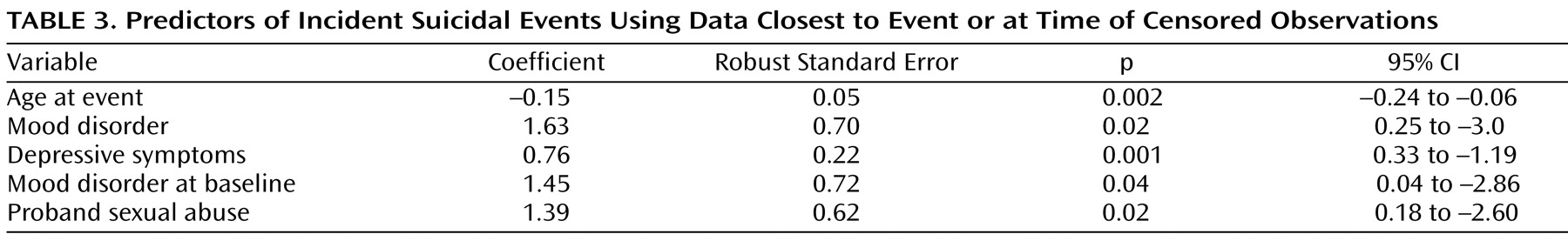
We examined predictors of suicidal events, including baseline characteristics as one set of predictors, using measures obtained at the time closest to the event or time of censored observation (for those who did not have an event); using the most severe observation for each predictor; and using all observations and taking the mean of a measure over all time points. For diagnoses, we examined the proportion of time the subject was in an episode of a specific disorder during the period of observation. Similar predictors were obtained using the three approaches. Thus, we report only on the predictors of incident events at baseline and at time closest to event. For predictors of time to onset of an event, we used all observations and the most severe observation.
After identifying characteristics that were significantly associated with new-onset suicidal events, we used multivariate analysis to identify the most important predictors. Because of the longitudinal nature of this study, there were missing data for different predictors. For the list of variables significantly associated with new-onset suicidal events, 17% of the sample had no missing data for any variable, 31% had missing data for one or two variables, 43% had missing data for three or four variables, and 9% had missing data for more than four variables. We used the multiple imputation by chained equations technique
(30) in Stata release 8.2 (Stata Corp, College Station, Tex., 2004), which is based on each conditional density of a variable, given all other variables, and does not require that the multivariate joint normal distribution assumption be met. It allows the conjoint imputation of variables based on a set of predictor variables by an appropriate regression model (ordinary least squares, logit, etc.). We used the multiple imputation approach with an inclusive strategy, as recommended by Collins et al.
(31), which makes use of auxiliary variables that are correlates of missingness and/or correlates of the variable of interest, to improve the missing data procedure. This approach reduces the chances of inadvertently omitting an important cause of missingness and provides noticeable gains in terms of increased efficiency and reduced bias. Multiple imputed data sets were created and combined using the “micombine” command for regression analysis. Convergence was observed after five imputations. Since multiple offspring per family were recruited, we controlled for the potential cluster effect in the regression analysis. Logistic regression was used to identify predictors of suicidal events, and Cox regression analysis was used to examine predictors of time to an event. Logistic regression yields an odds ratio rather than a risk ratio, even in a cohort study. However, when the incidence of an outcome measure of interest in the study population is low (<10%), which was the case for our outcome measure, the odds ratio approximates the risk ratio
(32) .
Discussion
This is one of the first prospective studies to examine risk factors for suicide attempt in youths at high risk of a suicide attempt by virtue of family history. We found that offspring of suicide attempters were much more likely to experience a suicidal event on follow-up compared with offspring of nonattempters. The risk factors for an incident suicidal event were similar to those reported in previous cross-sectional and retrospective analyses, namely, mood disorder and impulsive aggression in offspring and parental history of sexual abuse, suicide attempt, and self-reported depression.
Before discussing the implications of this study, we place them in the context of the limitations of our study design. The main limitation is that even in a high-risk sample, suicidal events were relatively rare, which provides limited power to detect effects that are less than moderate. However, our rate of incident events (5.4%) is similar to the 4.5% lifetime prevalence of suicide attempts in a community sample of adolescents
(12) and the 7.1% rate during ages 14–21 years in an unselected birth cohort in New Zealand
(2) . In addition, the number of events (N=20) was similar to the number of events we found in our first cross-sectional analysis of this sample
(7) . The findings are not likely to be spurious, because they are consistent with our own cross-sectional analyses as well as findings in the literature
(2,
7,
33) and because they are consistent across complementary analytic approaches.
A second possible limitation is the inclusion of emergency referrals for suicidal ideation along with suicide attempts as our outcome measure. In conducting a study with participants at high risk of suicidal ideation or behavior, researchers are obligated to treat or refer those who are in a suicidal crisis to avert a suicide attempt. Participants in this study who were referred expressed ideation with high intent or a suicidal plan, and epidemiological studies show that as many as 90% of unplanned first attempts and 60% of planned first attempts occur within 1 year of the onset of suicidal ideation
(34) . This approach has a precedent in the InterSePT study
(35), which compared the differential outcome with regard to suicide attempts and suicidal events in schizophrenia patients at high risk of suicidal behavior who were treated with either clozapine or olanzapine. Moreover, the similarity of characteristics of those who had emergency referrals for suicidal ideation to those who had an attempt supports the use of both referrals and attempts as an outcome measure.
A third important limitation is that demonstration of familial aggregation or transmission is not the same as demonstration of a genetic etiology, as there can be family environmental factors that are transmitted from parent to child but are not genetic. However, the main advantage of a prospective design with high-risk participants is that, without knowing etiology, one can still find the precursors for suicidal behavior and their sequence and interrelationships, which in turn can be informative to both etiological and intervention studies.
Our finding that parental attempt confers a markedly increased risk of future suicidal events in a referred sample is consistent with, and on the same order of magnitude as, our initial cross-sectional analyses of this sample as well as a similar prospective study conducted with a community sample
(7,
12) . Moreover, our prospective validation of earlier cross-sectional findings allows us to identify families whose children are at high risk of suicidal behavior.
These results may also have important implications for the treatment of suicidal youths, who are often depressed. Depressive disorder, particularly chronic or recurrent depression, consistent with other clinical and epidemiological studies of attempted and completed suicide, also emerged as a risk factor for suicide attempt
(36,
37) . Prevention of early-onset depression in high-risk youths may also help reduce the overall public health burden of early-onset suicidal behavior.
Our findings also suggest, however, that the risk of suicide attempt is multifactorial and that while treatment of depression is necessary, treatment strategies that only target depression may not be sufficient to reduce suicidal risk. Other factors, such as impulsive aggression and parental history of sexual abuse, also contribute to suicidal risk. As has been emphasized in previous studies of adults, the assessment and management of impulsive aggression is likely to be critical to the prevention of onset or recurrence of suicidal behavior
(38) . Neurocognitive tests of impulsivity and emotion regulation may be helpful in further clarifying the phenotype of early-onset suicidal behavior. In adults, psychosocial and pharmacological interventions that increase emotion regulation and decrease impulsive aggression are among the only interventions that diminish the risk of reattempt
(38) . Similar approaches should be considered for adolescent suicide attempters.
The finding of such a prominent role for parental history of sexual abuse in youth suicide was not predicted before we began this longitudinal study. A history of sexual abuse in the parent appears to increase the risk of mood disorder and suicide attempt in the child by increasing the risk that the child will also experience abuse as well as by increasing offspring impulsive aggression, according to our previous cross-sectional analyses
(8) . Parental sexual abuse may also increase the risk of suicide attempt in offspring by affecting the quality of parenting and attachment and increasing the risk for the parent of a wide range of negative psychiatric, interpersonal, and functional outcomes
(2,
3), which in turn may lead to a higher-risk child-rearing environment.
These findings suggest that clinicians treating adult depressed suicide attempters should assess for a history of abuse and review the home environment to ensure that risk of exposure to domestic violence and abuse is minimized for the patient and the patient’s children. Similarly, clinicians who treat adolescent suicide attempters should inquire about family history of depression, since maternal depression has been linked in several studies to an adverse response to treatment
(33) . Moreover, recent evidence shows that treatment of maternal depression results in improved psychiatric and functional outcomes for children
(39) . This study suggests that other adverse sequelae of early childhood abuse may also be appropriate treatment foci.
Because suicidal behavior is the single most important risk factor for completed suicide in adolescents, the identification of precursors of adolescent suicidal behavior is of great public health importance
(40) . This first report of precursors of suicidal behavior in a sample at familial risk helps to identify families at very high risk of having a child with suicidal behavior and frames targets for prevention and treatment.