Studies have suggested that childhood- and adolescent-onset major depressive disorder may be distinct subtypes of depression relative to adult-onset major depressive disorder. Jaffee et al. (1) found associations between pre-adult-onset major depressive disorder and unique genetic and early childhood risk factors, such as increased criminality and psychopathology in families of origin, more perinatal insults, more motor skills deficits at birth, more caretaker instability, and more behavioral and sociobehavioral problems. Other studies suggest that pre-adult-onset major depressive disorder may be a more severe variant with increased chronicity and disability, increased levels of anxiety or rates of anxiety disorders, increased rates of alcohol and other drug dependence, and behavioral and personality difficulties
(2 –
6) .
For the initial 1,500 participants who entered the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, we found that pre-adult-onset major depressive disorder was a particularly severe and chronic condition associated with a distinct set of demographic (female gender) and clinical features (longer duration of illness, longer current episodes, more episodes, more suicidality, greater symptom severity, more psychiatric symptoms associated with axis I comorbidity, and more sadness, irritability, agitation, and atypical symptom features) and more psychosocial consequences (lower educational attainment and marriage rates) than adult-onset major depressive disorder
(7) . The next 2,500 STAR*D participants partially replicated the first group’s results, emphasizing that pre-adult-onset major depressive disorder is associated with having more lifetime suicide attempts than adult-onset major depressive disorder and is a more familial subtype of depression
(8) . However, the second report did not replicate other key findings, such as the pre-adult-onset group showing longer current episodes and more total episodes of major depression, greater symptom severity, more psychiatric comorbidity, poorer psychosocial functioning, and more sadness, irritability, agitation, and atypical symptoms of major depressive disorder. This article presents the final analysis of the combined sample. Despite the symptom differences, age of onset before or after age 18 was not associated with a different rate of remission or response in the initial study of citalopram
(9) .
Method
The rationale and design of STAR*D have been described in detail elsewhere
(7,
10,
11) . Briefly, STAR*D aimed to define prospectively which of several treatments were effective for participants with nonpsychotic major depressive disorder who had an unsatisfactory clinical outcome to an initial and, if necessary, subsequent treatment. The participants were recruited from 18 primary care and 23 psychiatric care clinical settings across the United States. To enhance generalizability, only self-declared outpatients seeking medical care were eligible; recruitment through advertisement was prohibited. All risks, benefits, and adverse events were explained to the participants, who provided written informed consent before study participation.
Defining Age of Onset
The age of onset of each participant’s first major depressive episode was recorded at study intake by the clinical research coordinators, who provided the participants with a description of major depression and asked them to estimate the age at which they first experienced persistent dysphoria coupled with other signs and symptoms of a major depressive episode as defined by DSM-IV. This symptom cluster had to have lasted at least 2 weeks, had to be associated with clinically significant distress or impairment in functioning, and was considered to be the first full major depressive episode whether or not treatment was sought. If superimposed on preexisting dysthymic disorder, the age of onset of major depressive disorder was measured by the participant’s best estimate of when the first major depressive episode began.
We divided the sample into distinct age-of-onset categories because previous studies
(1), including our own (7, 8), have suggested there might be distinct subgroups of patients with major depressive disorder based on age of onset of first major depressive episode and because the current diagnostic convention is to use categories rather than dimensions for diagnostic and subtyping purposes. To maximize the probability of identifying clinically meaningful age-of-onset groups throughout the life cycle, while simultaneously enabling comparisons with published works on age of onset, we divided our sample into five groups: childhood onset (ages <12), adolescent onset (ages 12–17), early-adult onset (ages 18–44), middle-adult onset (ages 45–59), and late-adult onset (ages ≥60).
Statistical Analyses
To examine the association of age of onset with participant clinical characteristics, we used regression models with age of onset as an independent variable. For discrete data, logistic regression models were fitted for binary data, and cumulative logistic regression models were fitted for nonbinary data. For continuous data, linear regression models were fitted. Analyses were also conducted to assess the impact of age of onset with adjustment for the effects of current age and gender. Adjusted odds ratios were calculated by exponentiating the parameter estimates for the age-of-onset design variables estimated from the adjusted logistic regression models. Because of the large number of statistical tests, a more stringent significance criterion of 0.005 was employed. Pairwise post hoc comparisons with a Bonferroni correction were conducted for adjusted results with a statistical significance for a pairwise comparison set at p<0.005.
Results
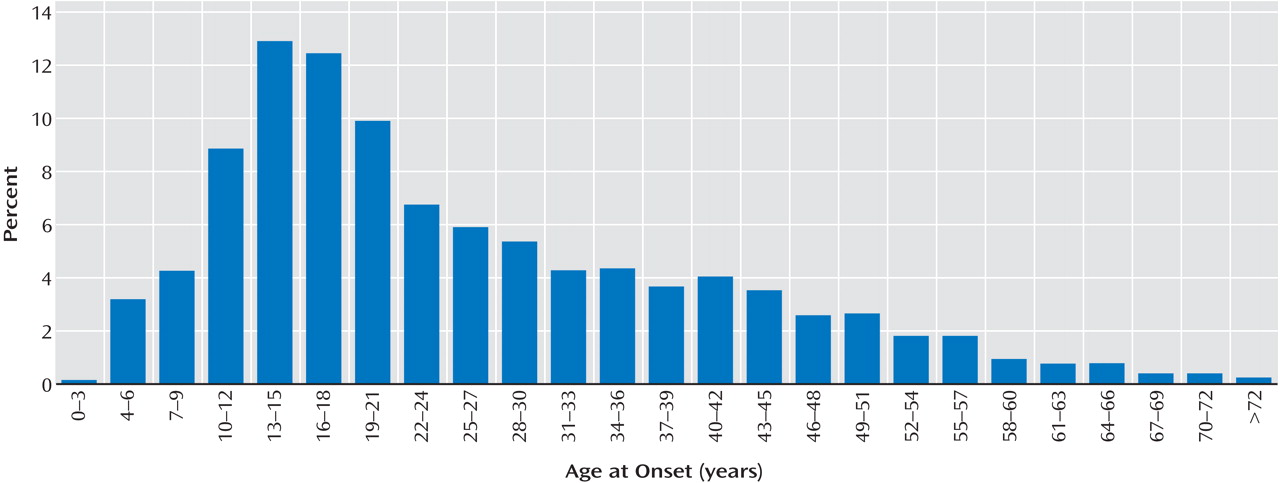
Of the 4,041 participants enrolled in STAR*D, 3,896 had available age-of-onset data. Their mean age of major depressive disorder onset was 26 years (
Figure 1 ).
Participants in the pre-adult-onset groups (childhood and adolescent onset) were younger at entry into the study than those in the adult-onset groups (early, middle, and late onset) (35.2 years, SD=12, versus 43.6 years, SD=13; t=20.3, df=3992, p<0.0001). The pre-adult-onset participants had a greater proportion of women than the adult-onset participants (67.5% versus 59.6%; χ 2 =24.6, df=1, p<0.0001). Because of these results, comparisons between groups were adjusted for the potential confounding variables of gender and current age.
Data supplement
Table 1 (available at http://ajp.psychiatryonline.org) summarizes sociodemographic and family history variables associated with age at onset. Younger age of onset was associated with a larger proportion of participants employed; seeking care in a psychiatric care setting; having a family history of depression, alcohol abuse, or drug abuse; and a smaller proportion of participants married.
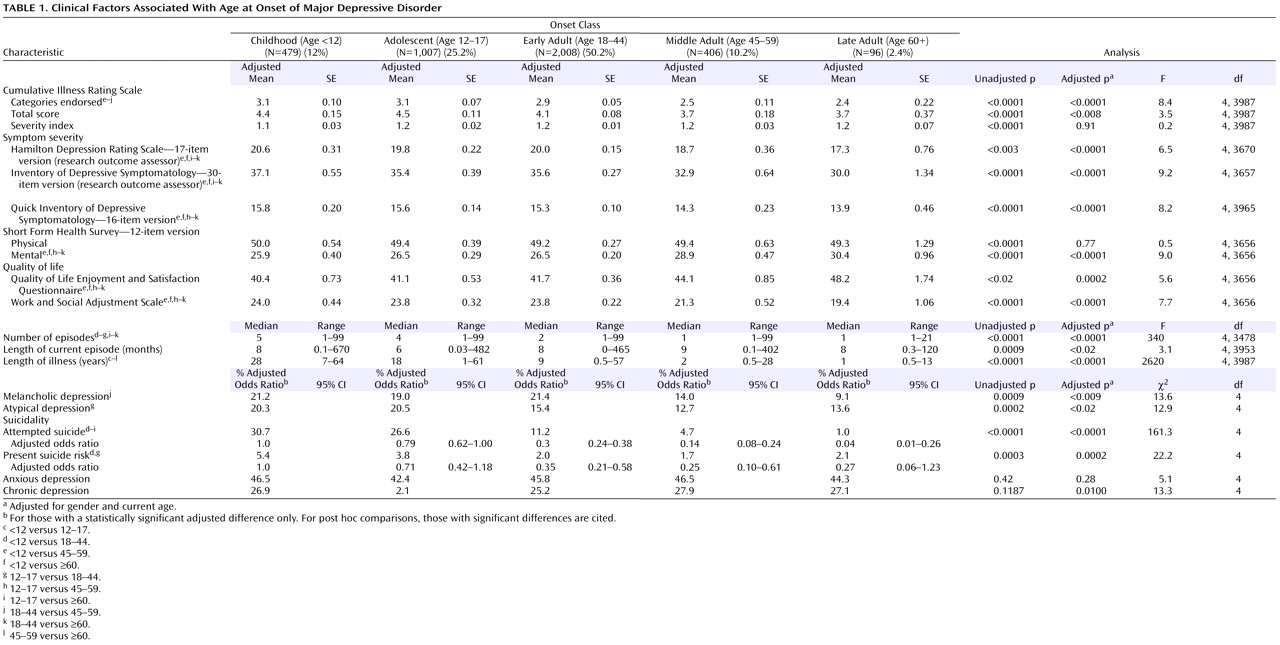
Longer duration of illness and a greater number of lifetime episodes of major depressive disorder were significantly associated with younger age at onset, both before and after adjustment for current age and gender (
Table 1 ). After adjustment for gender and current age, younger age of onset generally indicated higher levels of general medical comorbidity (Cumulative Illness Rating Scale
[12] categories endorsed), greater depressive symptom severity (Hamilton Depression Rating Scale—17-item version, Inventory of Depressive Symptomatology—30-item version
[13], Quick Inventory of Depressive Symptomatology—16-item version
[14] ), worse mental functioning (Short Form Health Survey—12-item version
[15] ), quality of life (Quality of Life Enjoyment and Satisfaction Questionnaire
[16] ), and work function and social adjustment (Work and Social Adjustment Scale
[17] ), increased likelihood of past suicide attempt(s), and greater present suicide risk. There were few significant differences between the middle-adult-onset and late-adult-onset groups except that the former had a longer duration of illness.
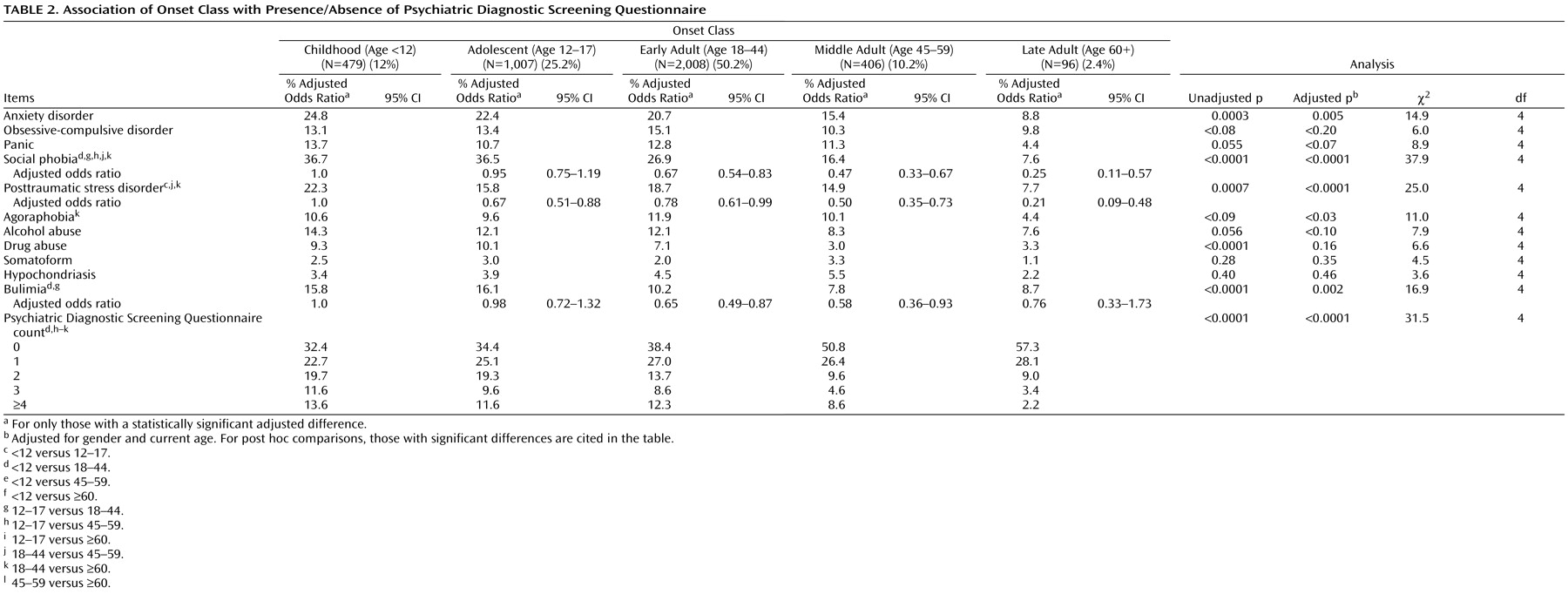
After adjustment for gender and current age, younger age of onset indicated a greater probability of anxiety disorder and social phobia and a greater number of concurrent anxiety disorders (
Table 2 ). Posttraumatic stress disorder (PTSD) was more frequent in the childhood-onset group than in the adolescent-onset group and more frequent in the early-adult-onset group than in either the middle-adult- or late-adult-onset groups. Bulimia was statistically more frequent in the childhood-onset and adolescent-onset group than in the early adult-onset group.
Data supplement
Table 2 shows the prevalence at study entry of specific depressive symptoms in relation to age of major depressive disorder onset. After adjustment for gender, current age, and baseline severity, four symptoms (negative view of self, negative view of future, suicidal ideation, and interpersonal rejection sensitivity) were significantly more prevalent in the youngest age-of-onset groups.
Discussion
Although no single age-at-onset group stood out as distinct, participants who reported younger ages of onset had more severe and recurrent forms of major depressive disorder, whereas the older age-at-onset groups, especially the late-adult-onset group, had the mildest, least pervasive, least dysfunctional, and less recurrent forms. Earlier ages of onset were associated with substantial functional impairment (e.g., poor social and occupational function, poor quality of life) and greater illness burden (more current general medical and psychiatric comorbidity, a more negative view of life and the self, more lifetime episodes of depression, more severe depressive episodes, more lifetime suicide attempts, and greater suicidal ideation). They also were less likely to be “never married,” but the oldest age-of-onset participants were more likely to be “widowed.”
This study does not support the contention that childhood-onset depression is markedly different from adolescent-onset depression in terms of clinical features or treatment outcomes. After adjustment for gender and current age, the only differences between these groups were more family history of alcohol use disorders, longer duration of illness, and greater likelihood of comorbid PTSD in the childhood-onset group. Similarly, few variables distinguished the late-adult-onset group from the other adult-onset groups, and those that were observed (i.e., the oldest participants were more likely to be widowed, completed fewer years of education, were less likely to be employed, and suffered fewer years of illness) appear to be simple epiphenomena of the group classification method. Our findings that pre-adult age of onset is associated with female gender, family histories of depression and substance abuse, medical and psychiatric comorbidity, highly recurrent course and severe index episodes, both atypical and possibly melancholic features, impaired social and occupational functioning, and lower quality of life are consistent with our own preliminary findings with the first 1,500 participants to enter STAR*D
(7) and the work of others
(2 –
6) . Our finding that younger age-of-onset groups were more likely to be seen in specialty psychiatric clinics than older age-of-onset groups may be a function of their increased severity and duration of illness; it is not simply a function of more difficult access to specialty care in the elderly because the results were adjusted for current age.
The methodology of this study does not allow causal explanations for findings. For example, we are unable to say whether all of the negative outcomes described above are due to having an early-onset major depressive disorder or whether pre-adult-onset major depressive disorder may be more likely to occur in individuals already experiencing some of these negative life experiences. On one hand, one of the most pernicious aspects of early age of onset of major depressive disorder is that the depression occurs at or before key developmental milestones, which may have prolonged, rippling effects on the way one feels about oneself; masters key educational, social, or occupational challenges; or learns to compete for success
(18 –
21) . It is certainly possible that interpersonal sensitivity, worse self-esteem, and poorer social adjustment early in life could all contribute to fewer and poorer interpersonal relationships later in life and, theoretically, lower rates of marriage in individuals with early-onset major depressive disorder. On the other hand, one could also make a strong argument that early-onset major depressive disorder is the outcome of a general vulnerability factor, such as neuroticism, that predisposes an individual to an early onset of major depressive disorder. Thus, early onset might identify people who have a different, more pernicious illness than later-onset major depressive disorder.
This study has a number of limitations. The major limitation relates to the uncertainty that results from using self-reports to estimate age of onset of major depressive disorder. This may particularly affect the validity of comparisons between “adjacent” age-of-onset groups, in which a recall inaccuracy of only 1 year would result in misclassification. It is also possible that younger participants may recall age of onset more reliably than older ones because milder episodes experienced early may be forgotten in later years. In addition, ascertaining age of onset during a depressive episode adds another source of bias because depression affects cognition and may color one’s view of their past as well as their present and future. The finding of an association between earlier onset and more severe depression may be due to a misperception by depressed individuals that their depression extends further into the past than is actually so. A second limitation is that age of initial dysphoria may have been a more useful marker of age of onset than the age of the first major depressive episode. At least one investigation found clinically meaningful dysphoria, but not major depressive disorder, important in dissecting out depressive subtypes among patients with major depressive disorder and atypical features
(22) . In either case, however, accuracy of recall would remain a problem. Third, the age-of-onset groupings may not have been ideal to identify specific age-of-onset subtypes. Owing to the increasingly early occurrence of puberty in females, many of the female participants classified as having childhood-onset major depressive disorder (years 0–11) may actually have been in puberty, whereas that was far less likely for the male participants. Fourth, the relative scarcity of participants over age 65 and lack of those over age 75 limited our data on the late-adult-onset group. Fifth, the absence of inpatients, bipolar depressed patients, and treatment-resistant patients may limit the generalizability of the findings, although the paucity of other exclusions allowed for a highly representative group of care-seeking “real patients” with nonpsychotic, non-treatment-refractory major depressive disorder. Sixth, the lack of information on additional factors that might be associated with early age of onset (e.g., personality factors
[3], abuse, or trauma
[23] ) or with late-life age of onset (e.g., cognitive decline
[24] ) prevents a more comprehensive exploration of risks for, and consequences of, age of onset of first major depressive episode. Finally, the use of multiple comparisons could result in finding something statistically significant by chance or with little clinical meaning, although this was at least partially addressed by using a stricter threshold for significance (p<0.005) and conducting Bonferroni corrections for pairwise post hoc comparisons of adjusted results.