Despite advances in treating HIV infection, there remains great variability in the course of this disease, including the length of time before an AIDS diagnosis and mortality. Some of this variability has been explained by psychosocial variables
(1) . Studies have shown that stressful and traumatic life events and chronically elevated depressive symptoms are associated with more rapid progression to AIDS, mortality, and other indicators of immune compromise
(2 –
12) . These studies have been largely conducted before the advent of highly active antiretroviral therapy. Since the era of highly active antiretroviral therapy, there have been limited studies showing the association of depressive symptoms with faster decline in antigenic marker on helper/inducer T cells (CD4)
(13), an increase in HIV viral load
(13,
14), progression to AIDS
(14 –
16), and mortality
(14,
17) . To our knowledge, there are no studies during this recent era, however, examining the effects of trauma and recent stress on HIV morbidity and mortality.
One could argue that more convincing evidence of an underlying relationship between psychosocial factors and HIV disease course may come from studying trauma because the timing of these stressors relative to HIV disease change (e.g., childhood abuse and neglect) may be less ambiguous than the timing of depression. The goal of the current study was to examine the effects of lifetime trauma, recent stressful events, and depressive symptoms on all-cause and AIDS-related mortality among HIV-infected men and women during the era of highly active antiretroviral therapy. We hypothesized that these psychosocial variables would significantly predict faster HIV-specific and all-cause mortality.
Method
Sample and Procedure
As part of the Coping with HIV/AIDS in the Southeast (CHASE) study, we consecutively sampled HIV-infected men and women who received care at one of eight infectious diseases clinics in five Southeastern states: North Carolina, South Carolina, Alabama, Georgia, and Louisiana. We chose clinics outside major metropolitan areas that had at least two infectious diseases specialists. Details regarding sampling and the study population have previously been described
(18) . The institutional review boards at the University of North Carolina, Duke University, and all study sites approved the study. Written informed consent was obtained after we described the study to the subjects.
The consecutive sampling of patients was strictly enforced. HIV-infected English-speaking patients at the eight clinics were eligible to participate if they passed the Short-Portable Mental Status Questionnaire
(19) . From December 2001 through April 2002, 611 patients enrolled in the CHASE study and were followed longitudinally by interview every 9 months for 27 months. Sociodemographic and psychosocial information was obtained through structured interviews in the clinics, nearby locations, or patients’ homes and lasted, on average, 2 hours. The interviewers engaged in a week-long training on instrument administration followed by certification in the field.
Medical information (e.g., CD4, viral load, HIV medications, and mortality) was obtained by trained health care providers from the patients’ medical records and recorded on standardized abstraction forms. Chart abstraction was done for all 527 CHASE participants (86.2% of 611) who provided consent. The current analysis includes 490 (80.2% of 611) who had chart abstraction data available starting from the date of the baseline interview. The participants included in the analysis were more likely to be white than those not included (34% versus 23%, p=0.02); otherwise, the two groups were similar on baseline sociodemographic, clinical, and psychosocial characteristics. Chart data on mortality were available for up to 41 months, with a median of 31 months.
Measures
Mortality
Cause of death was recorded on the chart abstraction form as indicated in the chart by the infectious diseases physician. The participants were coded as dying from an AIDS-related condition if the cause of death was recorded as an opportunistic infection (N=12) or if the cause of death was unknown but either the most recent CD4 count before death was <200 cells/mm 3 (N=3) or an opportunistic infection (AIDS category C) was noted in the 12 months before death (N=1). All 12 individuals recorded on the chart as having died of AIDS had either a CD4 <200 or an opportunistic infection immediately before death, and all 11 individuals recorded as having died of non-AIDS-related causes had both CD4 >200 and no recent opportunistic infection immediately before death.
CD4 lymphocyte count and HIV RNA viral load
Each participant’s baseline CD4 count and viral load were determined from the medical record abstraction forms and were defined as the most recent measure within 6 months of study enrollment.
Antiretroviral therapy
Detailed information on past and current antiretroviral therapy was recorded on the chart abstraction forms. Antiretroviral therapy exposure status was modeled, as previously recommended
(20), using a time-varying covariate over the follow-up period with a dichotomous variable indicating whether, for each given month, the participant had been receiving antiretroviral therapy at least 80% of the time during the preceding 6 months. The large majority of patients receiving antiretroviral therapy (∼90%) were receiving highly active antiretroviral therapy concordant with clinical recommendations in effect at the time (e.g., at least three antiretroviral agents including at least one protease inhibitor, nonnucleoside reverse transcriptase inhibitor, or abacavir).
Number of categories of lifetime traumatic events was constructed by assigning one point for each of 15 traumas (e.g., sexual abuse, physical abuse, childhood physical neglect, childhood emotional neglect, presence of seven other types of trauma before the age of 18, and presence of four lifetime traumas). Each trauma component has been detailed previously
(18), with a more concise description below. The number of categories or types of traumatic events has been widely used; patients experiencing more such categories have been shown to have higher rates of life-threatening medical conditions
(21) .
The measure of lifetime
sexual and physical abuse history was based on our previous studies and has been shown to correlate with many indicators of poor health
(22 –
24) . We defined sexual abuse to include sexual experiences (e.g., touching, intercourse) where force or threat of force was used; however, in children (<13 years) the threat of force or harm was implied by a 5-year age differential between the victim and perpetrator. We defined physical abuse as incidents separate from sexual abuse that included life threat (being physically attacked with the intent to kill or seriously injure) and other physical abuse (being beaten, hit, kicked, bitten, or burned).
The Childhood Trauma Questionnaire
(25) was used to assess
physical and emotional neglect during childhood. Cronbach’s alpha reliability has been reported at 0.89 for emotional neglect and 0.66 for physical neglect, and both have substantial test-retest reliability (0.81 and 0.79, respectively). We used the cutoff suggested by Bernstein and Fink
(25) for moderate physical neglect (9 or higher) and moderate emotional neglect (12 or higher) for adding one point each to the total number of lifetime traumas.
The interview also included questions adapted from previous research
(21,
26) concerning a variety of
other traumas occurring before the age of 18 and at any time. Presence of
other trauma before the age of 18 included 1) parental alcohol/drug abuse; 2) parental depression or parental suicide or attempted suicide; 3) imprisonment of parent; 4) domestic violence in the home; 5) subject sent to reform school, prison, or foster care or adopted; 6) death of immediate family member (mother, father, or sibling), and 7) subject having a life-threatening illness or injury not HIV-related.
Lifetime trauma included 1) the murder of a close family member, 2) the death of a child, 3) the death of a spouse/partner, and 4) other trauma written in by the subject that was judged by one of the authors (J.L.) to be similar in severity to those listed above.
Recent stressful life events were measured with a modified version of the Life Experiences Survey
(27,
28), including stressors during the 9 months before the baseline and at each 9-month follow-up. The list was modified to include only the events that were considered moderately to severely stressful based on our previous studies with interviewer-based objectively rated stresses
(4,
11,
29) . Stresses included marriage or engagement, divorce, an increase in serious arguments or separation from mate/partner in a committed relationship, estrangement from a family member, the death or serious illness of a family member or a close friend, trouble with employer or work, lost employment, looking for work, working long hours, major financial problems, major illness or injury other than HIV, major motor vehicle accident, physical or sexual assault, feeling unsafe in neighborhood, patient or close relative or mate arrested or convicted of serious crime, subject robbed or home burglarized, the subject or partner was pregnant or had a baby, subject ended formal schooling, the subject or his or her child leaving home for the first time, and moving residence more than once. We counted the number of events and omitted any HIV-related stresses. The number of recent stresses could vary between 0 and 42.
The Brief Symptom Inventory
(30), measuring psychological symptoms, is a shortened version of the well-validated Symptom Checklist—90. We focused on the depression subscale (Cronbach’s alpha=0.85
[30] ), assessed at baseline and at 9-month intervals. Scores on the depression subscale were converted to gender-specific T scores
(30) ranging from 0 to 100, with a higher score indicating more depressive symptoms. A change of 10 units corresponded to a shift of one standard deviation in the normative population.
Psychotropic medication use
The participants reported mental health-related medications at baseline, which we dichotomized for analyses (antidepressant and/or anxiolytic or none).
Statistical Analyses
Univariate analyses were performed for all study variables to ensure that distributional assumptions were met. We modeled time from study baseline to two outcomes with survival analysis techniques: 1) all-cause mortality and 2) AIDS-related mortality. The patients were censored at loss to follow-up or, in the latter case, at non-AIDS-related death. In bivariate analyses, survival probabilities between groups were compared with log-rank tests, with continuous covariates categorized into quartiles. Given a small number of events, multivariable Cox proportional hazard regression models for each outcome were developed in two stages to avoid overfitting. First, two groups of covariates were considered in separate models: sociodemographic (age, gender, race [white/nonwhite], years of education, gay or bisexual) and clinical (baseline CD4, baseline viral load, antiretroviral therapy status). Owing to nonlinearity in the bivariate relationship between baseline CD4 and survival time and for ease of interpretation, CD4 was modeled with a dichotomous term (<200 versus ≥200). Viral load was log (base 10) transformed. Covariates with a p value <0.20 in each model were then combined. Three final models were fitted by using the retained covariates from the first step, each containing one psychosocial variable (lifetime traumatic events, recent stressful life events, and depressive symptoms). Psychosocial variables were considered independently owing to some correlation between predictors (r=0.24–0.32). Covariates excluded at the first stage were reintroduced into the final model one at a time to confirm that their addition would not substantively affect coefficients or statistical significance. The results were compared for models that did and did not control for the use of antidepressants and/or anxiolytics at baseline, a potential mediator. In addition, we ran the all-cause mortality equations with control for recruitment site by using seven dummy variables. Because two recruitment sites had no AIDS-related deaths, we could not control for site in analyses predicting AIDS mortality.
Depressive symptoms, stressful life events, and previous 6 months antiretroviral therapy status were modeled as time-varying covariates. Values for depressive symptoms and stressful life events were updated with the value from the most recent survey (every 9 months). Thus, this analysis strategy accounted for change in these predictors over time. Antiretroviral therapy status was updated on a monthly basis, reflecting antiretroviral therapy exposure in the 6 months immediately preceding that month. For ease of interpretation, the depressive symptoms score was divided by 10 so that the relevant exponentiated coefficient corresponded to the predicted relative change in the hazard of a 10-unit change in depressive symptoms.
In modeling continuous variables (age, years of education, log-transformed viral load, number of lifetime traumatic events, depressive symptoms, and stressful life events), we confirmed the appropriateness of a linear specification by comparing it to a restricted quadratic spline specification with three knots
(31) . We verified the assumption of proportionality in the log hazard by examining plots of Schoenfeld residuals for each covariate in the final model and evaluated interaction terms with the natural logarithm of analysis time for covariates that appeared to violate the proportional hazard assumption
(32) . We also performed a logistic regression with control for age, education, and race, comparing men and women on types of traumatic events reported.
Results
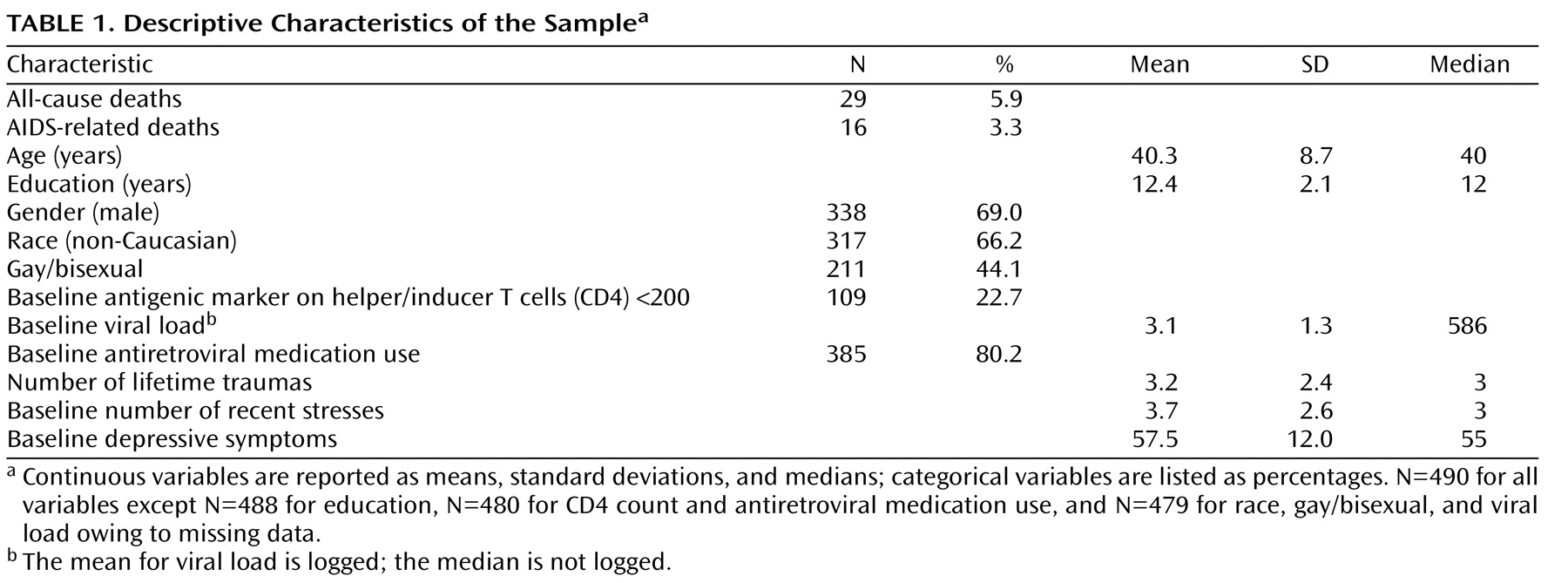
Table 1 provides descriptive information about all variables used in these analyses. The mean age of the participants was 40.3 years, with a range from 20 to 70. Most were men (69.0%), nonwhite (66.2%), and had a high school education or less (53.9%). Gay or bisexual persons made up 44.1% of the sample.
During the 1,070 person-years of follow-up contributed by the 490 participants (mean=2.22 years, SD=0.86), there were 16 AIDS-related deaths and 29 total deaths, corresponding to an AIDS-related mortality rate of 1.5 per 100 person-years and an all-cause mortality rate of 2.7 per 100 person-years. The median baseline CD4 count was 365, with 22.7% of the participants having a CD4 count <200. The median baseline viral load was 586, with 47.0% having undetectable levels (<400 copies). The majority (80.2%) were receiving antiretroviral therapy at baseline.
Both the median number of categories of lifetime trauma and the median number of recent stressful events during the 9 months before study entry were three. Few subjects (<10%) reported having any trauma within the 2 years before study entry. As part of the trauma measure, 33.1% had been sexually abused, 38.4% had been physically abused, and 53.1% had either or both types of abuse. Compared to men, women were more likely to report sexual abuse (odds ratio=1.82, p=0.002) or having a child (odds ratio=7.04, p<0.001) or a partner die (odds ratio=1.72, p=0.02). At baseline, our participants scored above average on depressive symptoms, with slightly over one-third (34.3%) above the 90th percentile
(30) . Approximately 75% of the participants remained either above or below the 90th percentile between consecutive time points.
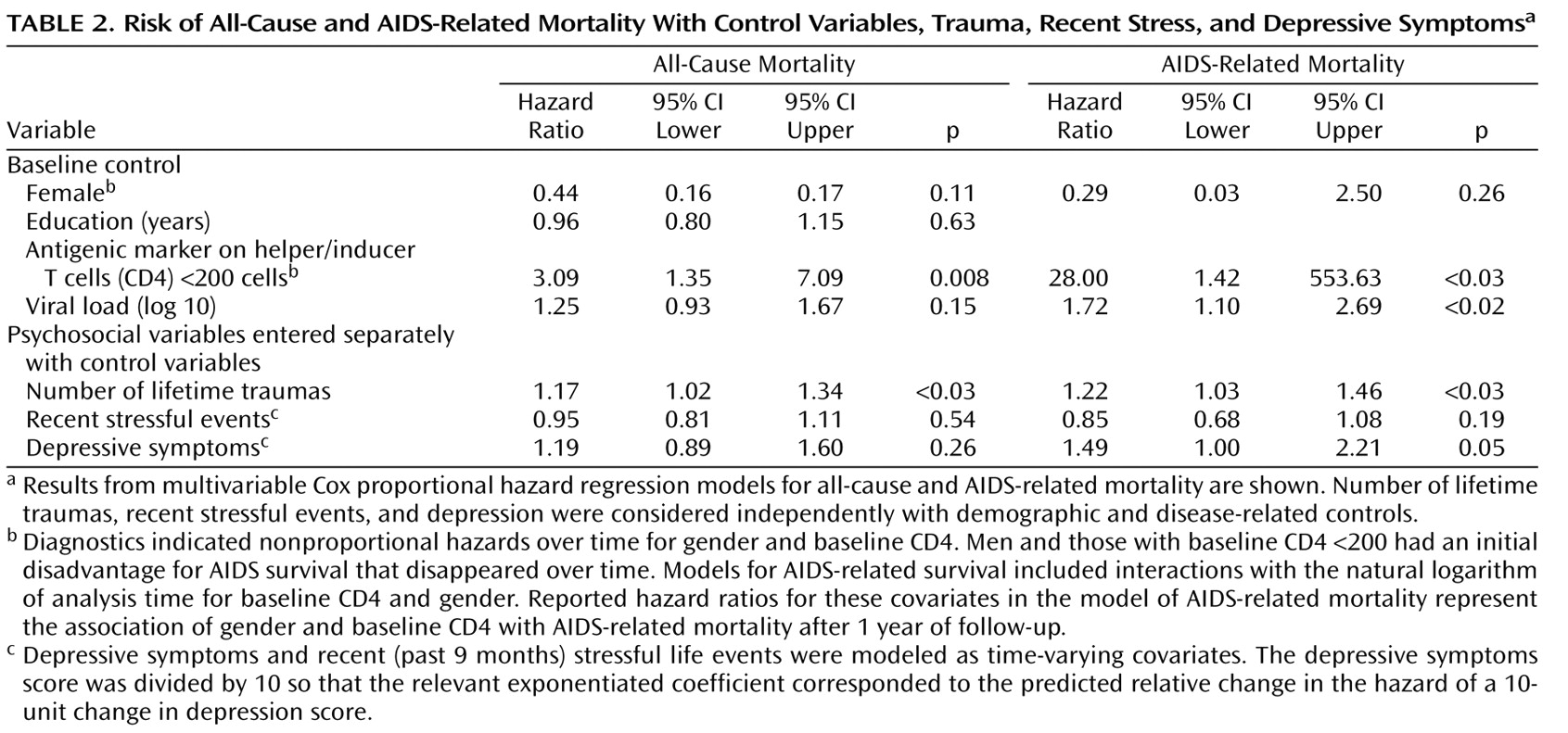
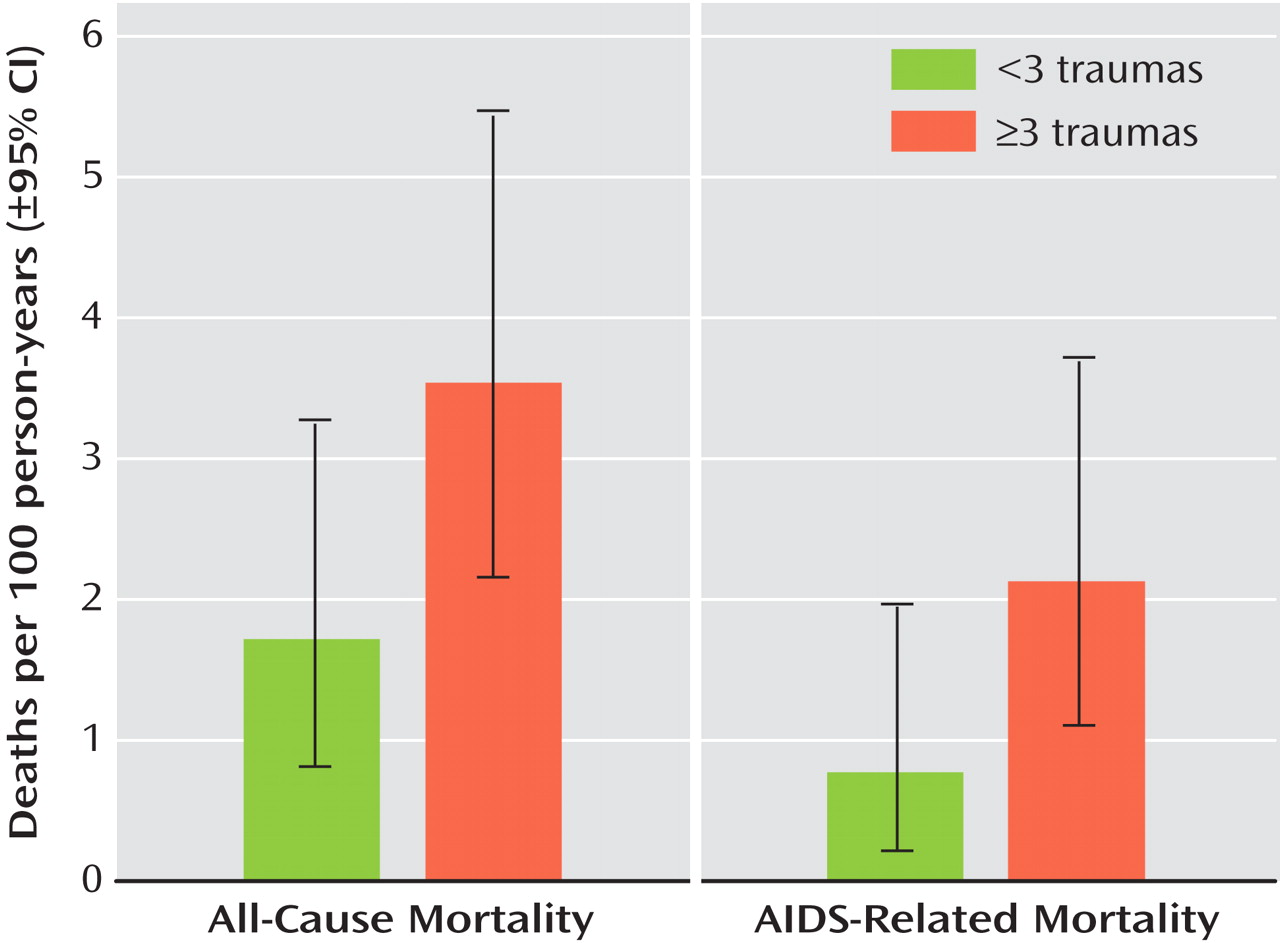
Table 2 shows the Cox regression results for all-cause deaths and AIDS-related deaths. Note that for all-cause deaths the only significant predictors were baseline CD4 <200 and number of categories of lifetime trauma. Those with CD4 <200 at baseline had about triple the risk of all-cause death compared to those with higher CD4 counts. For every one unit of trauma, patients had a 17% increased risk of death; for every three-point (median) increase in trauma, the risk of death increased by 60%. For those at or above the median in trauma, 7.8% (N=20) died, corresponding to a death rate of 3.54 per 100 person-years, compared to 3.8% (N=9) and a death rate of 1.72 for those below the median (adjusted rate ratio=3.42, 95% CI [confidence interval]=1.08–10.77, p=0.04) (
Figure 1 ).
Baseline CD4 <200, higher baseline viral load (log transformed), lifetime trauma, and depressive symptoms were significantly related to greater risk of AIDS-related mortality. In this model, diagnostics indicated nonproportional hazards over time for gender and baseline CD4 such that men and those with baseline CD4 <200 had an initial disadvantage for AIDS survival that disappeared over time. For every one unit of trauma, the patients had a 22% increased risk of dying from AIDS; for every three-point (median) increase in trauma, the risk of AIDS death increased by 83%, almost doubling. For those at or above the median in trauma, 4.7% (N=12) died from AIDS, corresponding to a death rate of 2.13 per 100 person-years, compared to 1.7% (N=4) and a death rate of 0.77 for those below the median (adjusted rate ratio=3.27, 95% CI=1.05–10.21, p=0.04) (
Figure 1 ). Finally, for every 10-unit (1 standard deviation) increase in depressive symptoms, the risk of an AIDS death increased by 49%.
Adjustment for use of antidepressants and/or anxiolytics at baseline did not change any results in
Table 2 . In addition, there were no significant differences between clinic sites on all-cause (p=0.36) or AIDS-related mortality (p=0.75). Controlling for site did not appreciably change the hazard ratios in all-cause mortality models. No interaction terms of trauma and depression with CD4 and viral load were significant in either the all-cause or AIDS-related models.
Discussion
In studying HIV-positive men and women for up to 41 months, we found that patients with more categories of traumatic events had an increased risk for all-cause and HIV-specific mortality. Although few patients died during the follow-up study (5.9%), previous trauma (most events occurring during childhood or years before the study) predicted mortality. The rate of all-cause and HIV-related death for those at or above the median in trauma was about three times the rate for those below the median. These effect sizes for trauma are similar to those shown for depression and the risk of other diseases (e.g., heart disease, stroke, or cancer)
(33) . It is notable that over one-half of our participants experienced three or more lifetime traumas, and over one-half had a history of sexual and/or physical abuse. Previously in this cohort, we showed that trauma was associated with more bodily pain, disability, and use of health services
(18), as well as developing an AIDS clinical condition
(34) . Our study advances previous work by being the first to our knowledge in the era of highly active antiretroviral therapy to show that traumatic life events are associated with faster all-cause and AIDS-related mortality.
Depressive symptoms were also associated with faster HIV-related mortality, although not all-cause death. These findings are consistent with previous HIV literature
(4,
10,
12,
17,
35) and studies on other medical conditions
(33) . With relatively few deaths during follow-up, we may not have had ample power to test this hypothesis relative to all-cause death in which the effects of depressive symptoms may be less pronounced.
Although previous studies have shown that stressful events are associated with faster HIV disease progression
(4,
6), no studies, to our knowledge, including the current one, have reported that recent stressful events predict faster mortality. In addition, reliance on questionnaire approaches for measuring recent stress has been shown to be less reliable than interview-based ratings or studying persons experiencing a particular stressor (e.g., bereavement)
(1) .
Several caveats should be acknowledged when interpreting the data from our study. Our participants were chosen from HIV clinics in the rural southeast and may not be representative of other areas of the country. The HIV epidemic, however, is growing disproportionately faster in this region. We could not control for length of time with HIV infection because the date of infection was unknown, although we did control for baseline CD4 count and viral load (two approximations of disease stage). We found that baseline CD4 count below 200 was associated with all-cause mortality and with an initial disadvantage for AIDS survival, although the latter association disappeared over time. In addition, higher baseline viral load was related to increased risk of AIDS mortality.
Another potential study limitation is that some uncontrolled variables, such as risky behavior or medication nonadherence, may mediate or account for our findings. We could not accurately control for adherence to medications because we had only baseline data on adherence and about 20% of our patients were not receiving antiretroviral therapy at entry. Demographic variables and use of antiretroviral therapy, however, did not explain the relationships shown in this study. Finally, although we could not control for possible site effects in analyses of AIDS-related mortality, site was not significantly associated with mortality owing to AIDS, and site did not affect the relationship of trauma with all-cause mortality.
We also need to be cautious in interpreting the causal direction of the psychosocial/mortality relationships. To address causal direction, the depressive symptoms score was modeled as a time-varying covariate. The measure of trauma was less likely to be confounded with HIV disease progression because most of the traumatic events reported happened many years before the study and before HIV infection. In addition, using number of events rather than the patients’ ratings of their traumatic experiences reduced the possibility that poor health preceding death might lead to higher trauma scores. Trauma may provide the best evidence for the impact of psychosocial factors on mortality in HIV. Although the measure of trauma may involve some recall bias, this is unlikely to explain our findings.
Our findings should be viewed with caution because we had relatively few instances of mortality, especially AIDS-related death. Furthermore, the measure of AIDS-related mortality may be subject to some misclassification error because we classified four individuals with unknown cause of death but last CD4 <200 or recent opportunistic infection as dying from AIDS. Our findings, however, did not change appreciably when those with unknown cause of death were reclassified as not dying from AIDS. Our mortality rates were somewhat higher than that reported in a recent study during comparable years
(36), perhaps owing to sampling rural clinics in the southeast.
Although we do not know the biological mechanisms accounting for the relationship of trauma and depression with HIV mortality, previous studies have linked increases in cortisol and norepinephrine to both psychological variables
(5,
37) and HIV disease progression
(4,
38,
39) . These biological mechanisms may mediate the detrimental effects of trauma and depressive symptoms.
In conclusion, to our knowledge, these data provide the first prospective evidence in this era of medication advances that trauma may contribute to mortality in HIV-infected persons. Further research is needed to determine if psychological and psychiatric interventions can modify the detrimental effects of trauma and depression, thereby altering the course of HIV disease progression.