General hospitals are the largest providers of inpatient psychiatric services in the United States on the basis of admissions and the number of psychiatrists employed
(1) . According to data from the Center for Mental Health Services, general hospitals accounted for 49.9% of admissions to 24-hour hospital and residential treatment centers in 2002 and employed 4,348 psychiatrists in 2000. Many general hospitals also provide ambulatory and emergency psychiatric care. Medical and surgical inpatients often have psychiatric conditions that require psychiatric consultation. Most leading academic departments of psychiatry are based in general hospitals and perform the bulk of federally funded psychiatric research, the training of psychiatric residents, and the education of medical students. The top 10 medical school departments of psychiatry by National Institutes of Health funding are all based in general hospital-linked academic medical centers. Despite these critical functions, psychiatric services in general hospitals are vulnerable. Reimbursement and operating margins for hospital and physician psychiatric services lag behind those of other medical services. This article will review the current state of psychiatric services in general hospitals, outline current challenges, and make recommendations for their future.
Before the 1940s, 96% of all inpatient psychiatric services were provided in publicly funded state mental hospitals and veterans’ hospitals, with nearly all of the remainder provided in private psychiatric hospitals. Beginning in the 1930s, a few academic medical centers developed inpatient psychiatric services funded in part by grants from the Rockefeller Foundation
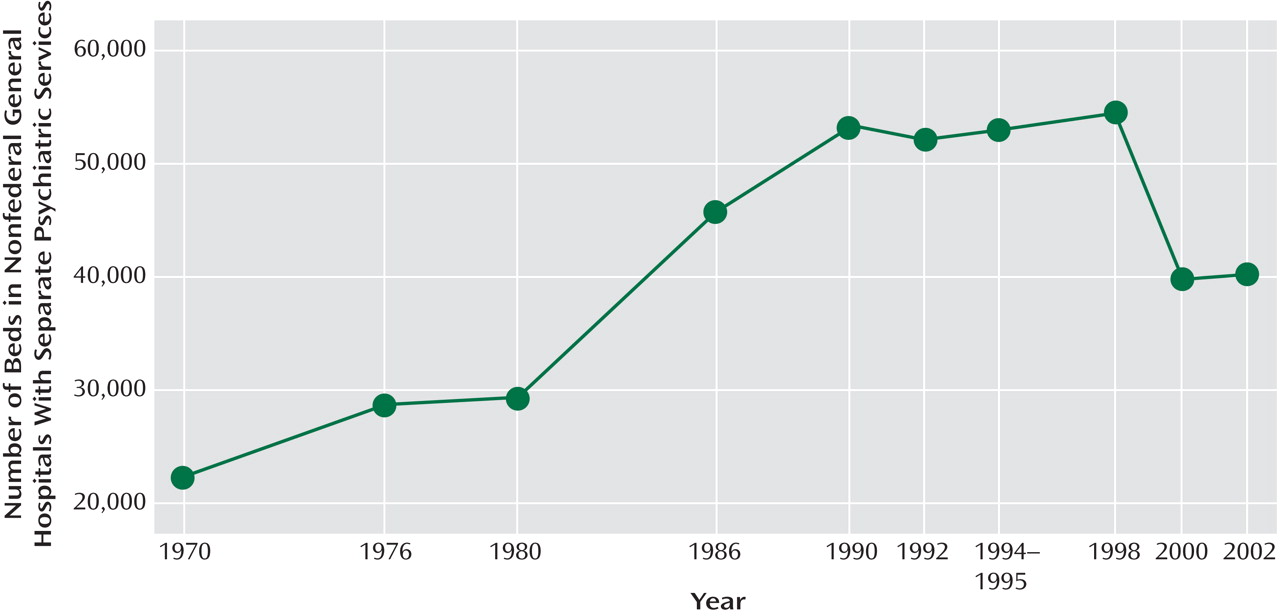
(2) . From these limited services, the number of psychiatric beds in general hospitals expanded rapidly during the next 60 years, peaking at 54,434 in 1998
(1) . In the 1980s, several factors led to the growth of psychiatric capacity in the private sector. The implementation of prospective payment under Medicare in 1982 with a diagnosis-related group methodology shortened lengths of stay and created capacity in the medical/surgical units of general hospitals and an incentive to develop inpatient psychiatric services that continued to receive retroactive cost-based reimbursement because there was insufficient information to predict resource use under diagnosis-related groups
(3) . The fiscal value of inpatient psychiatric services also led to an expansion of investor-owned psychiatric hospitals, spurring private investment and capitalization. As a result of the increased availability of psychiatric inpatient beds and the private and public insurance to pay for them, expenditures for psychiatric services rose rapidly. In current dollars, expenditures by mental health organizations increased more than 11-fold between 1969 and 1998, from $3.3 billion to $38.5 billion
(1) . Private insurers and employers became concerned that the increasing expenditures reflected provider-induced demand and an insurance “moral hazard.” Insurers looked to specialty mental health management (“carve-out”) companies to help control the growth of these costs. As they consolidated and were managing more covered lives, these organizations developed significant purchasing power, leading to reductions in hospital per diem rates and professional fees, often to a level below the fully allocated cost of these services. At the same time, expenditures for psychopharmacologic agents, often borne by the primary insurer, increased dramatically. Patients with combined medical and psychiatric disorders—an increasing and underrecognized population—were often outside the coverage of carve-out payers. In the 1990s, as the financial performance of inpatient psychiatric services deteriorated, general hospitals began to question whether inpatient psychiatric services were part of their core mission. Hospital turnaround consultants would usually point to the inpatient psychiatric unit as a financial drain and recommend closing it. For example, after eliminating two-thirds of its psychiatric inpatient capacity, only an outcry from the community and the nonpsychiatric medical staff prevented the renowned Beth Israel Deaconess Medical Center in Boston from closing its sole remaining psychiatric unit. A similar effort blocked the planned relocation of psychiatric beds to an off-site location from Fletcher Allen Health care, the main teaching hospital of the University of Vermont School of Medicine.
Figure 1 illustrates the growth in psychiatric beds in general hospitals and then by 2002, a decrease to 40,202
(1) . The number of general hospitals providing psychiatric services declined from 1,707 in 1998 to 1,285 in 2002
(1) . (Inpatient beds in private psychiatric hospitals also increased from 14,295 in 1970 to a high of 44,871 in 1990 before dropping back to 25,095 in 2002.) Despite the recent decrease in beds, the number of psychiatric discharges from general hospitals increased from 1988 through 1994 by approximately 35%, from 1.4 to 1.9 million discharges
(1) . General hospitals increasingly replaced public mental hospitals as the institutions caring for publicly funded patients
(4) . Discharges from general hospital units for patients with serious mental illness increased by 34.7% from 1995 to 2002
(5) . In addition to the difficult circumstances for inpatient care, negative margins associated with ambulatory, emergency, and consultation services make clinical services in general hospitals and in academic departments of psychiatry net losers requiring subsidies from hospital funds and/or faculty practice plans.
Psychiatric services in general hospitals have become vulnerable to downsizing, closure, or movement off campus for several reasons. Inadequate reimbursement has led to poor or negative operating margins. A 2002 study done by the Public Consulting Group for the Massachusetts Medicaid program, a major payer for psychiatric services, found that general hospitals were being reimbursed for their psychiatric services by the mental health carve out at 39% less than their costs (unpublished report by the Public Consulting Group). A similar study of community hospitals in the state of Washington concluded that financial losses from inpatient psychiatric units threatened the viability of the entire hospital
(6) . Inpatient psychiatric services were, until recently, the only inpatient services not included in the Medicare prospective payment system. Moving from a cost to a prospective payment system had been mandated by Congress to reduce costs for inpatient psychiatric care but had been long delayed because of the lack of an appropriate diagnosis-related group-based methodology. Despite Medicare’s data showing higher cost per case because of acuity and medical comorbidity in general hospital patients, the recently introduced Medicare prospective payment system for inpatient psychiatry shifts dollars from general to freestanding hospitals
(7) . The new prospective payment system does not fully account for the costs of the patients who are cared for in general hospitals—particularly for patients with significant medical comorbidities or problems with activities of daily living
(8) .
Tertiary care hospitals have also experienced increasing shortages of medical-surgical beds. This may cause their emergency rooms to become dangerously overcrowded and/or to divert cases to other hospitals. This encourages hospitals to look at converting their inpatient psychiatric beds to needed and higher margin medical-surgical beds. Finally, there is a lack of appreciation that mental illness, which frequently co-occurs with medical illness
(9), is highly prevalent and disabling. This ignorance and accompanying stigma cause behavioral disorders to be mischaracterized as self-inflicted, less real, or less serious for the individual or their family or community. In fact, a World Health Organization analysis showed that mental illness is the leading cause of healthy life lost in disability-adjusted life-years in the world
(10) .
Despite the prevalence of psychiatric illness in general hospital patients, the large psychiatric research portfolios at major academic medical centers, and the increasing understanding of the basic neurobiology underlying major psychiatric syndromes, the payment structure for psychiatric services leaves them commoditized, relatively underpaid, and disconnected from the medical-surgical insurance system.
The Future
If nothing is done to reverse the trends in reimbursement, the future of psychiatric services in general hospitals is worrisome. Even hospitals with healthy operating margins will look at their psychiatric services as a financial drain and consider closing them. So what? Why are psychiatric services needed in general hospitals? First, some psychiatric patients need more care for general medical conditions than can be provided in freestanding psychiatric hospitals, crisis stabilization units, or other less intensive facilities. The new Medicare prospective payment system for psychiatric services partially recognizes that medical comorbidity costs more, and hospitals that care for these patients have modest (though inadequate) enhancements in their per diem rates. Second, patients with psychiatric problems are frequently cared for in the emergency rooms of general hospitals and can tie up staff and beds if they cannot be evaluated appropriately. It generally takes longer to transfer a patient to another facility than to admit to one’s own inpatient unit. The cost of providing these emergency and consultation services has historically been subsidized by the margins from inpatient psychiatric services. As margins erode, hospitals may curtail these essential services, leaving psychiatric patients in medical-surgical beds without appropriate and humane treatment and burdening medical staff inexperienced in caring for psychiatric patients. Third, tertiary care general hospitals are the principal training sites for medical students, residents, and other trainees. Although this may be an unintended consequence of funding graduate medical education through Medicare, training in general hospitals does allow for more interaction between medical and psychiatric trainees. This is particularly important because more patients with psychiatric problems are seen in primary care than by psychiatric specialists. Finally, research in medical school departments of psychiatry is closely linked to the broader research enterprise, particularly in molecular genetics, neuroimaging, and health services research based in academic medical centers.
What can be done to enhance the viability of psychiatric services in general hospitals
(1) ? It is essential to negotiate better reimbursement rates with private payers. There is no a priori reason why psychiatric services should be paid less than their costs while other hospital services are very profitable. Hospitals need to use their leverage as major providers of medical-surgical care to ensure that adequate rates for psychiatric care are paid by any insurer or carve out. Similarly, public mental health carve outs need to be pressured and funded by legislators to pay adequate rates
(2) . Other essential psychiatric services, including emergency, consultation, and ambulatory services, must be reimbursed at an economically self-sustaining level, reducing the overreliance on margins from inpatient services to cross-subsidize this care
(3) . General hospitals should effectively partner with freestanding hospitals or other community-based services to ensure that care is provided in the most efficient environment. General hospitals may need to focus on the care of patients with more substantial medical comorbidity and provide a safety net for persons with severe and persistent mental illness
(4) . General hospitals need to partner with others to reduce stigma. Personal stories of the impact of mental illness on individuals and their families are essential in this effort
(5) . Finally, departments of psychiatry need to develop other revenue streams, including philanthropy, to support their activities.
The recent Institute of Medicine report on quality of care for mental health services
(11) recognized the essential indivisibility of medical and psychiatric care. Several generations have passed since psychiatry moved into general hospitals. Advances in clinical services and increased disease recognition and care by nonpsychiatric physicians have transformed an isolated specialty into one closely linked to all medical services. Discoveries in molecular biology, genetics, and neuroimaging are transforming our understanding of these common and disabling conditions. The general hospital and general medical sector are now major components of our clinical care, research, and training missions. It is important that we preserve these accomplishments with more comprehensive public policy and care strategies. The American Hospital Association recently concluded, “As an important player in the continuum of care, hospitals that positively address behavioral health care needs will contribute to the more effective and efficient use of health care resources, while also helping to produce positive outcomes for patients and their communities”
(12) .