The effects of extreme stress have long been recognized through syndromes such as battle fatigue and shell shock. However, it was not until 1980 that APA first included posttraumatic stress disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), in part because of a social demand to acknowledge and describe the insidious psychological problems experienced by many of the Vietnam veterans returning from an unpopular war. The significance of creating PTSD as a diagnosis was the recognition that responses to traumatic events formed a legitimate psychiatric condition influenced by the meaning of social events and were not merely a matter of individuals’ weakness. This inclusion has allowed the identification of a broad range of psychiatric symptoms and accompanying difficulties associated with extreme stress. It has been a crucial step in providing a framework to investigate scientifically how traumatic experiences occurring at various stages of the lifespan can profoundly, and in some cases permanently, alter individuals’ psychology and biology.
However, there is still no clear consensus concerning the interaction of genetic and environmental factors that predispose individuals to PTSD, mechanisms underlying the development of and recovery from PTSD, or the precise role of social and cultural influences on individuals’ risk or prognosis for the disorder. The variety of articles in this issue concerning PTSD attests to this complexity.
The article by Wessa and Flor approaches the study of PTSD from a fear conditioning perspective. This model is widely accepted in the PTSD literature and has been supported by a considerable number of studies
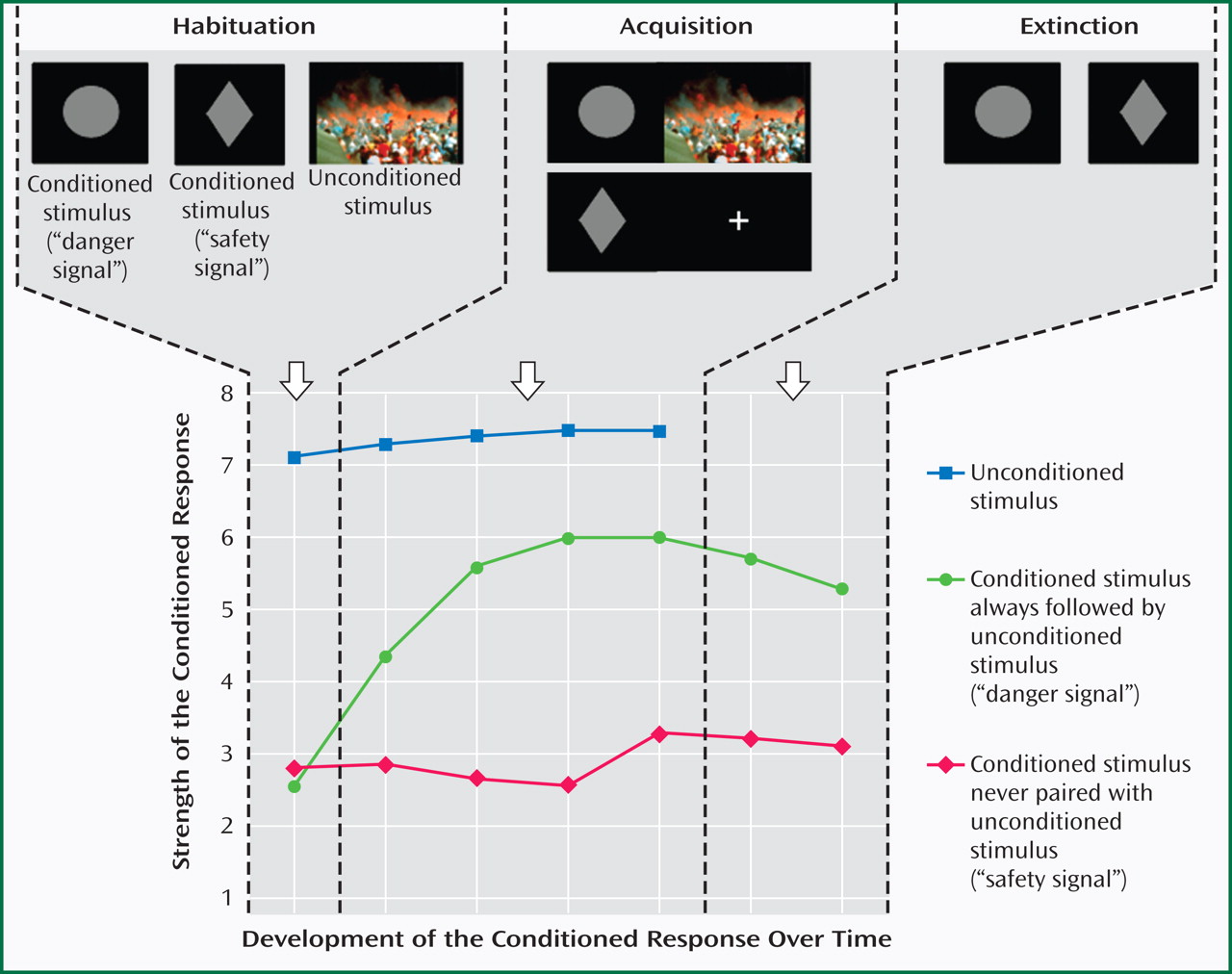
(1) . A fear conditioning model assumes that stimuli that cause an adverse reaction (e.g., air show disaster) become linked with other, neutral stimuli (e.g., airplanes) to produce a conditioned response (fear of airplanes) to these previously neutral stimuli. Over time, the conditioned response diminishes if the conditioned (previously neutral) stimulus is not linked to the negative stimulus. In other words, there is an extinction of the association (
Figure 1 ). The data presented by Wessa and Flor point to a failure of extinction in patients with PTSD and underline the need for pharmaco- and/or psychotherapeutic treatments focusing on the extinction of learned responses.
The study by Litz et al. examines the outcome of an 8-week randomized, controlled trial of Internet-based self-management cognitive behavior therapy versus supportive therapy for PTSD related to attacks on the Pentagon on September 11, or the Iraq war. The rationale of the cognitive behavior therapy employed in this study again largely draws on the fear conditioning paradigm in that it utilizes graduated, self-guided, in vivo exposure designed to relearn/unlearn the association between the conditioned stimulus and the conditioned response, thus facilitating extinction. The data from this trial are promising and show reductions in PTSD, depressive, and anxiety symptoms at 6-month follow-up, thereby providing further evidence for the importance of the underlying mechanism of extinction in the treatment of PTSD. However, insofar as exposure therapy failed to eliminate all PTSD symptoms, the inference is that there are probably additional mechanisms at work.
The investigation by Kilpatrick et al. indicates complex interactions among genetic factors, trauma exposure, and social aspects (social support) in the moderation of risk for PTSD after the 2004 hurricane season. Specifically, this study shows that the low expression variant of the serotonin transporter gene increased the risk for posthurricane PTSD and major depression, but only under the conditions of high hurricane exposure and low social support, thus supporting gene-environment interactions in the modification of risk for postdisaster PTSD. A noteworthy future research direction in the field of PTSD may involve an examination of the relationship between serotonin genotype and extinction. It is interesting that prior work has highlighted the role of genetic variation within the repetitive sequence in the transcriptional control region of the serotonin transporter gene (5-HTTLPR, locus
SLC6A4 ) in altering resting brain function of the amygdala and ventromedial prefrontal cortex
(2), both of which are brain structures that have been shown to play a key role in extinction
(3) . It has therefore been suggested that the serotonin transporter gene may be associated with vulnerability for anxiety disorders by biasing the functional reactivity of the amygdala in the context of stressful life experiences and/or deficient ventromedial prefrontal cortical regulatory input
(4) .
The article by Leserman et al. examines the interactions between extreme experience and physical health. In particular, they explore the occurrence of lifetime trauma and AIDS-related mortality and report that a history of lifetime trauma significantly increases AIDS-related mortality. These data add to the already existing literature pointing to a strong relationship between childhood adverse experience and the later development of physical illness. Felitti et al.
(5) demonstrated in a large HMO sample that adverse childhood experiences are associated with two- to fourfold increases in 10 health risk factors in adulthood, accounting for a significant increase in both morbidity and mortality. These data link the effects of extreme stress throughout the lifespan with both mental and physical illness as well as life expectancy. Research exploring early attachment styles and ruptures and their relationship to biopsychosocial indicators of risk and resilience will need to address the likely complex mechanisms underlying the associations among lifetime trauma, physical illness, and immune functioning.
Finally, the investigation by Yehuda et al. explores cultural influences on the occurrence of histories of sexual abuse in married, observant Jewish women. Examining the cultural aspects of trauma exposure and PTSD is particularly interesting since the personal meaning of traumatic experience is likely influenced not only by the social context but also by the religious context in which it occurs. Yehuda et al. report a prevalence of sexual abuse of 26% in observant Jewish women, which is similar to that reported in several national surveys
(6 –
8), despite the fact that these women are living in a culture with a clearly prescribed set of laws designed to regulate sexual contact. It is also interesting that women who were raised observant reported less childhood abuse than those who became observant later in life, raising the question of whether these women are more likely to seek a religious practice in which sexual restrictions are associated with an increase in personal safety.
These articles ably illustrate how no one mechanism or factor can account for either the development or successful treatment of PTSD. They do describe how complex the biopsychosocial variables are that interact to result in the development of PTSD and issues related to its treatment. In doing so, they raise the issue of how to best attune biopsychosocial treatment strategies to patients traumatized at or throughout different stages of development. The continuing investigation of how biopsychosocial variables interact, in order to describe the mechanisms underlying the development of PTSD, is necessary. Moreover, research is needed to explore the effect of various treatment strategies at different stages of the disorder as well as the question of resilience, or why some people can be exposed to traumatic events without developing PTSD. It is essential for future investigations to maintain a broad approach to research, as exemplified by the articles in this issue, in order to capture the complexities of the factors that predict risk and outcome of traumatic experiences and their extensive and sometimes devastating consequences.