Homelessness among persons with severe and persistent mental illness is the most visible manifestation of failures in mental health policy and in other areas of public policy. Our reading of the body of knowledge about the serious housing problems of those with severe and persistent mental illness suggests that we need a three-pronged policy strategy. The first step is addressing the problem of housing even before addressing the problem of mental illness. This is what we mean by “putting housing first.” Second, we need to make sure that persons with severe and persistent mental illness have access to housing. Finally, if this population is to remain housed, supportive services should be available for those who need them. That is what we mean by “making housing last.”
Although these three strategies emerge from the accumulated body of research and experience over roughly the past two decades, most of what we need to know to translate these ideas into evidence-based policy and practice does not exist. Building this evidence base will require solid, rigorous research that does not cut corners in design or implementation. We propose specific new studies focused on each prong in our policy strategy: First of all, we call for a thorough evaluation of the Housing and Urban Developments (HUD) main housing program for people with disabilities, Section 811. Second, we recommend a study of housing discrimination on the basis of severe and persistent mental illness. Third, we urge the development of a research demonstration program comparing various settings and supportive services approaches.
Homelessness among persons with severe and persistent mental illness is the most visible manifestation of failures in mental health policy and in other areas of public policy. This article presents a focused review of current housing policy for people with severe and persistent mental illness. It is designed to suggest a research agenda to inform this area of public policy. This review is selective and not comprehensive, but it is based on a thorough review of the literature. Our reading of the body of knowledge about the serious housing problems of those with severe and persistent mental illness suggests that we need a three-pronged policy strategy. A detailed critical review of this literature through early 2001 is provided in a previous publication
(1) . We updated this review through early 2007. A synopsis of this update from the perspective of residential stability is shown in data supplement Table 1 (available at http://ajp.psychiatryonline.org).
The first step is addressing the problem of housing, not of mental illness. That is what we mean by putting housing first (Jencks also described housing as “the first step”
[2] ). Housing cannot cure mental illness, nor can it address the myriad problems affecting homeless people, mentally ill or not. But decent, affordable housing would at least give homeless people with mental illness a place to live and might instill greater public confidence in mental health services and related programs.
Second, we need to make sure that persons with severe and persistent mental illness have access to housing. This requires that they be able to negotiate the bureaucratic maze of government housing programs and that landlords be willing to rent to them.
Finally, if this population is to remain housed, supportive services should be available for those who need them. That is what we mean by making housing last. The manifestations of severe and persistent mental illness do not disappear when a mentally ill person becomes housed. To promote housing stability, people need services offering continuity of care.
Although these three strategies emerge from the accumulated body of research and experience over roughly the past two decades, there are other policy issues that might have become the focus of this article. We have chosen these strategies for this focused review because we believe that they are the most important and the most amenable to further research. Most of what we need to know to translate these ideas into evidence-based policy and practice does not exist. Building this evidence base will require solid, rigorous research that does not cut corners in design or implementation.
The Housing Context
The Housing Status of Persons With Severe and Persistent Mental Illness
Three-fourths of the estimated 4.5 million people age 18 and older with severe and persistent mental illness live most of their lives in the community, many in independent housing with no on-site services
(3 –
5) . For the nearly 90% who are not living with family
(6), their housing options are, like everyone else, heavily determined by what they can afford. Most individuals with severe and persistent mental illness are poor, relying on Social Security Insurance and/or Social Security Disability Insurance payments that, at best, amount to roughly a poverty-level income. Even though many receive food stamps, Medicaid, and/or Medicare, which are of enormous help in meeting basic needs for food and medical care, these in-kind benefits do not pay the rent.
From a strictly housing perspective, these in-kind benefits allow the recipient to spend a greater share of income on housing than the typical 30% of income rule-of-thumb, since some basic necessities of life are already being met. But a poverty-level income is insufficient to rent decent housing. According to one analysis, the average rent on a modest efficiency apartment was equal to 96% of the monthly Social Security Insurance payment
(7) .
It is not surprising, therefore, that disabled people, a category that includes individuals with severe and persistent mental illness, are overrepresented among households with what the HUD calls “worst case needs,” that is, very low income renters with housing cost burdens of 50% or more or living in severely inadequate unsubsidized housing
(8) . Even if we ignore other risk factors, the level of economic disadvantage alone among those with severe and persistent mental illness makes it unsurprising that they comprise roughly 30% of the homeless
(6,
9 –
10) .
Housing Programs and Policy
As with other programs designed to provide the basic necessities for vulnerable populations, there are both mainstream housing programs and housing programs specifically earmarked for persons with mental illness. The debate about which approach is best raises a policy dilemma. The strong push for “normalization” means treating persons with severe and persistent mental illness like everyone else. This, in turn, means that individuals with severe and persistent mental illness, like other people with disabilities, have to compete for scarce housing subsidies against all other eligible populations. But because these subsidies are scarce, because the severe and persistent mental illness population is likely to have greater trouble dealing with the bureaucratic maze of subsidized housing, and because persons with severe and persistent mental illness are not the most favored tenant applicants, the question becomes whether the principle of being treated like everyone else is more important than the ultimate goal of getting access to desperately needed housing assistance through a program earmarked especially for them.
Mainstream Housing Assistance Programs
Unlike food stamps and Medicaid, housing assistance is not an entitlement, and operates instead like a lottery. We do not know how many persons with severe and persistent mental illness are lucky enough to gain access to assisted housing. A 1998 analysis by Early
(11) suggests the fraction is extremely low. He estimates that under the targeting criteria for subsidized housing in effect in the late 1990s, increasing the number of subsidized units by 100 would have cut the number of homeless households by less than five. Securing mainstream assistance is typically an arduous bureaucratic journey with a complex application process that would be especially difficult for persons with severe and persistent mental illness because of their functional impairment.
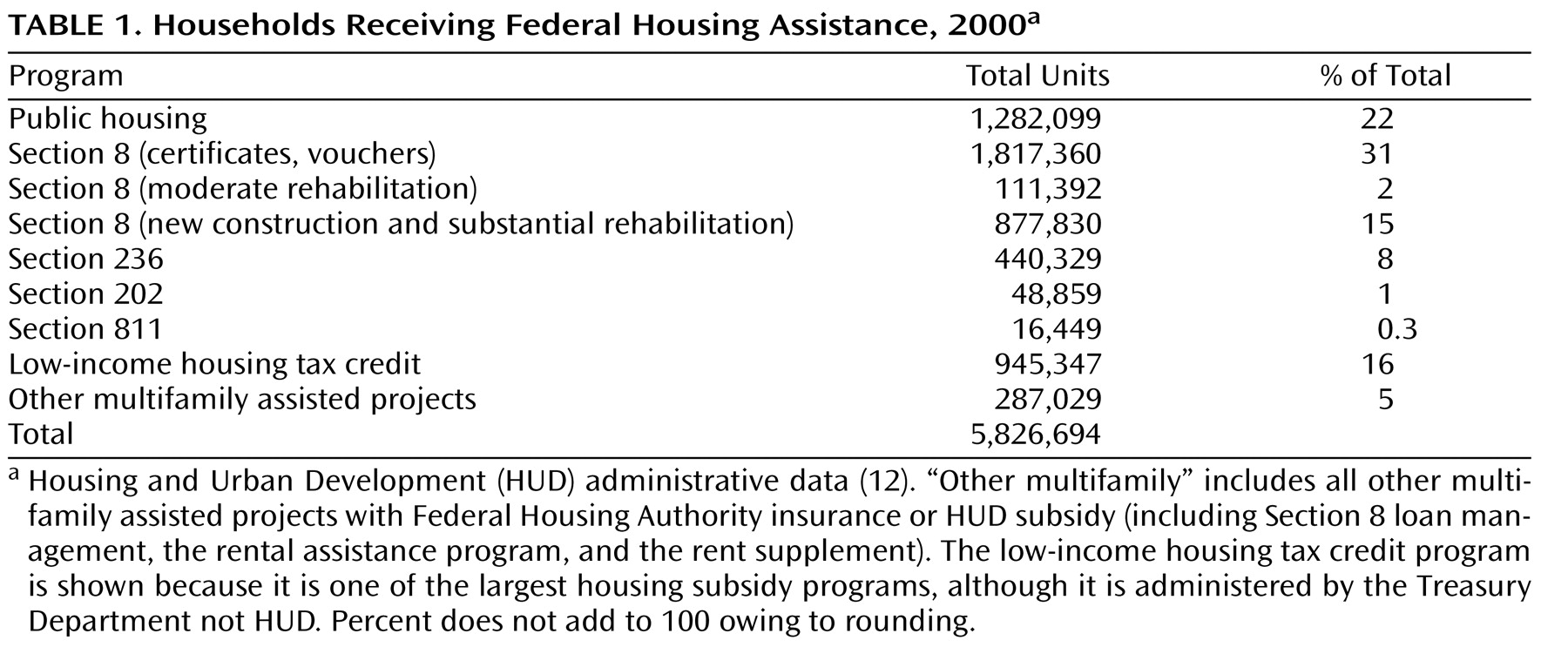
HUD administers three major housing assistance programs: 1) public housing, which consists of housing units typically owned and operated by local public housing authorities; 2) privately owned developments that abide by fair market rent rules in exchange for the concessionary new construction or rehabilitation financing they received from HUD; 3) and housing vouchers, which underwrite the difference between 30% of the household’s income and the fair market rent (see
Table 1 ).
Because of economies of scale, public housing and private assisted housing often take the form of large apartment buildings, and few tenants in any individual building would be persons with severe and persistent mental illness. Vouchers can be used in any rental housing that meets modest rent and housing quality standards. But even if an individual in this population wins the voucher lottery, there is still the challenge of finding a landlord willing to rent to a person with a mental disability. More than 1,500 complaints of discrimination because of a mental disability were filed with HUD in fiscal year 2006 (numbers represent HUD and Fair Housing Assistance Program agencies combined). Fair Housing Assistance Program agencies are state and local fair housing enforcement agencies. (See http://www.hud.gov/offices/fheo/partners/FHAP/index.cfm.) The HUD Office of Fair Housing began collecting data on mental disability in fiscal year 2003.
Research suggests that persons with mental illness have better social functioning and emotional well-being in settings (e.g., apartment buildings) with fewer occupants
(13 –
16) . Once setting size and other factors are controlled, tenant mix also appears to play a role, with a larger proportion of other tenants with mental illness associated with the most beneficial effects
(16,
17) . The typical public housing or private assisted development therefore does not provide the most accommodating environment for persons with mental illness.
Research on the effects of voucher-type independent housing on outcomes for persons with mental illness shows mixed results. For example, some find beneficial effects on housing stability
(18), whereas others do not
(19) . Other researchers, however, report that tenants with mental illness in such housing units report feeling lonely and isolated
(20,
21) . Several studies find that neighborhoods that are socioeconomically and demographically diverse, with a mix of commercial and residential land uses, are associated with better mental health outcomes
(16,
18,
22) . One study also found that neighborhoods with no outward signs of physical deterioration are associated with better outcomes
(16) . Voucher-type units are more likely to be located in such neighborhoods compared with public housing and private assisted units.
This brief review suggests that mainstream housing assistance programs put decent housing within reach of low-income and poor households. But because they are not entitlements, these subsidies are actually out of reach of most eligible households, including persons with mental illness
(11) . Furthermore, the structure type, population mix, and neighborhood location of the average project-based subsidized housing unit are not a good fit for many persons with severe and persistent mental illness.
Earmarked Housing Programs for Persons With Severe and Persistent Mental Illness
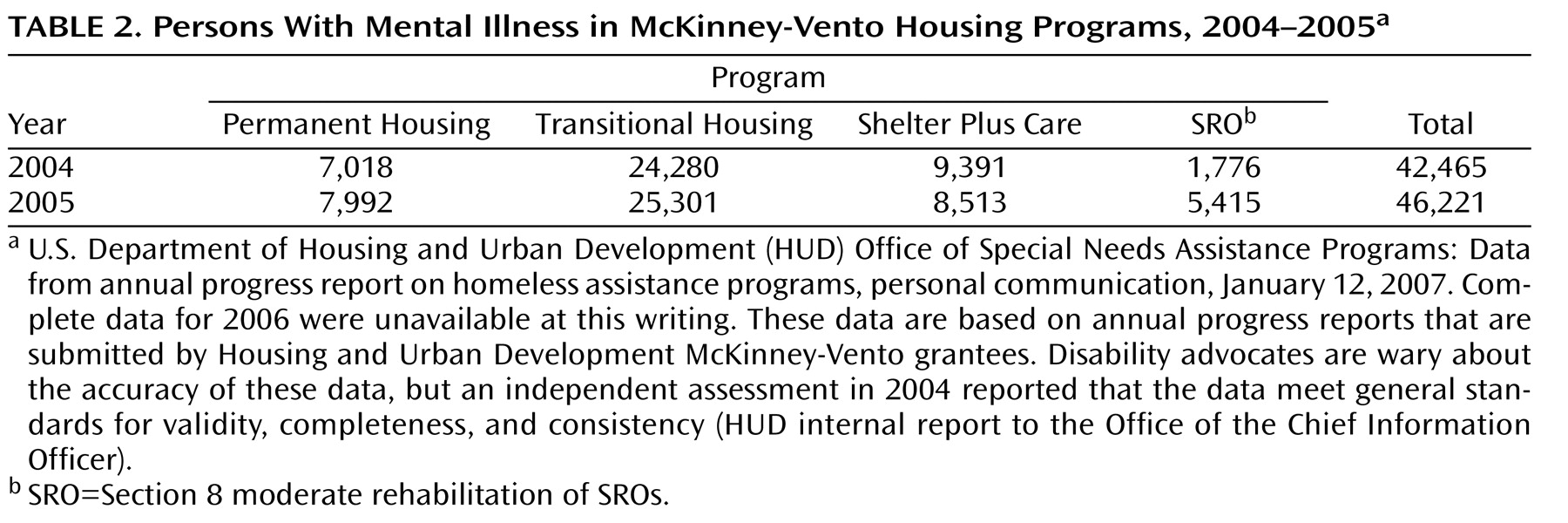
The housing needs of homeless people with a mental illness gained genuine prominence through the 1987 McKinney Act. Although requirements under the act have been changed many times, the core concept of devolution of housing program decision making to local jurisdictions remains. As shown in
Table 2, roughly 44,000 homeless persons with mental illness participated in these programs in 2004 and 2005, about 5% of the annual population of homeless persons with mental illness. In 2000, Burt and Aron
(23) estimated that between 2.3 and 3.5 million persons per year experience homelessness. By using the average of these estimates (2.9 million) and applying the rough estimate that 30% of the homeless are persons with mental illness produces a denominator of 870,000 homeless persons with mental illness over the course of a year (44,000 of 870,000=5.1%). The extent of double-counting, erroneous categorization of individuals as having mental illness when they do not—and the reverse—are unknown.
The main housing program specifically for persons with disabilities is Section 811. As of 2006, 11,223 Section 811 housing units for persons with mental illness had been funded by HUD (HUD, Office Housing Assistance and Grants Administration: Section 811 and Section 202 funding data, personal communications, April 2007). Group homes funded under this program generally must serve eight or fewer persons, and independent living buildings are limited to 20 persons with chronic mental illness. This program appears to be well-suited to the housing needs of this population. There is a deep subsidy for development and operating costs, and the structure type and tenant mix conform to the weight of the research evidence on environments associated with positive effects on the well-being of tenants with mental illness. Unfortunately, the program has not been rigorously evaluated.
Housing, Support Services, and Housing Access: The State of the Evidence
Policy and practice are far ahead of research on housing and serious mental illness. Over the past 20 years, the threshold policy questions have remained the same: 1) How to put housing first: what sorts of housing environments work best, for whom, and under what conditions? 2) What are the impediments to persons with severe and persistent mental illness gaining access to housing, and how can these obstacles be removed? 3) What sorts of support services are required to make housing last to ensure that this population can remain stably housed? In our view, the studies conducted to date do not answer these questions fully.
We see three main suggestive findings in the existing research. First, some persons with severe and persistent mental illness are able to live stably in independent housing in the community. But we do not have a clear sense of who this subgroup is or what mechanisms—such as specific support services—facilitate their ability to live independently. Second, data on complaints filed with HUD suggest a substantial problem of housing access as a result of possible landlord discrimination against persons with severe and persistent mental illness. But no published studies have systematically examined these complaint files to characterize these landlords, where they are located, and the nature of their potentially discriminatory action. Third, various models of case management appear to be associated with fewer days homeless and more days stably housed. But we have few insights into the specific support services that lead to successful outcomes or the effects of combining case management with different housing arrangements on such benefits as housing stability.
Building the Evidence Base
Gaps in research to date arise, in part, because of methodological weaknesses (e.g., assumptions, data, poor documentation of intervention, measures and methods, selection bias, contamination of control or comparison groups). But also important is the lack of a sharp focus on the highest priority policy questions and the application of the best research design and analysis methods to studying these questions. We, therefore, advocate the initiation of a major demonstration and research program to answer the threshold policy questions.
We are calling for a new generation of research on housing, services, and mental illness that strives for the highest standards in order to truly build the evidence base. First of all, we call for a thorough evaluation of the Section 811 program. Second, we recommend a study of housing discrimination on the basis of severe and persistent mental illness. Third, we urge the development of a research demonstration program comparing various settings and support service approaches, building on the design of the San Diego McKinney housing experiment.
The McKinney experiment
(19) provides a general framework on which to build the new demonstration program (also see unpublished work by Hough R et al.). This two-by-two experimental design examines a particular housing and service option, namely, Section 8 housing, which is a completely independent housing unit with no on-site services, and case management. As arguably the most prominent strategies in their respective domains, Section 8 and case management were the right choices for the first experiment of this kind. Furthermore, one of the advantages of focusing on Section 8
access— not use (i.e., intent-to-treat design)—is the opportunity to study the obstacles this population faces in the process of searching for and securing an apartment in the general housing market. But one could also conceive of multiple variations on this general approach, such as studying actual use of a Section 8 subsidy and not only access to it (i.e., treatment on treated) and examining other combinations of housing and service options. To maximize the generalizability of findings, it is worth considering a research design that includes randomized selection of sites as well as random assignment of individuals to experimental and control groups within sites.
We should compare tenant-based and program-based housing, as well as several approaches to delivering clinical and supportive services. This demonstration program also should test the appropriateness of various strategies for individuals with and without co-occurring substance use disorders because this characteristic is considered by some to be a critical issue.
The field has determined that housing needs are preeminent, but for them to be successful, housing solutions must be persistent. We have agreed that we must put housing first, but we have yet to discover how to make housing last.