The mortality from eating disorders is known to be elevated. This is true for both all-cause mortality and suicide, and there is evidence to suggest that suicide mortality may be higher in eating disorders than in any other psychiatric illness
(1) .
Most mortality research in the eating disorders literature has focused on anorexia nervosa, in which suicidal behavior and mortality rates are particularly high
(1,
2) . The limited evidence to date suggests that the mortality risk is low for bulimia nervosa
(3) . This is somewhat surprising, given the medical complications associated with vomiting, laxative abuse, and other purging behaviors
(4) . It is also surprising that observed suicide rates in bulimia nervosa have not been higher, given the association with impulsivity and the high rates of comorbidity with mood, anxiety, and substance use disorders typically observed in bulimia nervosa
(5,
6) . Although eating disorder not otherwise specified (a catch-all DSM-IV diagnosis for patients with significant features of eating disorders not meeting criteria for anorexia nervosa or bulimia nervosa) is the most common eating disorder diagnosis in nearly all community and clinic-based studies of the epidemiology of eating disorders
(7 –
9), virtually nothing is known about the course or complications associated with eating disorder not otherwise specified, including mortality.
The literature on mortality in eating disorders generally has several limitations, including relatively small numbers of study subjects with bulimia nervosa or eating disorder not otherwise specified; the use of clinical follow-up to ascertain vital status; and (in some but not all studies) relatively short follow-up periods. Thus, several important questions remained unanswered. Is the rate of mortality (and in particular suicide) in bulimia nervosa really nearly zero? What mortality risks are associated with eating disorder not otherwise specified? And finally, little is known about the longitudinal course of mortality risk in eating disorders. Does mortality persist at an elevated level throughout the course of the illness, or even after recovery? Does it drop after recovery? Alternatively, does the risk of mortality increase as a result of late complications of eating disorders?
Our goal in this study was to describe mortality associated with eating disorders in a large, diagnostically diverse sample followed up after an extended period through computerized record linkage to death records. We hypothesized that mortality rates would remain persistently high in anorexia nervosa; that there would be an increased mortality risk in bulimia nervosa; and that modest elevations of mortality would be observed in eating disorder not otherwise specified.
Method
Study Population
The patients in this study all presented for evaluation at the Outpatient Eating Disorders Clinic at the University of Minnesota between 1979 and 1997. The clinic provided a thorough diagnostic assessment, referral for further medical assessment as indicated, and referral to the appropriate level of specialized care for eating disorders. A total of 1,885 individuals received treatment evaluation during that period. As part of the initial evaluation, each patient completed an Eating Disorders Questionnaire
(10), which assesses demographic variables; eating disordered behaviors and cognitions; other psychopathology; current and prior treatment experiences; and medical history. The Eating Disorders Questionnaire has been shown to have acceptable diagnostic agreement with structured interview-generated eating disorder diagnoses (kappa=0.64)
(11) . With the questionnaire version of the Eating Disorder Examination
(12), diagnostic agreement for the Eating Disorders Questionnaire has been shown to be fairly high (kappa values ranging from 0.64 to 0.80)
(13) . Body mass index (BMI) was calculated from self-reported weight and height (kg/m
2 ); previous work suggests that self-reported and measured BMI correlate highly in patients with eating disorders
(14) .
Diagnoses were generated from data from the Eating Disorders Questionnaire, based on the following algorithm: for anorexia nervosa, BMI at time of assessment ≤17.5 and fear of weight gain rated as “very much” or “extremely”; for bulimia nervosa, BMI >17.5, endorsement of large binge eating episodes, and endorsement of binge eating at least twice a week for the past month plus vomiting, use of diuretics, laxatives, enemas, fasting, or exercise to compensate for binge eating at least twice a week for the past month. All other patients were considered to have eating disorder not otherwise specified.
National Death Index
The National Death Index (NDI) is a computerized death index
(15) compiled by the National Center for Health Statistics, based on state vital statistics data. The NDI provides vital status information beginning in 1979 for the entire United States including the District of Columbia as well as Puerto Rico and the Virgin Islands. The NDI database is updated yearly; for this study we screened records through 2004. Studies examining the sensitivity and specificity of the NDI using known decedents and known living subjects have shown specificity and sensitivity above 95%
(16 –
18) .
An NDI search uses all available demographic information provided by investigators for the search. For this study, the following identifiers were available: first name, middle initial, and last name; social security number; birth date; sex; race; father’s surname; and marital status. After searching with these data, NDI provides a list of possible decedents, and the investigator must develop a mechanism for making decisions about the vital status of study subjects (see reference
19, for example). The use of such algorithms may be particularly helpful in studies with large numbers of female subjects because of surname changes
(15,
20) . We developed and used an algorithm consistent with previous studies (details are available from the authors).
The NDI provides vital status and a numerical link to death certificates. In this study we also used an NDI Plus search, which provides cause of death, extracted from death certificates. NDI Plus has been shown to be a cost-effective method of obtaining cause of death coding, with very high agreement with expert assignment of cause of death based on actual death certificates
(21) . We then classified causes of death into four groups: suicide, substance use-related, traumatic, and medical.
The study was approved by the University of Minnesota Institutional Review Board prior to initiation.
Statistical Analyses
Statistical analyses were conducted using the computer software programs R (www.r-project.org; with the Epitools package, version 0.5-2, www.medepi.com) and SPSS, release 12 (SPSS, Chicago, 2003)
(22 –
24) . Crude mortality rate, standardized mortality ratio (the ratio of the observed rate of deaths in a population divided by the expected rate, based on the sample’s demographic characteristics), and suicide-specific standardized mortality ratio were calculated for each diagnosis as well as for the entire cohort. Expected mortality for each standardized mortality ratio was derived from age-, race-, sex-, and calendar year-specific national mortality rates published by the National Center for Health Statistics
(22,
23) . Ninety-five percent confidence intervals were calculated by modeling the observed deaths with an exact Poisson distribution.
Results
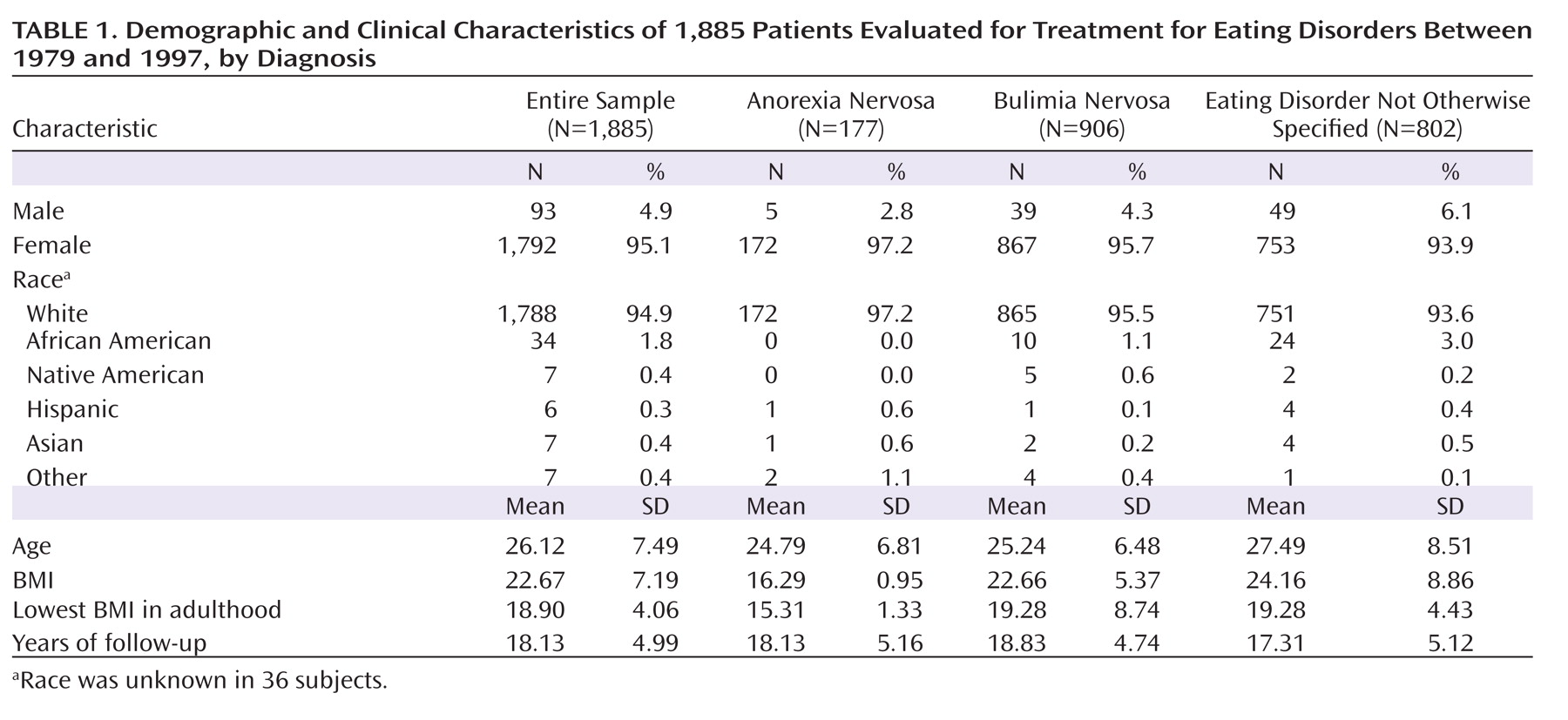
The demographic and clinical characteristics of the sample are summarized in
Table 1 . As expected, the majority (95.1%) of the sample was female. The most common diagnosis was bulimia nervosa (48.1%), followed by eating disorder not otherwise specified (42.5%) and anorexia nervosa (9.4%).
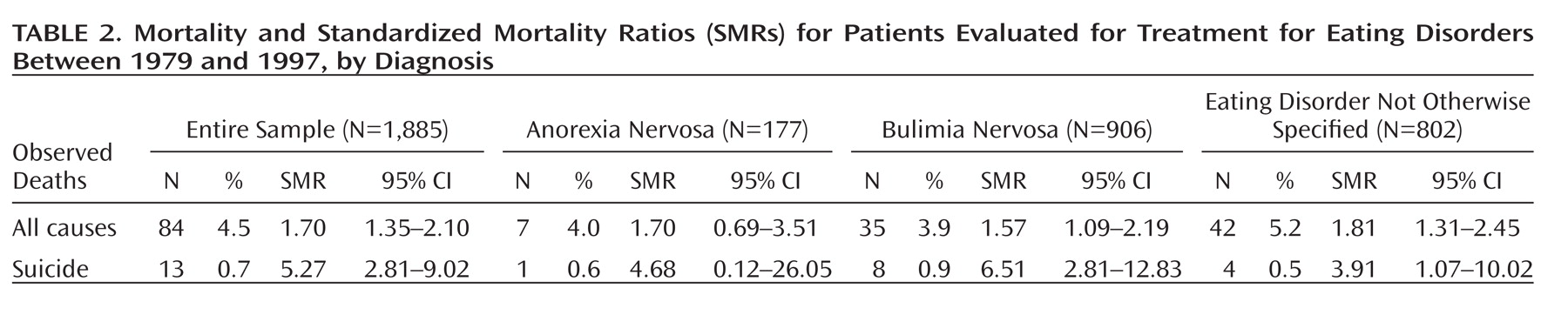
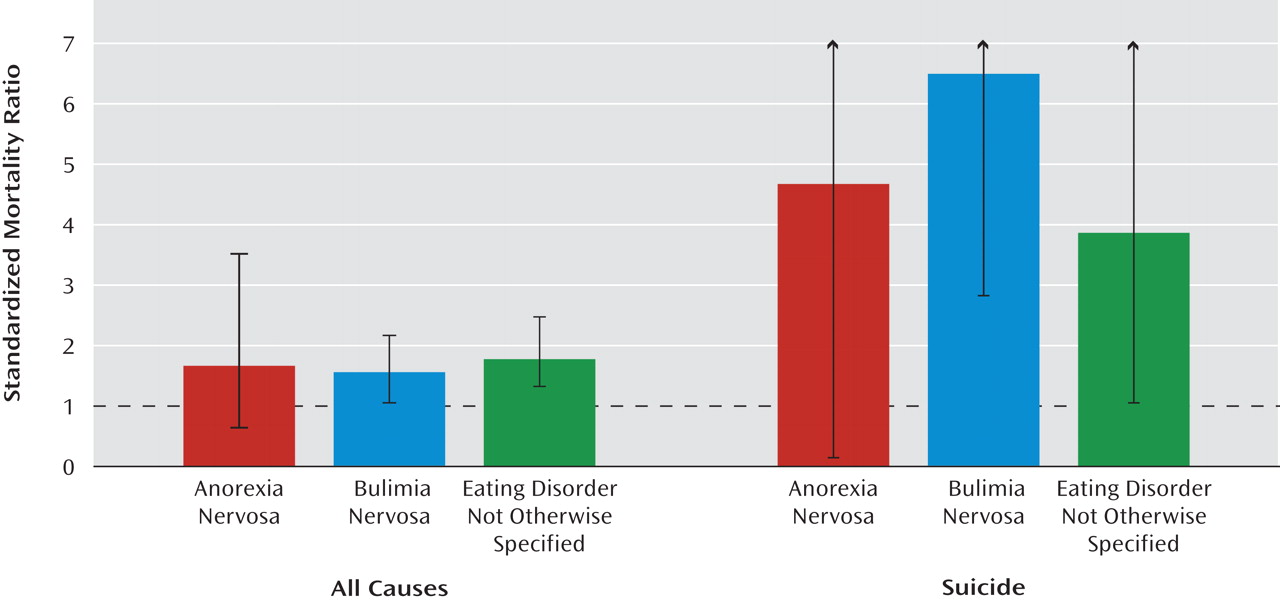
Crude mortality rates and standardized mortality ratios for the entire sample and by diagnosis are listed in
Table 2 and
Figure 1 . The mortality rate for bulimia nervosa (3.9%) was higher than that reported in most previous studies. The mortality rate (4.0%) and standardized mortality ratio (1.70) for anorexia nervosa were lower than seen in some studies. The crude mortality rate for eating disorder not otherwise specified (5.2%) was similar to that seen for anorexia nervosa, and the standardized mortality ratio for eating disorder not otherwise specified was significantly elevated, at 1.81.
The relationship of age to crude mortality and standardized mortality ratio was examined by dividing the sample into five age groups: <20 years, 20–30 years, 30–40 years, 40–50 years, and >50 years. Crude mortality rates in these cohorts were 0.7, 2.3, 1.8, 1.2, and 0.7, respectively, reflecting increases in both expected and observed mortality with age in the sample.
Separate standardized mortality ratios were calculated for suicide mortality (
Table 2 and
Figure 1 ). While the suicide standardized mortality ratio for anorexia nervosa was elevated, it was not statistically significant; by contrast, the elevated risks for suicide seen in bulimia nervosa and eating disorder not otherwise specified were statistically significant.
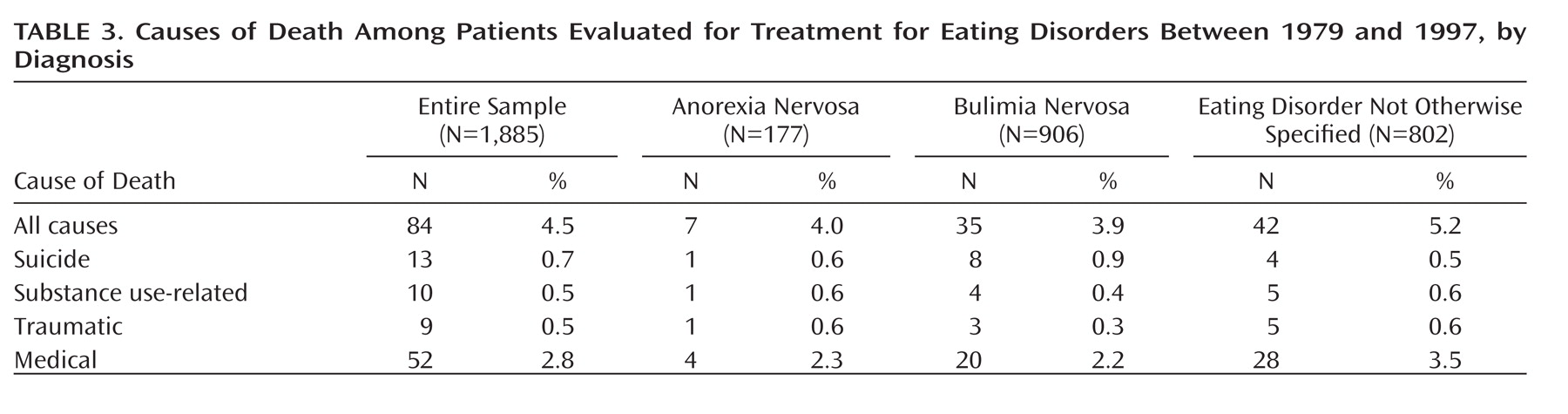
The counts and percentages of the various causes of death are listed in
Table 3, grouped for the sample as a whole as well as by diagnostic category. Notably, “eating disorder,” “anorexia nervosa,” or “bulimia nervosa” was listed in the causes of death for only 6% of decedents (N=5 for anorexia nervosa and N=1 for bulimia nervosa).
Discussion
There are several noteworthy findings in this study. It is the first large-scale examination of mortality in individuals meeting criteria for eating disorder not otherwise specified, and the results suggest that mortality associated with this diagnosis is similar to that seen in anorexia nervosa. The common perception of eating disorder not otherwise specified as a “less severe” eating disorder thus seems unwarranted. In both clinical and research samples, eating disorder not otherwise specified (as currently diagnosed) appears quite heterogeneous, and it seems quite plausible that the elevated mortality seen here is largely contained to certain subpopulations within “eating disorder not otherwise specified.” Understanding these relationships more fully would be of great benefit to efforts to develop new diagnostic nomenclatures (such as in DSM-V). Longitudinal validations of diagnostic constructs are particularly useful, and mortality is an especially important one.
Second, this is one of the largest studies of mortality in bulimia nervosa, and it is notable for the finding of elevated all-cause and suicide mortality in this disorder. As in previous work, mortality in anorexia nervosa was found to be increased, although not as much as in some studies, and the increases in all-cause and suicide standardized mortality ratios were not statistically significant. This somewhat surprising finding may have at least three explanations. First, classification of patients on the basis of current rather than lifetime diagnosis of anorexia nervosa resulted in a smaller sample of anorexia nervosa patients compared to bulimia nervosa or eating disorder not otherwise specified and thus more limited statistical power. Second, it appears that most previous work has used lifetime rather than current diagnosis of anorexia nervosa, and for patients whose diagnostic status evolves, this may lead to assignment of mortality to anorexia nervosa rather than bulimia nervosa or eating disorder not otherwise specified, even if anorexia nervosa was not the most recent or current diagnosis. When all-cause and suicide standardized mortality ratios were reexamined using lifetime diagnosis of anorexia nervosa, the all-cause standardized mortality ratio for anorexia nervosa remained similar but also was statistically significant (1.70, 95% CI=1.04–2.62) and the suicide standardized mortality ratio increased and became statistically significant (6.45, 95% CI=1.76–16.51). Third, the duration of follow-up observation in this sample was greater than in many (but not all) studies; as the duration of follow-up increases, expected mortality increases, and this would tend to diminish standardized mortality ratios.
Patients in this study were seeking treatment in an outpatient clinic setting, and the results should be interpreted in that context. Most previous research on mortality in eating disorders has examined individuals with anorexia nervosa, many of whom appear to have been hospitalized. In the clinical system in which this study was conducted, it was common for patients identified as more severely ill to be referred to the emergency department for evaluation and possible hospitalization; furthermore, many patients were hospitalized in direct transfer from outside care settings. Thus, the decision to first see a patient in the clinic might be understood as a judgment that the patient was less severely ill; the finding of lower overall suicide mortality might support this impression. This point is underscored by a previous study that examined mortality in 122 patients with eating disorders seen in the emergency department of the same hospital system
(24) . That study found higher mortality rates and standardized mortality ratios for anorexia nervosa (more in keeping with the existing literature). Thus, the lower mortality rates observed in the present study might be viewed as a marker of diminished severity of illness in the outpatient setting. It remains unclear how similar the results might be in a community (rather than a treatment-seeking) sample.
This study has a number of strengths, including the large sample and lengthy follow-up period. State-of-the-art methods were used for determining vital status; few other studies have employed NDI in research on eating disorders
(25,
26) . The large cohorts of patients diagnosed with eating disorder not otherwise specified and bulimia nervosa also constitute strengths. Finally, the use of an outpatient sample is relatively novel and broadens our understanding of mortality in eating disorders.
There are also some limitations to this study. First, we did not use state-of-the-art diagnostic methods; rather, diagnosis was based on algorithms using patient self-report data from the Eating Disorders Questionnaire. This limitation was unavoidable, given that data collection began nearly 15 years before the publication of the current structured interview-based standard for diagnostic assessment, the Eating Disorder Examination. The Eating Disorders Questionnaire does not provide a specific illness onset date, so duration of illness could not be examined. Second, data subsequent to the initial evaluation that would have helped clarify factors relating to mortality were not available. For example, detailed information on comorbid psychiatric illness would allow testing of hypotheses about additive mortality risk, but this was unavailable. Third, during the period from which data for this study were drawn, obese individuals with binge eating problems were usually referred to a different, obesity-focused clinic. Thus, individuals with binge eating disorder, a specific type of eating disorder not otherwise specified, were generally not included in this sample. Fourth, the study was conducted at only one clinical site, and site-specific factors might have influenced outcome, thus diminishing generalizability. Fifth, the diagnoses used were intake diagnoses and do not account for diagnostic crossover (for example, from anorexia nervosa to bulimia nervosa) during the follow-up period. Finally, while the NDI yields high-fidelity mortality data, underreporting of suicide as a cause of death is a likely limitation of all methods for determining cause of death.