Recent studies have demonstrated that public mental health patients die as much as 25 years earlier than individuals in the general population, largely as the result of medical causes rather than suicide or accidental death (
1). Standardized mortality ratios for medical deaths among these patients are between 1.5 and three times greater than the rate for persons without mental disorders (
2,
3), and this differential mortality gap appears to be increasing over time (
4).
Poor quality of medical care appears to be an important factor contributing to this excess morbidity and mortality seen in persons with severe mental disorders. In this population, deficits in quality care may explain as much as one-half of the excess death rates from myocardial infarction after hospitalization (
5). These patients may be at risk for poor quality care across a broad range of medical conditions, including diabetes (
6) and asthma (
7), as well as poor routine preventive services (
8) and cardiometabolic risk factors (
9).
A series of provider, patient, and system factors, acting individually and in conjunction, is likely to contribute to the deficits in quality care experienced by persons with severe mental disorders. For mental health clinicians, such factors include lack of knowledge or comfort regarding medical issues and lack of time and resources to address these concerns in their busy practices (
10). For primary care providers, analogous problems include lack of knowledge or comfort with populations with mental disorders as well as clinical demands that make it difficult to address multiple comorbidities (
11). Patient factors include problems directly resulting from mental illness, such as amotivation, cognitive limitations, and poverty, which may lead to deficiencies in patients' capacity to serve as effective agents and self-advocates in obtaining the services they need. System factors include fragmentation and financing challenges that limit the ability to provide medical care within mental health facilities and challenges in referring and coordinating care off-site.
Although there is little research on strategies for improving medical care for persons with severe mental illness, several studies have demonstrated the potential to improve the quality of care in this population (
12). A randomized trial of severely mentally ill patients at a Veterans Affairs (VA) medical center found that an on-site, collocated medical clinic was associated with improved quality of care and health outcomes (
13). Other studies have demonstrated the potential benefits of organized models in linking patients from emergency care to outpatient medical follow-up evaluation (
14) and of providing medical consultation in inpatient settings (
15). Similarly promising results have been found in pilot programs targeting persons with schizophrenia (
16) and bipolar disorder (
17) as well as older populations (
18).
Serving more than 3.5 million adults with mental illness each year, community mental health centers (CMHCs) are perhaps the most important point of entry to the healthcare system for persons with severe mental disorders (
19). Based on the growing literature on excess medical morbidity and mortality in this patient population, CMHC administrators are increasingly interested in assessing and addressing the medical problems of the patients they serve.
However, CMHCs currently have few evidence-based approaches to improve primary care. These centers typically lack the economies of scale and resources to deliver a full range of medical services on-site (
19), making fully collocated approaches less feasible than in larger, quasi-integrated systems, such as the VA healthcare system. CMHCs need to simultaneously address the needs of patients across a range of medical and mental diagnoses, which requires approaches that can be implemented across multiple conditions. Care is likely to require involvement of community medical providers. However, access to and quality of primary medical care for CMHC patients are typically substandard (
20).
In general medical settings, there is increasing interest in the use of care managers to help improve the quality of care and to coordinate care for patients treated across multiple systems. Rather than provide direct medical care, these staff provide education, advocacy, and logistical support to help patients navigate through the healthcare system. Care management is one of the central "active ingredients" of multifaceted approaches designed to improve chronic illness care (
21). It has also been successfully implemented as a stand-alone intervention for major depression (
22) and other chronic medical conditions (
23–
25). Care coordination, one of the core tasks of care managers, has been designated by the Institute of Medicine as a top priority for transforming healthcare (
26).
To our knowledge, this study is the first to test a population-based approach for improving primary medical care in community mental health settings. We hypothesized that participants receiving medical care management intervention would have a greater improvement in the quality of primary care (primary outcome) and health-related quality of life compared with a usual care group.
Method
The Primary Care Access, Referral, and Evaluation (PCARE) study is a randomized trial examining the effect of population-based medical care management on the quality of care for persons with severe mental disorders. All study participants gave written, informed consent, and the study was approved by the Emory University Institutional Review Board.
Study Setting
The study was conducted at an urban CMHC in Atlanta. The target population consisted of individuals age 18 and older from the area who were economically disadvantaged and who experienced serious and persistent mental illness with or without comorbid addictive disorders. The clinic does not provide any formal medical or mental healthcare management or any on-site medical care.
Sample Recruitment
The sample was assembled through a combination of 1) flyers posted at the CMHC, 2) waiting room recruitment, and 3) provider referrals, with approximately one-third of potential subjects identified through each of these three approaches. This hybrid method has been recommended as a strategy for balancing between recruitment efficiency and representativeness in health services intervention trials (
27). To be eligible, subjects had to be listed on the active patient roster at the CMHC, have a severe mental illness (
28), and have the capacity to provide informed consent. Inclusion criteria were purposely kept broad to optimize generalizability to other community mental health settings. Subjects were enrolled between September 1, 2004, and April 1, 2007.
Measures
Reviews of all medical and mental health charts at baseline and the 12-month follow-up evaluation were used to assess the quality of preventive and cardiometabolic care. An interview battery administered at baseline and at the 6- and 12-month follow-up evaluations was used to assess sources of primary care, health-related quality of life, and sites for all medical and mental health service use.
The quality of primary care was assessed at baseline and 12 months using 25 indicators drawn from the U.S. Preventive Services Task Force guidelines. A total of 23 indicators were included across the following four domains: 1) physical examination (blood pressure, eye, height/weight, oral, breast, mammogram, and pelvic); 2) screening tests (cholesterol, fecal blood, HIV, sigmoid, and tuberculosis); 3) vaccinations (influenza; hepatitis B; measles, mumps, and rubella; pneumococcal bacterial infection; tetanus-diphtheria; and varicella); and 4) education (exercise, self-examination, smoking, nutrition, and weight) (
29). The primary study outcome was an aggregate preventive services score, representing the proportion of services for which an individual was eligible that was obtained by the subject.
Among individuals with a cardiometabolic condition (diabetes, hypertension, hypercholesterolemia, or coronary artery disease), quality indicators were drawn from chart reviews using the RAND Community Quality Index study (
30), which includes chart-based quality indicators for diabetes (seven measures), hypertension (28 measures), hyperlipidemia (seven measures), and coronary artery disease (three measures). An aggregate cardiometabolic score was calculated to reflect the mean value for any given individual across these cardiometabolic risk factors. The Framingham Cardiovascular Risk Index, which estimates the 10-year risk of developing incident coronary heart disease, was used to assess the subset of individuals with available values for blood glucose, total cholesterol, and high-density lipoprotein cholesterol. The estimated 10-year risk is calculated on the basis of a weighted score based on age, blood pressure (four levels), smoking status (yes/no), diabetes (yes/no), total cholesterol (three categories), and high-density lipoprotein cholesterol (three categories). This measure required that values be available for all of the components of the summary and thus was considered an exploratory outcome.
Presence of a primary care provider was defined as self-report of a usual source of care other than the emergency room in conjunction with one or more documented primary care visits during the past year.
Health-related quality of life was assessed using the Medical Outcomes Study 36-Item Short-Form Health Survey. Summary physical component and mental component scores can be constructed from the survey (range: 0 [poor health] to 100 [perfect health]) (
31). The oblique method, which is the preferred approach when examining persons with comorbid physical and mental conditions (
32,
33), was selected a priori as the approach for calculating the component summary scores. Individual subscale scores were also calculated to provide context for the summary scores (
34).
Randomization
Using a computerized algorithm, patients were randomly assigned to a care management intervention group or a usual care group by the project manager. After randomization, follow-up interviews were conducted at 6 and 12 months. Interviewers were blinded to subjects' randomization status.
Care Management Intervention
Two full-time registered nurses followed a manualized protocol for care based on standardized approaches documented in the care management literature (
35). The program was designed to help overcome patient, provider, and system-level barriers to primary medical care experienced by persons with mental disorders.
To address patient barriers to primary care, the care manager used strategies to enhance motivation by providing information to the patient about 1) his or her medical conditions, 2) available medical providers in the community, and 3) upcoming appointments. An information booklet was given to the patient, with updated information at each meeting. Motivational interviewing techniques (designed to understand patients' concerns from their frame of reference, monitor their readiness to change, and reinforce their autonomy rather than work through direct persuasion) were used to help support patients' self-management skills (
36). Action plans involving goals for medical care or lifestyle change were used to foster health behavior change as well as to help patients become more active participants in their healthcare (
37).
To overcome the provider barriers to primary care, the care manager served as an advocate for the patient as well as a communication conduit between the patient and specialty medical and mental health providers. The care manager developed and maintained a provider list, and, with the patient's permission, providers were notified about changes in the patient's medication regimen and medical status. Coaching was provided to patients to help them interact more effectively with their providers. The care manager accompanied patients to visits to specialty providers as needed.
To address system-level barriers to care, the care manager worked to help enroll uninsured patients in entitlement programs, including Medicaid (for eligible persons). Public transportation tokens were provided as needed to ensure that patients were able to attend all medical visits. Strategies for troubleshooting factors that may have hindered patients' ability to attend appointments, such as child care, were also addressed.
Usual Care
Subjects assigned to usual care were given a list with contact information for local primary care medical clinics that accept uninsured and Medicaid patients. Subsequently, these subjects were permitted to obtain any type of medical care or other medical services.
Statistical Analysis
All analyses were conducted as intent to treat. Bivariate analyses were used to examine differences between the care management intervention and usual care groups in demographic and clinical variables at baseline (to assess the adequacy of randomization) and at each follow-up evaluation period. The primary analytic technique for assessing statistically significant changes in outcome variables was random regression. This method made it possible to compare the difference in change between groups over time and to conduct intent-to-treat analyses that included subjects with missing data at one or more follow-up evaluation period. Analyses were conducted using the SAS PROC MIXED procedure for continuous variables and SAS PROC GENMOD procedure for binary and ordinal variables (SAS Institute, Cary, N.C.). For each outcome measure, the model assessed the outcome as a function of 1) randomization, 2) time since randomization, and 3) group-by-time interaction. The group-by-time interaction, which reflects the relative difference in change in the parameters over time, was the primary reflection of statistical significance.
Results
Patient Flow
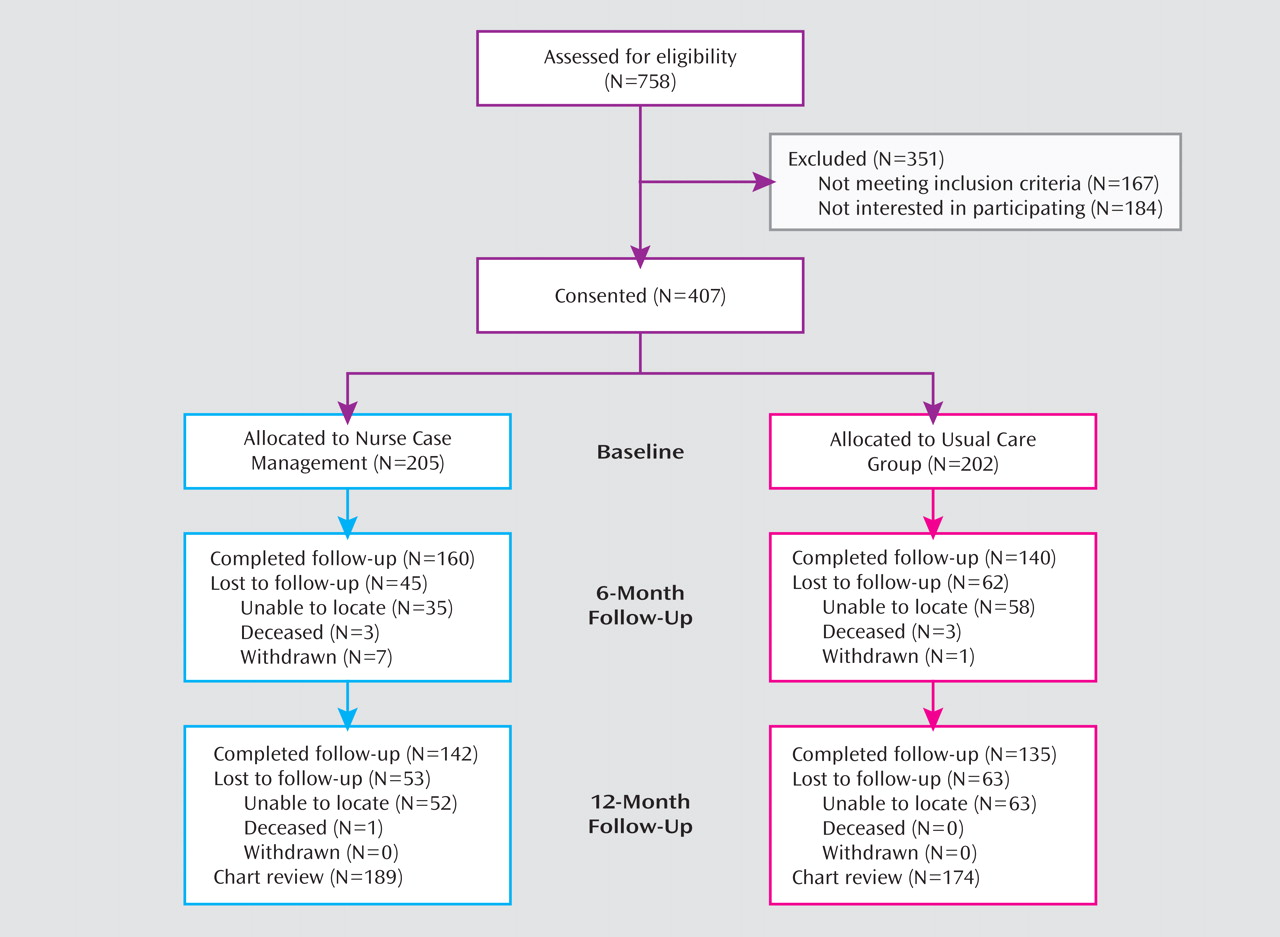
Figure 1 illustrates the flow of patients from screening through the 12-month follow-up evaluation period. A total of 758 patients were assessed for eligibility. Of these, 167 were excluded for not meeting the inclusion criteria (with the most common reason being that they were not listed on the active patient roster of the CMHC), and an additional 184 declined to participate. A total of 407 subjects provided informed consent and were randomly assigned. Of those randomly assigned, 73% completed 6-month follow-up interviews and 68.1% completed 12-month follow-up interviews. A total of eight subjects (2.0%) withdrew during the study period. There were no statistically significant differences on any baseline socioeconomic or clinical characteristics between the intervention and usual care subjects. A total of 89.2% of the sample had complete 12-month chart review data.
Baseline Characteristics
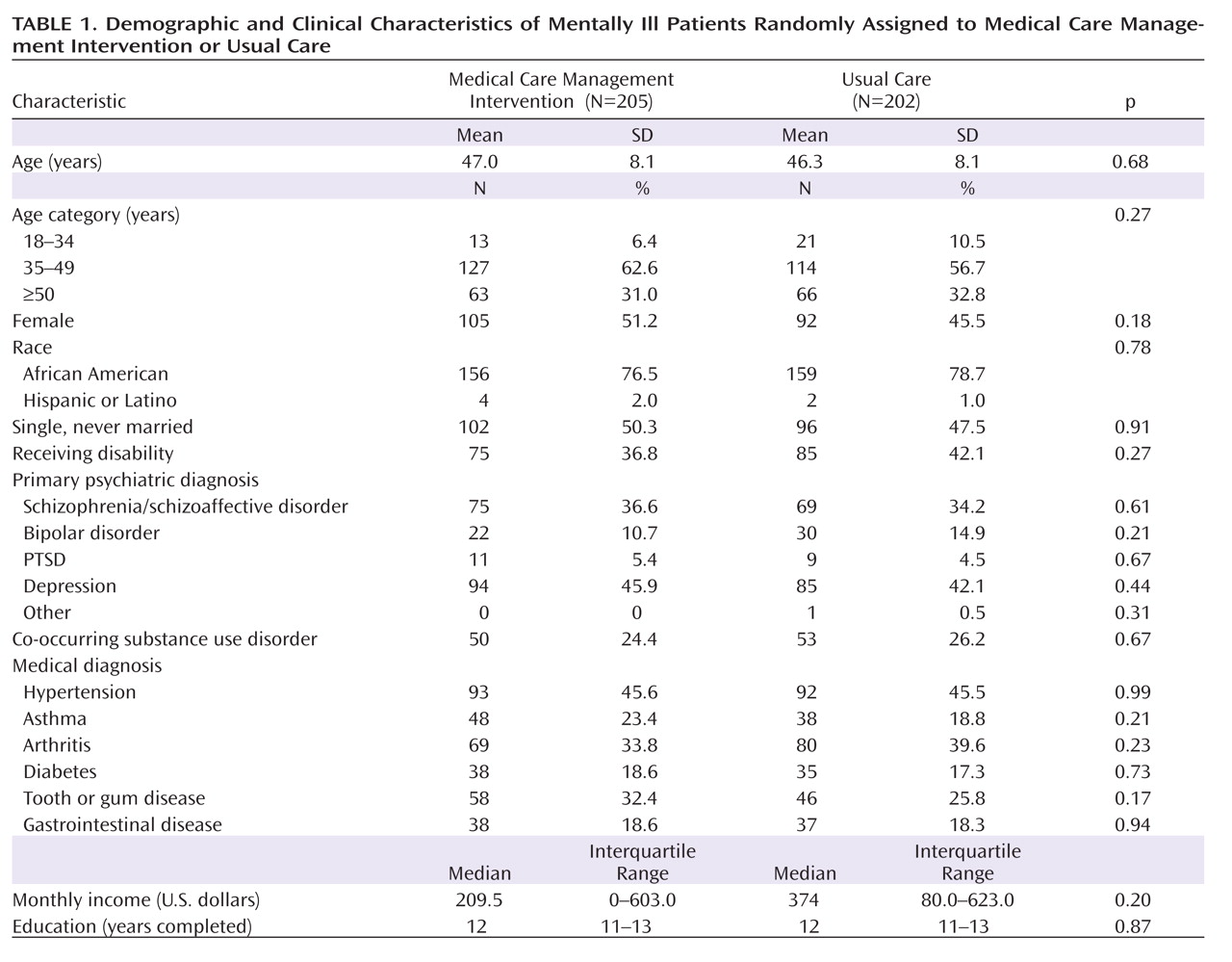
Reflecting the demographic characteristics of the CMHC, the sample was largely African American (77.9%) and poor (median annual income: $3,400) (
Table 1). The most common psychiatric diagnoses were schizophrenia (42.8%), depression (32.7%), and bipolar disorder (17.2%). A total of 25.3% of the sample had a co-occurring substance use disorder. The most common medical comorbidities were hypertension (45.6%), arthritis (36.6%), tooth or gum disease (25.6%), asthma (20.1%), and diabetes (17.9%). There were no significant differences between any of the demographic or diagnostic characteristics at baseline.
Quality of Preventive Services
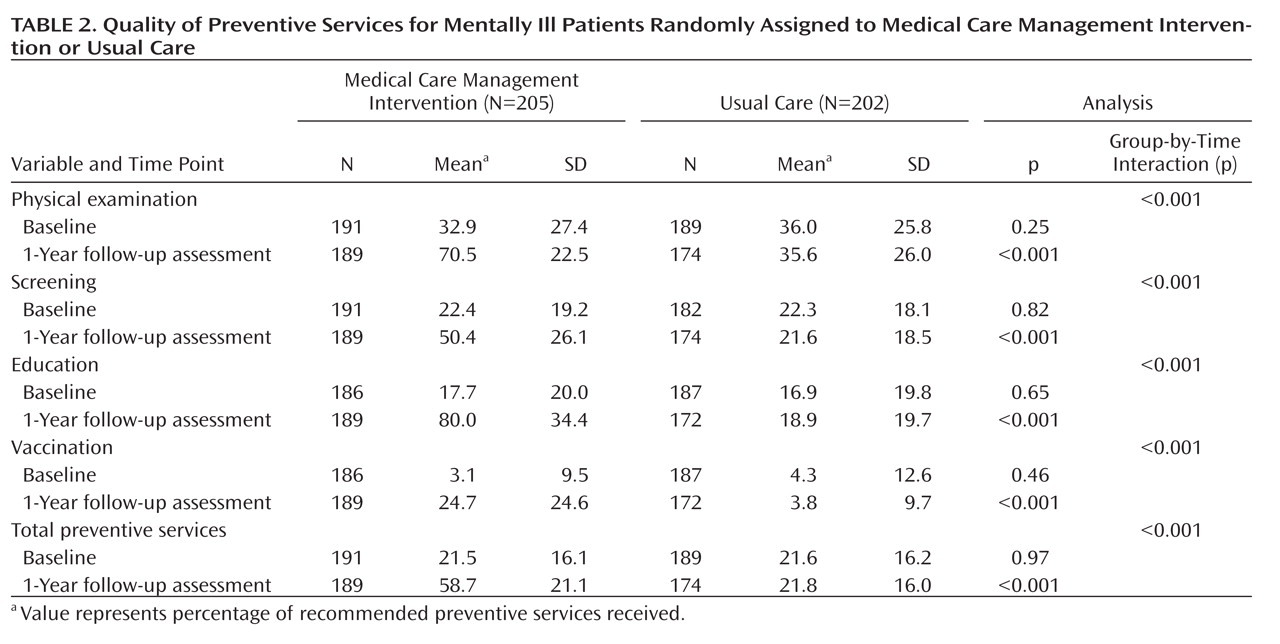
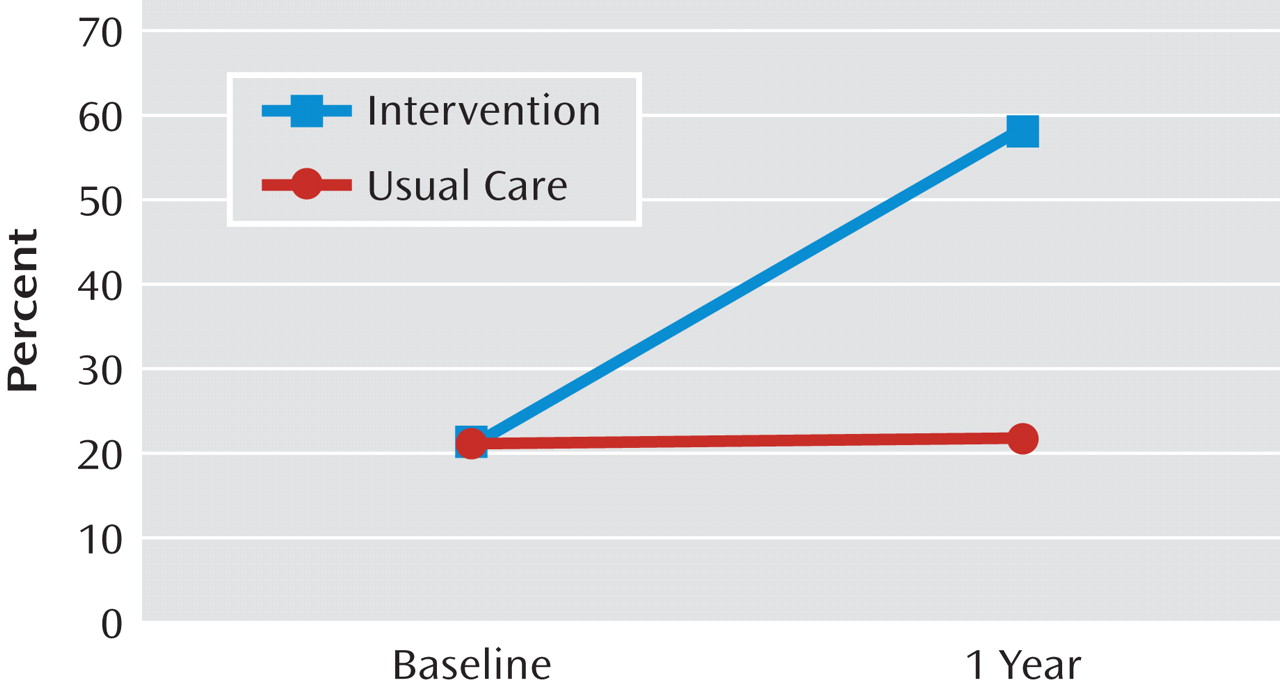
At baseline, there were no significant differences in the quality of indicated preventive care services received by subjects in both the intervention and usual care groups (
Table 2). At the 12-month follow-up evaluation, the average proportion of indicated preventive services more than doubled, to 58.7%, in the intervention group but remained constant in the usual care group (21.8%) (
Figure 2). The group-by-time interaction effect, which indicated the difference in changes between the two groups, was statistically significant (F=272.03, df=1, 361, p<0.0001).
Within individual categories of preventive services, the intervention group had twice as many indicated physical examination activities at the 1-year follow-up evaluation compared with the usual care group (70.5% versus 35.6% [F=166.83, df=1, 361, p<0.001]), more than twice as many screening tests (50.4% versus 21.6% [F=105.93, df=1, 361, p<0.001]), more than four times as many educational interventions (80.0% versus 18.9% [F=410.93, df=1, 353, p<0.001]), and more than six times as many indicated vaccinations (24.7% versus 3.8% [F=100.76, df=1, 353, p<0.001]).
Subjects in the intervention group exhibited significantly greater improvement in sustaining a primary source of care compared with subjects in the usual care group (from 49.5% to 71.2% versus 48.3% to 51.9% [F=10.42, df=1, 310, p=0.001]). Patients in the intervention group were significantly more likely to report one or more visits to a general medical doctor relative to patients in the usual care group (81.8% versus 69.9%, p=0.006) and, among those with at least one visit, had a higher number of primary care visits (N=4.94 versus N=4.11 [F=9.39, df=1, 319, p=0.02]).
At the 1-year follow-up evaluation, a significantly greater number of previously undiagnosed medical conditions were identified in the intervention group (11.9%) than in the usual care group (1.8%) (χ2=10.75, p=0.005). The most common newly diagnosed conditions were hyperlipidemia and hypertension.
Health-Related Quality of Life
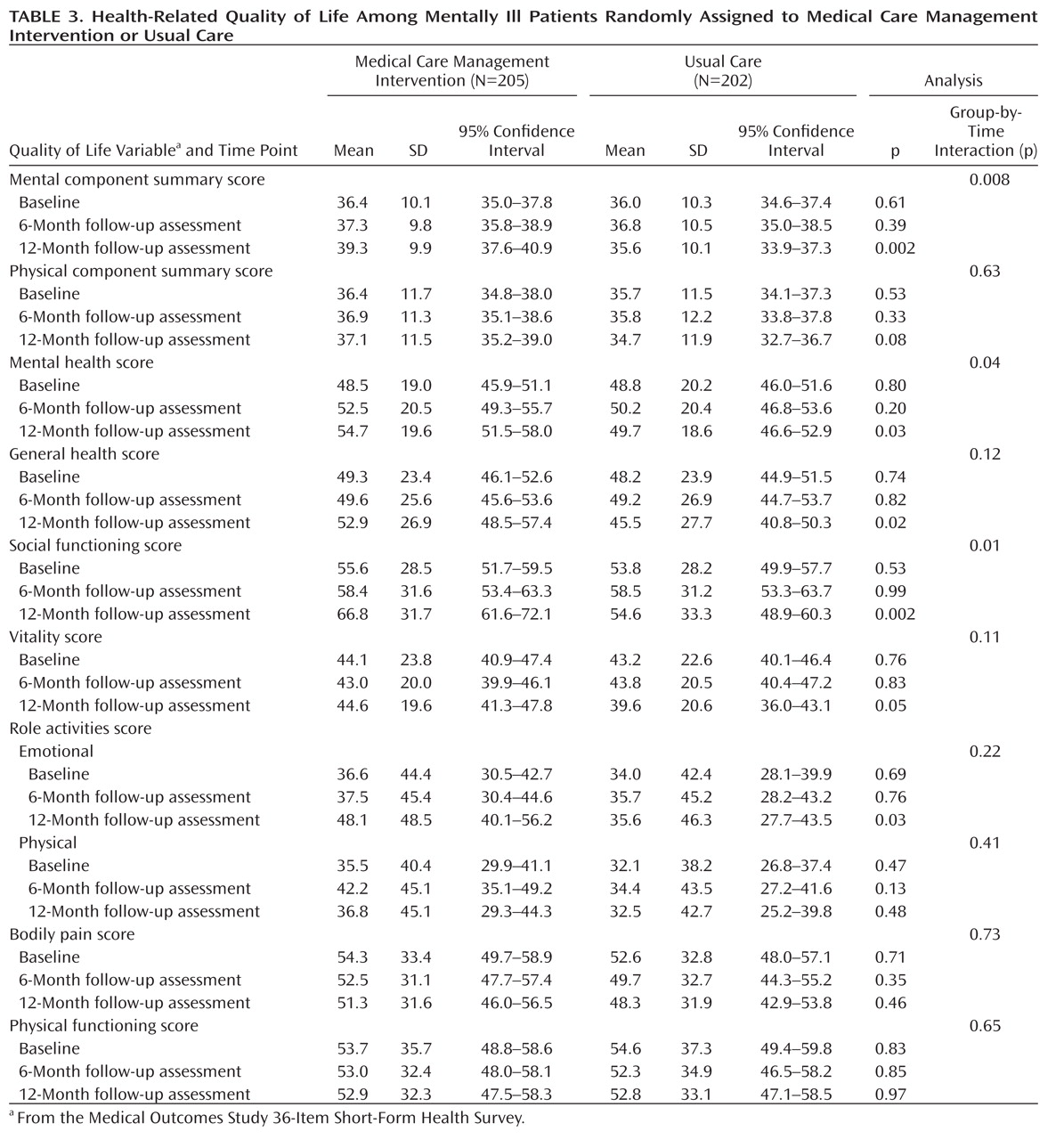
On the 36-item short-form survey, the intervention group showed significant improvement on the mental component summary (
Table 3). At the 12-month follow-up evaluation, the intervention group had a significantly higher survey score than the usual care group (z=–3.15, p=0.002). The difference in change between the two groups (8.0% improvement in the intervention group versus a 1.1% decline in the usual care group) was statistically significant (group-by-time interaction: F=4.87, df=2, 571, p=0.008). Also at the 12-month follow-up evaluation, there was a nearly significant difference in scores on the physical component summary (intervention group, 37.1, versus usual care group, 34.7; z=0.08, p=0.08). However, the difference in change between the two groups was not statistically significant (intervention group, 1.9% improvement, versus usual care group, 2.8% decline).
Examining the specific subscales used to calculate the component summary scores of the short-form survey at the 12-month follow-up evaluation, we found that the intervention group had significantly higher scores on the mental health (z=–2.19, p=0.03), general health (z=–2.27, p=0.02), social functioning (z=–3.09, p=0.002), vitality (z=–1.98, p=0.04), and emotional role functioning (z=–2.21, p=0.03) subscales than the usual care group. The difference in change over time, as reflected in the group-by-time interaction, was significant for the mental health (F=3.22, df=2, 572, p=0.04) and social functioning (F=4.42, df=2, 573, p=0.01) indices.
Quality and Outcomes of Cardiometabolic Care
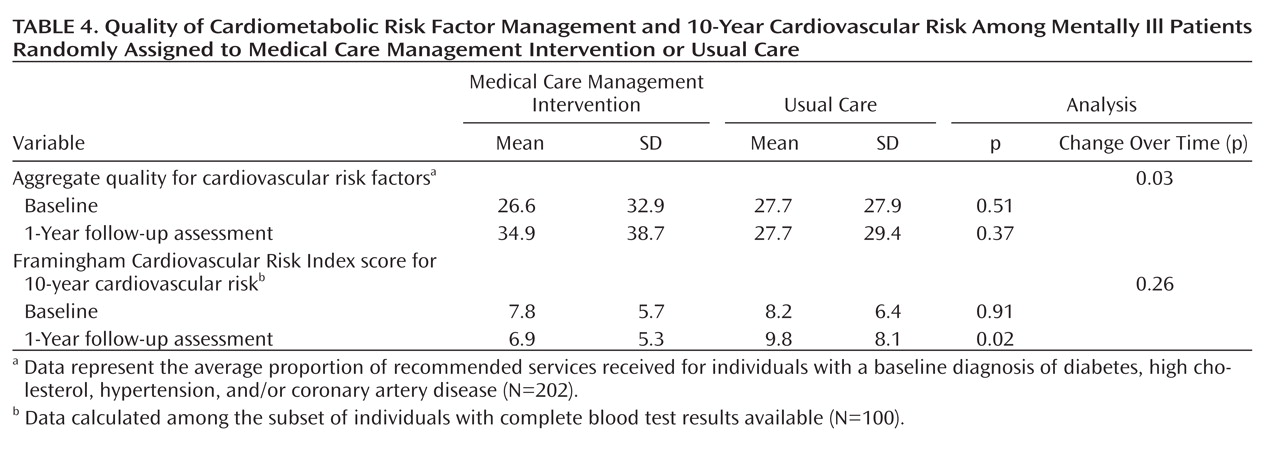
A total of 202 subjects had one or more cardiometabolic conditions (diabetes, hypertension, hypercholesterolemia, or coronary artery disease) (
Table 4). Among these subjects, those in the intervention group had a significantly greater increase in the proportion of indicated services received for cardiovascular disease than those subjects in the usual care group (34.9% versus 27.7%; group-by-time interaction: F=4.90, df=2, 166, p=0.03).
Among those patients with blood test results available (N=100), the Framingham Cardiovascular Risk Index score, which represents the risk of developing cardiovascular disease in 10 years, was significantly lower at the 1-year follow-up evaluation among subjects in the intervention group relative to subjects in the usual care group (6.9% versus 9.8%; z=2.23, p=0.03). The intervention group showed an 11.8% rate of improvement (decrease in risk) at the 1-year follow-up evaluation (from 7.8% to 6.9%), and the usual care group showed a 19.5% increase in risk during this period (from 8.2% to 9.8%). This change, while clinically significant, was not statistically significant in the group-by-time interaction.
Discussion
The PCARE study, a population-based, care management intervention, demonstrated a rate of evidence-based preventive medical services that more than doubled among individuals with severe mental illness. There was a significant improvement in 1) care for cardiometabolic conditions, 2) the presence of a primary source of care, and 3) mental health-related quality of life. These results suggest that care management can be a useful strategy for improving the quality of medical care in community mental health settings.
Medical care management intervention showed a clinically and statistically significant effect on the primary study outcome, which was the quality of primary care. Despite the fact that the care managers did not provide any direct medical services, they were able to facilitate improved primary care in the community through a combination of advocacy, education, and helping patients overcome logistical barriers to care. These findings are consistent with a growing body of literature suggesting that there are benefits of care management models for vulnerable populations in general medical settings. For instance, "guided care" has been shown to be effective in improving care in elderly patients with multiple comorbidities (
23,
24), and "patient navigators" are increasingly used for cancer screening and treatment in underserved populations (
25). Persons with severe mental disorders share common features with these populations, including high levels of medical comorbidity, limited health literacy, and fragmentation within the systems designed to serve them.
In the present study, medical care management intervention was associated with a significant improvement in mental, but not physical, health-related quality of life. Recent psychometric studies of the short-form Medical Outcomes Study survey have raised questions about the distinctiveness of the physical and mental component summary scales, noting that many of the same items load onto both scales (
32–
34). In our study, the psychosocial support provided to help patients obtain medical services may have contributed to improved mental health status. At the 12-month follow-up evaluation, there were significant differences between intervention and usual care subjects on the short-form survey subscales, including for mental health, social functioning, and emotional role functioning. Although there was not a significant change in the physical component summary scores, there were substantial and statistically significant differences between intervention and usual care subjects by the 12-month follow-up evaluation in the general health and vitality subdomain scores. Changes in other physical subscale items that load onto the physical component summary, such as physical functioning (which measures strength and mobility), would be expected to take a longer time to become evident, particularly in populations with long-standing medical problems or disabilities.
Several features of the PCARE study management model make it an appealing approach for community mental health clinics seeking to improve their patients' medical care. Compared with collocated approaches, care management is relatively inexpensive to implement and practical for even relatively small sites that do not have the financial or staffing resources to establish fully functioning medical clinics on-site. Existing mental healthcare managers can be retrained to add medical services to their scope of activities. Finally, a rationale for CMHCs to address primary care services among their clients may be provided by the fact that improving medical care might be associated with better mental health outcomes.
However, care management programs are ultimately dependent on the accessibility and quality of primary medical care in the community. These challenges are likely to be most salient for services requiring intensive and ongoing input from a prescribing physician. Although medical care management intervention in our study was associated with significant improvement in the quality of care for cardiometabolic conditions, individuals in the intervention group received less than one-half of indicated treatments for these risk factors. Despite this finding, the study did show improvement in the risk of cardiovascular disease among intervention subjects that was of an effect size comparable to that seen in underserved populations without mental disorders (
38). Given that cardiometabolic disorders are the most important causes of excess mortality in persons with severe mental disorders (
9), this study suggests the potential for care management programs to have a positive effect on cardiometabolic outcomes. More intensive models that include a prescribing provider may hold promise for improving the quality of cardiometabolic care and outcomes in this population. Longer follow-up evaluation periods will also be important for assessing the effect of these programs on physical health and functioning outcomes.
Two limitations to the study should be noted. The broad entry criteria, although optimizing practicality, hindered the statistical power to examine outcomes for individual medical conditions. Second, because the study was only conducted in a single site, replication would be needed to fully assess generalizability to different types of community mental health settings (for instance, rural regions with limited geographic access to medical providers).
The problem of excess morbidity and mortality in persons with severe mental illness is now gaining significant policy attention and traction. The 2009 Omnibus Appropriations Act spending bill included $7 million to hire primary care staff for CMHCs nationwide, which is being distributed through the Substance Abuse and Mental Health Services Administration as a series of demonstration grants (
39). The present study suggests that as these efforts move forward, care management should be a central component of models for improving health and healthcare in this vulnerable population.