Promoting national adoption of electronic health records (EHRs) has been a bipartisan endeavor, with similar goals for wide-scale adoption articulated by the previous presidential administration and the current one. EHRs have been framed as an integral component of health care reform and have been lauded for their potential to improve health care quality and efficiency. The recent stimulus bill, the American Recovery and Reinvestment Act of 2009, is expected to accelerate EHR use, with billions of dollars set aside for incentives to physicians and hospitals for EHR adoption. The selection and implementation of an EHR system can be a challenging and laborious undertaking, and the resulting improvements may be accompanied by new complications. Consequently, EHRs have the potential to introduce many enhancements as well as new challenges to the practice of psychiatry.
An EHR is an electronic repository of health information that incorporates features such as maintenance of lists of current problems and medications, clinical notes, electronic transmission of prescriptions, and provision of clinical decision support at the point of care. A key goal of widespread EHR adoption is ready access to all of a patient’s relevant health information regardless of when and where the care was delivered. Aggregation from multiple clinical settings will require that diverse EHRs be interoperable, i.e., able to exchange information in a format that can be used by other EHRs. A parallel entity that has also gained attention is the personal health record, or PHR. Unlike an EHR, which is maintained in a clinical setting, a PHR is controlled by the individual patient. The individual may choose which clinical information to include in the PHR and with whom it should be shared.
Much of the national EHR activity is centered at the Office of the National Coordinator for Health Information Technology, currently led by David Blumenthal, M.D. The various entities overseen by this office focus on different aspects required to define and encourage adoption of EHRs, including policy, technical standards, and certification that EHRs meet certain functional criteria. Starting in 2011, physicians who treat Medicare or Medicaid patients will be eligible for incentives of up to $44,000 over 5 years if they can demonstrate “meaningful use” of EHRs, and clinicians who are not using EHRs by 2015 will be subject to financial penalties. While the requirements of “meaningful use” had not yet been finalized by the Department of Health and Human Services when this was written, a proposed rule was issued in December 2009 and includes features intended to improve quality and safety (e.g., drug-drug interaction checking, incorporating laboratory results into the EHR, integrated performance measures), increase patient and family access to their clinical information, improve exchange of information among clinicians and thus care coordination, make certain data accessible to public health agencies, and protect privacy and security (
1). These criteria will evolve over time as new EHR products and capabilities emerge.
EHRs have the potential to enhance clinical workflow by increasing legibility and reducing time lost in locating records. Additional benefits may be realized by making pertinent, patient-specific medical references, clinical practice guidelines, and information on potential medication interactions and known allergies available at the point of care. Trends can be visualized by graphically displaying numeric values, such as medication blood levels and psychiatric measurements. Remote access makes clinical information available to clinicians regardless of their location. Templates can be employed to simplify complex documentation tasks, such as behavioral health treatment plans. Novel features will continue to emerge as EHR products evolve and are customized for specific settings and specialties.
Wide-scale EHR adoption could overcome many of the limitations of documenting and transmitting paper-based records. Discharge notes can be delayed or misplaced even if the outpatient clinician is known at the time of discharge. Previously recorded medical history, while critically important in clinical encounters such as psychiatric emergencies, remains locked in inaccessible or unknown paper records, leaving much of the burden of reporting it on the patient or family. Patients often receive care in multiple settings by an interdisciplinary assortment of clinicians, but clinical information is often isolated in each practitioner’s individual records, unavailable to others on the treatment team. Interconnected EHRs have the potential to expand the sources and types of clinical information available at the point of care and may be particularly valuable in emergencies or when patients are unable to communicate information effectively.
There are many potential benefits to public health as well. Structured EHRs could greatly increase chart review efficiency and feasible sample size, providing more robust information for clinical and public health research and earlier identification of emerging trends. Another proposed national goal for EHRs is to provide a platform for performance measurement, intended to facilitate quality improvement by drawing attention and resources to practices and clinical outcomes where there is an established gap in care.
Accompanying such benefits of EHRs are other facets that may be problematic. Potential vulnerabilities of EHRs have been illustrated by high-profile incidents involving misconfigured web sites, lost laptops and CDs, and hospital staff inappropriately viewing celebrities’ records. These breaches of privacy erode the trust critical to a productive therapeutic relationship and may cause individuals to withhold critical information from clinicians because of concerns over how it will be disclosed (
2). Large-scale thefts of personal information, such as credit card account numbers, illustrate that without strict security safeguards, electronic information is susceptible to compromise. This risk is compounded when the responsibility for maintaining a secure electronic environment falls on small clinical settings that do not possess security expertise. Given the wide range of individuals and stakeholders who may have access to EHRs, it is not difficult to imagine scenarios in which information on health issues such as mental health, reproductive history, infectious disease, or cancer diagnosis could lead to personal, professional, or financial harm. Knowledge of the vaster audience of individuals with access to electronic records could influence clinicians’ decisions pertaining to documentation or even diagnosis of potentially stigmatizing illnesses. Clinicians will need to weigh with their patients the potential harm resulting from inappropriate access to sensitive information versus the potential risk that other health care professionals may not have access to important information. Technology may allow for sophisticated protections that are unavailable for paper records, such as a detailed audit trail of who has accessed records and isolating and restricting access to sensitive information. Nevertheless, inability to protect privacy remains a significant unresolved concern.
There are other concerns beyond doubts about privacy protection. Selecting and implementing an EHR can be complex and costly, particularly for resource-limited small practices. That most EHR products available today target general medical, rather than psychiatric, settings only exacerbates this challenge. Productivity is often reduced during the initial implementation phase (
3). New types of errors, such as distorted and inaccurate clinical notes resulting from the ability to copy and paste preexisting documentation (
4), are not well studied. Documenting with a computer during the clinical encounter may result in diminished eye contact or clinician distraction that detracts from the therapeutic relationship, whereas documenting after the clinical encounter may take extra time or lead to loss of unrecalled information. Poorly designed interfaces and excessive or intrusive alerts will also hinder clinical workflow and foster aggravation. Clinicians often must commit to a specific EHR system before fully experiencing its strengths and weaknesses firsthand, since there is no straightforward way to transition from one system to another. Those endeavoring to adopt an EHR, regardless of the system selected, should be aware of potential complications and limitations.
Despite the unanswered questions and potential consequences, one of the rare points of broad agreement in the ongoing national health care reform debate is that EHRs will play a prominent role (
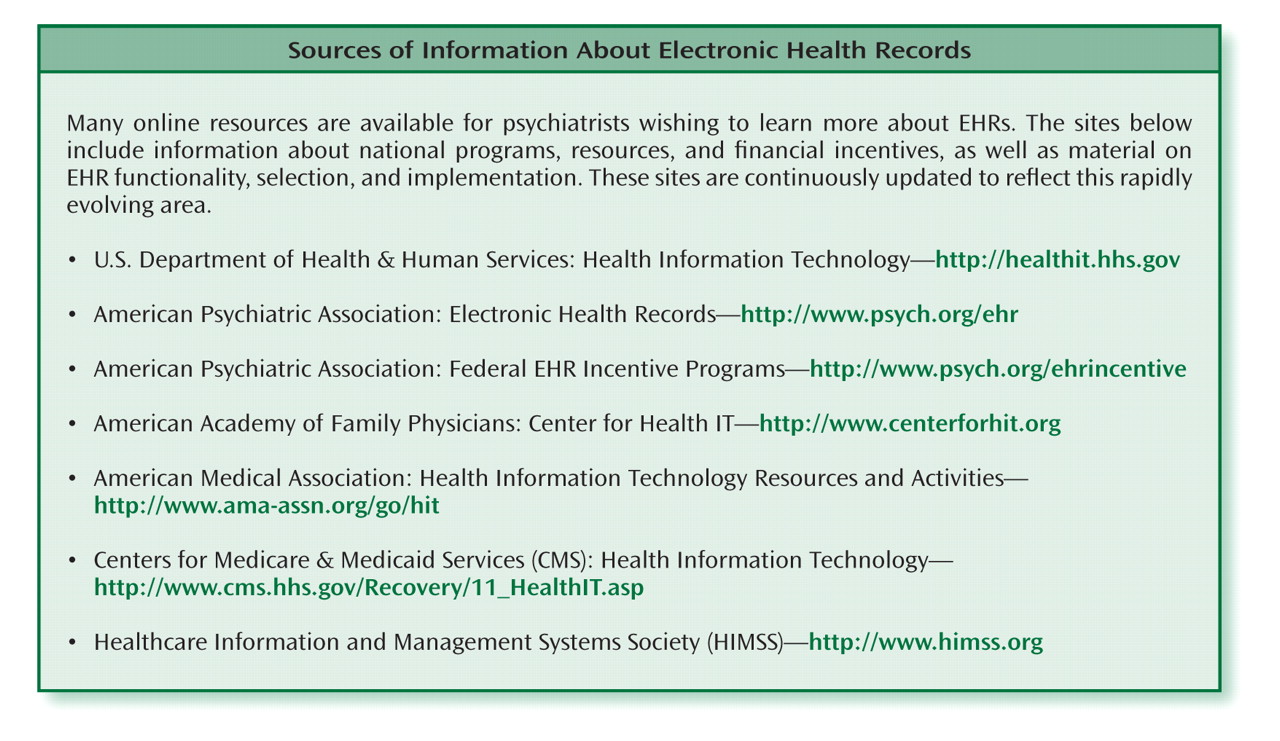
5). The outcomes of rapidly evolving discussions and decisions about financial incentives for adoption, technical standards, and EHR products are likely to have an impact on what EHRs can do and how health information technology is used for years to come. It is vitally important that this dialogue engages not just information technology experts and health care administrators, but also clinicians and patients. APA is among the professional organizations providing educational information online and at membership meetings as well as monitoring and participating in national EHR initiatives. However, psychiatrists will need to be engaged in efforts at the individual, institutional, local, state, and national levels to ensure that the needs and perspectives of mental health clinicians and patients are met.