This group of antigens includes antibodies against voltage-gated potassium channels, antibodies against the N-methyl-D-aspartate (NMDA) type of glutamate receptors, antibodies against --amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors, and antibodies against s-aminobutyric acid type B (GABAB) receptors.
Antibodies Against Voltage-Gated Potassium Channels
These antibodies are usually associated with nonparaneoplastic limbic encephalitis, but they can occur in the context of an underlying tumor (20% with small cell lung cancer or thymoma) (
21,
53). The disorder typically affects middle-aged or older patients, who develop severe verbal and visual memory deficits and confusion or disorientation (
21,
22,
54). Seizures are common, but CSF pleocytosis is rare in syndromes with antibodies against voltage-gated potassium channels, which is not the case in classic limbic encephalitis (
21,
53).
A survey of case descriptions of patients with voltage-gated potassium channel antibodies illustrates more diffuse psychiatric disturbances than occur in classic limbic encephalitis (described earlier). Behavioral changes are frequent and often include apathy and irritability (
21,
22). These symptoms may occur concurrently with signs of autonomic dysfunction, such as excess sweating and salivation (
21,
22). Visual hallucinations have also been described (
22,
54), although this symptom is rare in comparison to memory dysfunction. In addition, associations between this syndrome and hyponatremia (
21,
22), hypothermia (
54), and REM sleep behavior disorder (
55) have been reported. Despite the clinical variability in presentation, review of the literature highlights memory impairment as a core finding.
Antibodies recognizing voltage-gated potassium channels are well known to underlie the neurological abnormalities in Isaacs and Morvan syndromes, characterized by neuromyotonia, hypersalivation, hyperhidrosis, and insomnia (
21). Although some of the clinical symptoms of Isaacs and Morvan syndromes exist in encephalitis caused by antibodies against voltage-gated potassium channels, the predilection for limbic areas is not well understood. Perhaps antibodies in these distinct disorders are subtly different and target peripherally, rather than centrally, expressed potassium channel subtypes (
21,
56). It is also not known how antibodies against voltage-gated potassium channels result in memory deficits, although modulation of neuronal excitability likely plays a role (
22) and a knockout animal model lacking one of the channels expressed in the hippocampus does display memory impairment (
57).
A significant distinction between limbic encephalitis caused by antibodies against voltage-gated potassium channels and limbic encephalitis due to other causes is the rapid response to immunotherapy. About 80% of patients improve neurologically and radiologically following prompt (within 2 months) treatment with high-dose steroids, intravenous immunoglobulins, or plasma exchange (
21,
22); neuropsychological improvements have been noted but are less robust. While most patients show a large degree of cognitive and behavioral recovery, the majority still experience short-term memory deficits, although less serious than at symptom onset (
21,
22). Given the prognostic outcome with immunotherapy, prompt recognition and diagnosis of this syndrome is crucial, a fact emphasized by work demonstrating relatively poor improvement with more prolonged symptoms (greater than 9 months) prior to treatment (
21).
Anti-NMDA Receptor Antibodies
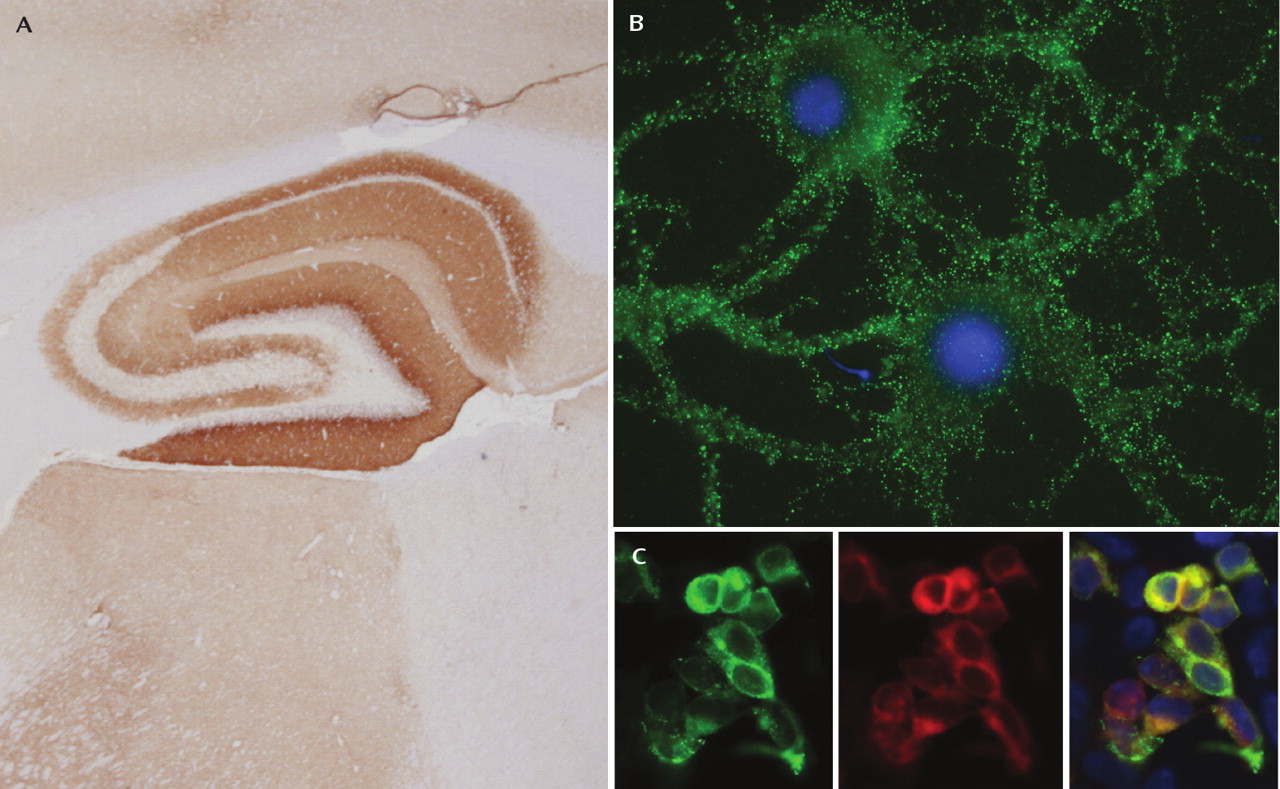
Perhaps the most intriguing disorder with regard to psychiatric symptoms is the autoantibody syndrome involving the NMDA-type glutamate receptor. NMDA receptors are ionotropic glutamate receptors with well-known roles in synaptic transmission and plasticity (
58), as well as in neuropsychiatric disease (
59). Antibodies in this syndrome recognize the NR1 subunit (
Figure 4), which normally combines with various NR2 subunits (A–D) to form heteromers with distinct properties (
59). Although the antibody was only identified in the last few years, about 200 patients have now been described with this disorder, and nearly 75% were seen by a psychiatrist or initially admitted to a psychiatric unit (
7). Because of the constellation of symptoms, patients were often misdiagnosed with acute psychosis, malingering, or drug abuse (
60).
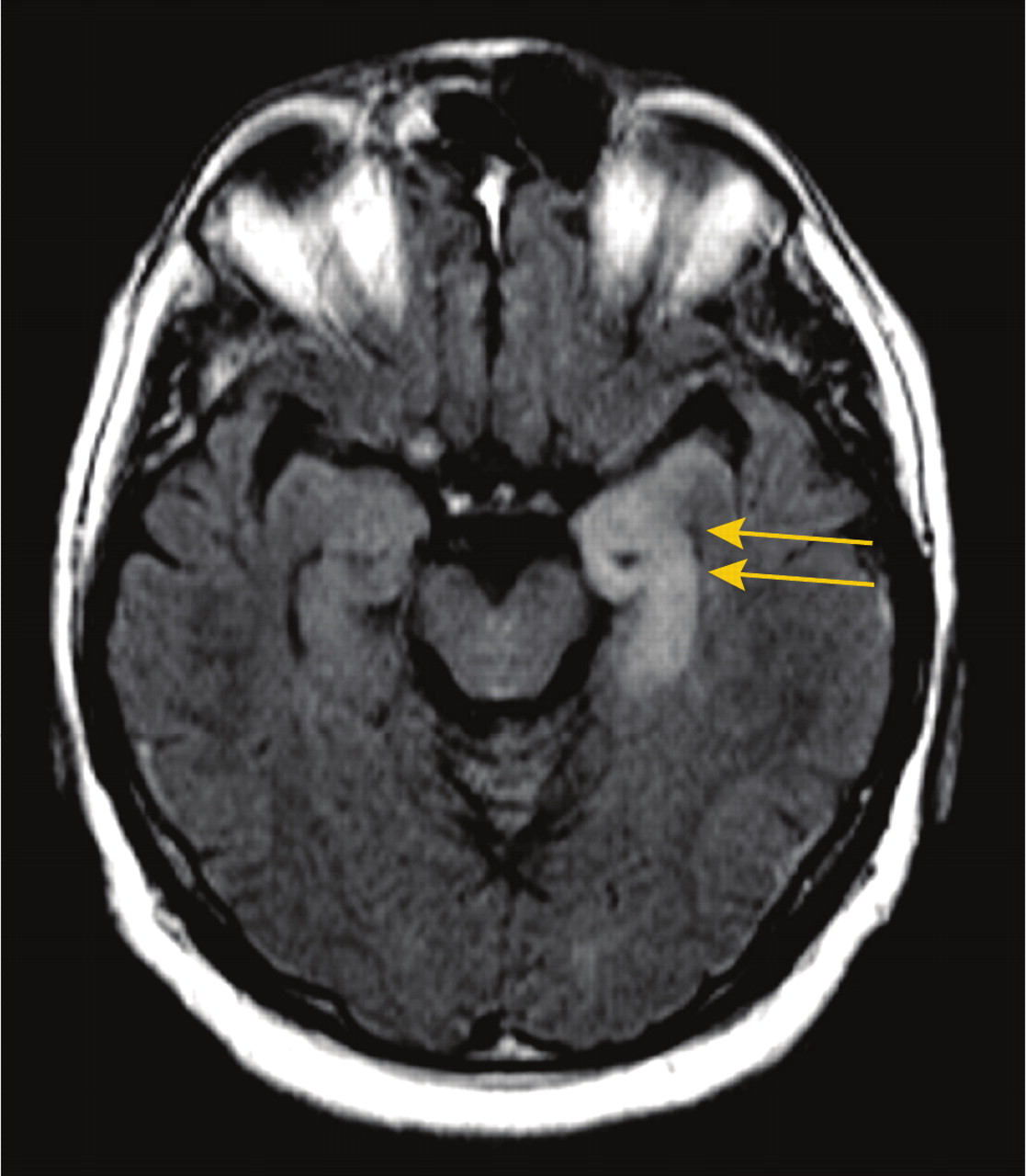
In many ways, the anti-NMDA receptor encephalitis is unique from the other syndromes discussed in this review. Rather than having predominant symptoms of memory changes or disorientation, patients are typically young women (75%) or children (40% younger than 18 years) with prominent psychiatric symptoms, including anxiety and agitation, bizarre behavior, delusional and/or paranoid thoughts, and visual or auditory hallucinations (see clinical vignettes) (
7,
61,
62). Recent work has focused specifically on the presentation of anti-NMDA receptor encephalitis in the pediatric population (as young as 23 months old), finding initial symptoms such as temper tantrums, behavioral change, agitation, aggression, and progressive speech deterioration (
61). The vast majority of patients in both the adult and pediatric populations experience a viral prodrome-like illness in the weeks prior to psychiatric destabilization. Throughout the first few weeks following admission, patients rapidly deteriorate neurologically with seizures and decreased consciousness, progressing to a catatonic-like state, along with dyskinesias, autonomic instability, and hypoventilation requiring intubation in some patients (more commonly adults) (
7,
61). While CSF findings are typical of encephalitis, MRI findings are unreliable, with approximately one-half of patients showing no abnormalities and only about 15% with specific signals in the medial temporal lobes (
7).
Initially, the NMDA receptor autoantibody syndrome was thought to be specifically associated with ovarian teratomas (
63). Studies now indicate that approximately 50% of patients do not have an identifiable tumor, and this percentage increases to nearly 70% when only those 18 or younger are considered (
7,
61). In patients with neoplasms, nearly all develop psychiatric or neurological symptoms prior to tumor diagnosis (
7). Although it is somewhat surprising given the severity of symptoms, patients with anti-NMDA receptor encephalitis often recover with treatment. Following tumor resection (if possible) and immunotherapy, nearly half of patients make a full recovery. In two large series, 75% had full or substantial recovery, although those remaining were left with severe deficits or died as a result of neurological complications (
7,
61). The presence of a tumor is a positive prognostic factor in this syndrome, as patients with tumor removal within 4 months of neuropsychiatric changes fared better than all other patients (
7).
The posthospitalization course in this patient population merits specific discussion. Of patients that ultimately make a full recovery or are left with only mild deficits, most (85%) have significant psychiatric abnormalities at discharge, including poor attention and planning, impulsivity, and behavioral disinhibition; approximately 25% experience sleep dysfunction (
7). Recovery is often slow, and it takes many months for patients to return to their baseline behavioral and cognitive status. In addition, 15 out of 100 patients had instances of relapse of encephalitis in one study, and most experienced a persistent amnesia for the entire illness (
7). The clinical picture and scientific results in this syndrome suggest that the antibody itself is pathogenic, as antibody titers correlate with disease severity (
63) and antibody activity results in a reversible decrease in synaptic NMDA receptors (
7). In addition, many drugs that modulate NMDA receptors are known to cause a similar constellation of symptoms, such as psychotic behavior (
64), dystonia (
65), and autonomic dysfunction (
66), while over the past several decades NMDA receptor hypofunction has received increasing scrutiny as a putative mechanism of schizophrenia (
67).
Anti-AMPA Receptor Antibodies
A recently discovered paraneoplastic disorder associated with limbic encephalitis is characterized by antibodies against subunits of the AMPA-type glutamate receptor (
20). The AMPA receptor mediates the majority of fast glutamatergic neurotransmission in the brain and plays a role in molecular mechanisms of learning and memory (
68). In this syndrome, subunits GluR1 and GluR2 are specifically targeted, resulting in the internalization and redistribution of AMPA receptors away from the synapse; the effect is reversible upon removal of antibody-containing CSF from neurons (
20). Animal models with similar mistrafficking of AMPA receptors have abnormalities in behavioral paradigms of learning and memory, as well as emotional disturbances (
69).
Of the 10 described patients with anti-AMPA receptor limbic encephalitis, nine were women, and the median age was 60 years. Almost all had isolated limbic symptoms: subacute memory loss (less than 8 weeks) and confusion (
20). The other most common symptom was agitation and/or aggressive behavior, which was reported in one-half of the patients (another had “behavioral changes” not otherwise specified [70]). Seven of the 10 patients had an associated tumor of the breast or lung or thymoma. All living patients with an identified neoplasm received cancer treatment, and nine patients received immunotherapy. Every patient receiving immunotherapy responded well, with reduced cognitive and behavioral symptoms (
20).
One of the most striking features of anti-AMPA receptor limbic encephalitis is the tendency to relapse despite treatment. Seven patients in the preceding series experienced relapsing symptoms, with deficits of short-term memory and persistent behavioral problems, such as aggression, in all but one patient, who had mild persistent depression and apathy (
20). All relapse cases occurred in the absence of tumor or tumor recurrence, suggesting that a persistent autoimmune disorder had been triggered. Taken together, these results demonstrate a remarkable similarity between the clinical picture and the behavior one would predict on the basis of AMPA receptor function in animal models.