[Case Study]
In August 2008, a resident at a Florida assisted living facility for adults with mental illness was diagnosed with infectious pulmonary tuberculosis (TB). From October 2008 to May 2009, 14 additional residents and three nonresidents were diagnosed with TB. The index patient was contagious for approximately 8 months before he was diagnosed in August 2008. He first sought medical attention for a cough and general malaise in April 2008, at a local psychiatric hospital where he felt comfortable receiving care because of his frequent previous hospitalizations there. He was evaluated by an internist and admitted for acute psychiatric decompensation for 8 days to a locked ward that held approximately 25 patients. Although cough was documented on admission, medical records did not reveal any detail on how the patient described his symptoms, and further evaluation was not performed at that time. During the course of his infectious period, the patient did not seek treatment at a medical facility for his worsening TB symptoms. He was held for one night in a one-person cell at the county jail and was hospitalized three more times at the psychiatric hospital for stays ranging from 2 to 8 days. He was assessed by an internist at each admission, and a cough was documented in each admission note. When the patient was hospitalized for the fourth time at the psychiatric facility in August 2008, a provider noted that his cough had persisted and ordered chest radiography, which revealed evidence of a cavitary lesion suggestive of pulmonary TB. The patient was transferred to a medical hospital, where sputum smear microscopy was positive for acid-fast bacilli, and confirmatory testing revealed Mycobacterium tuberculosis. After 2 weeks of TB treatment, the patient left against medical advice and returned to the assisted living facility. Three days later, supervisors from the assisted living facility brought him to another medical hospital for admission under direct one-to-one observation. He attempted to leave the hospital multiple times, requiring transfer to an isolation unit at the local jail and then to the A.G. Holley State Hospital, a Department of Health facility specializing in tuberculosis, in accordance with Florida state law permitting the involuntary examination and treatment of persons with mental illness who may be a harm to others, such as patients who have dangerous infectious diseases like tuberculosis.
The assisted living facility had an average census of 84 residents each month and the capacity to hold up to 91 at any one time. Each month, approximately four to five residents departed and a similar number of new residents arrived. Residents slept three or four to a room, but they did not have a curfew and were not required to sleep at the facility. Hence, despite stable housing, residents were sometimes transient, often sleeping at locations outside of the facility. The facility did not provide medical care; residents were not routinely screened for TB on admission, and those who developed TB symptoms could not be evaluated on-site. Medications were disbursed by facility staff, but staff did not enforce adherence.
[Introduction]
Although the incidence of tuberculosis (TB) in the United States has decreased steadily over the past decade, certain populations are at increased risk for
Mycobacterium tuberculosis infection and transmission, including persons with reported homelessness (
1), incarceration (
2), HIV infection (
3), or substance abuse (
4). TB outbreaks in some of these high-risk groups have been challenging and resource intensive for TB control programs (
5–
7). Whether mental illness is also a risk factor for TB remains to be documented.
An estimated 2.6%–5.7% of U.S. adults have a serious mental illness (
8,
9), and TB risk factors such as poverty (
10), substance use (
11), and HIV infection (
11) are known to be prevalent in this population. With the advent of effective antipsychotic medications in the 1950s, mental health care has shifted from large, state-run facilities to community institutions, displacing persons with mental illness to other congregate settings, such as homeless shelters, detention centers, nursing homes, and assisted living facilities (
12–
14). Such settings might lack routine TB infection control practices and be densely populated by persons with multiple risk factors for TB infection, creating environments with an increased likelihood of
M. tuberculosis transmission and placing persons with mental illness at further risk of infection.
We report here on the investigation, conducted from August 2008 to July 2009, of a TB outbreak involving an assisted living facility for adults with mental illness. We describe the risk for M. tuberculosis infection and the efficient transmission that occurred among persons with mental illness and highlight the challenges of TB control in this population.
Investigation of the Outbreak
Of the 18 patients diagnosed with TB disease, 11 cases were confirmed by sputum culture growth of
M. tuberculosis. Nine of these 11 cases had uncontaminated culture isolates available for genotyping analysis, which was conducted by spoligotyping and 12-locus mycobacterial interspersed repetitive unit (MIRU) typing; all
M. tuberculosis isolates had matching patterns. Florida law requires clinicians and laboratories to report TB cases to local health departments. Through the Centers for Disease Control and Prevention (CDC) National Tuberculosis Genotyping Service, health departments in the United States are able to submit for genotyping one
M. tuberculosis isolate from each culture-confirmed TB case within their jurisdiction (
15). As of July 2009, approximately 30% of Florida's culture-positive TB cases were being genotyped through the National Tuberculosis Genotyping Service, which limited knowledge about the prevalence of the outbreak-related
M. tuberculosis strain in the community. Because 15 of 18 patients had resided at the same assisted living facility, investigative efforts focused on this facility.
Case Definition
An outbreak case was defined as laboratory-confirmed TB disease caused by an M. tuberculosis strain with the outbreak-associated genotype pattern, or any TB disease without specimens available for genotyping, diagnosed between January 1, 2008, and June 30, 2009, in a county resident who had been an employee, resident, or volunteer at the assisted living facility or a contact of one these persons, for any time since January 1, 2007. Clinical cases were similarly defined but lacked laboratory confirmation and were instead determined to be TB disease by a clinician on the basis of symptoms, physical findings, and radiologic evidence.
Case Reviews
To determine the demographic and clinical characteristics of outbreak patients, establish epidemiologic links among them, and identify potential transmission sites, we reviewed medical records at hospitals, clinics, and the health department and interviewed patients and their proxies. Friends, relatives, employees from the assisted living facility, and health care providers served as proxies for patients who were either unavailable or unable to provide information because of severe mental illness. The period of time that each patient was considered contagious (“infectious period”) was estimated according to the CDC's contact investigation guidelines (
16).
Contact Investigations
Owing to difficulties eliciting names of contacts from the outbreak patients with mental illness, we identified places that they frequented or were thought to have visited during their infectious period. Based on this information, we reviewed registries and admitting information of homeless shelters, hospitals (including two mental health facilities), and county detention centers to document evidence of TB transmission at these sites.
In response to the index patient's pulmonary TB diagnosis and the cases that were subsequently identified, contact investigations had been conducted from August 2008 to July 2009 at the county jail and two sites most concerning for transmission: the assisted living facility and a nearby psychiatric hospital where the index patient had been hospitalized multiple times while contagious. To determine the scope of transmission of the outbreak strain, investigators reviewed the outcomes of the contact investigations at these sites, including the prevalence of latent TB infection and the incidence of active TB disease among contacts. All identified contacts of any patient with cavitary or sputum smear-positive pulmonary disease had been offered TB screening (
16). The evaluation included a review of symptoms and testing for TB infection with the tuberculin skin test (TST) (
17). An induration ≥5 mm was considered positive, indicative of TB infection (
16). Contacts who had symptoms suggestive of TB or had positive TST results underwent further clinical evaluation, such as chest radiography or sputum microscopy, to exclude TB disease.
Location-Based Active Case-Finding
Residents and staff at the assisted living facility were repeatedly exposed to infectious TB through outbreak patients who remained contagious either because their TB disease went unrecognized and untreated or because nonadherence rendered their TB treatment ineffective. Therefore, in July 2009, the Duval County Health Department rescreened all persons for TB on-site at the facility. Residents and staff were evaluated for TB symptoms using a standardized questionnaire, and all were offered testing for HIV infection (
16). Those with a previous negative or unknown TST result were given a TST. Sputum was collected for microscopy and culture, and portable chest radiography was performed on all persons not already being managed by the local health department for TB disease or latent TB infection. Persons whose chest radiographs were suggestive of TB disease were referred to a nearby hospital for further clinical evaluation and management.
Epidemiologic Links and Case Characteristics
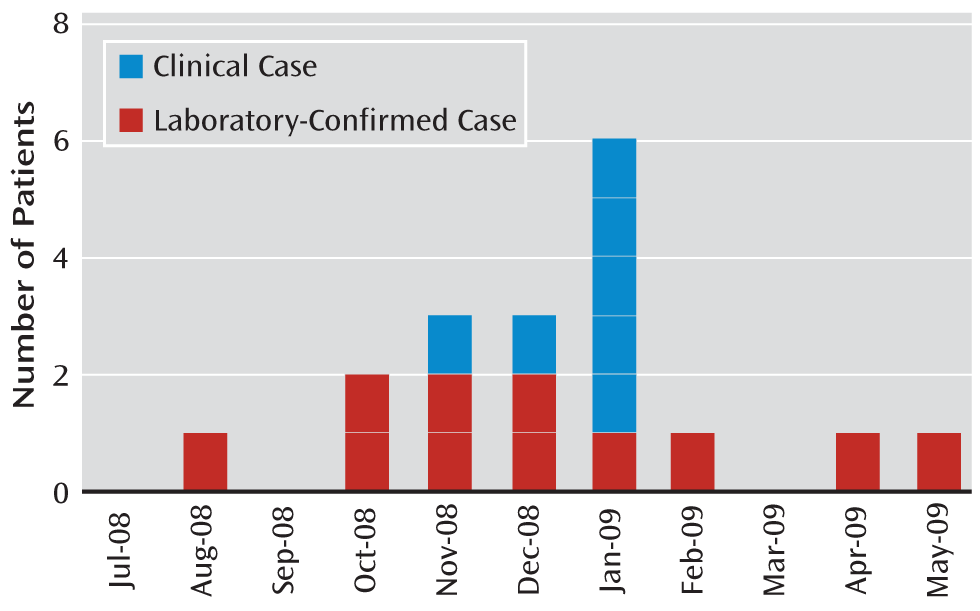
Of the 18 patients with TB disease who met the case definition (
Figure 1), 15 had resided at the assisted living facility during the time that the index patient was present and contagious and three were nonresidents. Of these three, one had close social ties with residents from the facility and two (a nurse and a patient) were exposed to TB through contact with the index patient at the psychiatric hospital where he had multiple admissions while contagious.
Severe and persistent mental illness was common among patients in this TB outbreak; all but two were documented to have schizophrenia spectrum disorders (
Table 1). Ten patients (56%) did not report TB symptoms or seek medical care independently, and their TB was instead diagnosed as a consequence of the health department's outreach (i.e., TB contact investigations). The median infectious period was 133 days, with a range of 45–307 days. Nonadherence with TB treatment was documented in the medical record for nine patients (50%), all of whom had schizophrenia. Five patients (28%) were committed by court order to the A.G. Holley State Hospital, a Department of Health facility specializing in tuberculosis. Two patients (11%) died from TB during the hospitalizations when their TB disease was diagnosed. Of nine patients for whom HIV test results were available, two (22%) tested positive for infection.
Based on review of medical records for the 18 patients, two patients were reported to be homeless, five had excessive alcohol use (including three who were also documented as users of illicit substances), and 17 smoked tobacco in the year preceding diagnosis. No patients were documented in the medical records to have been incarcerated. Staff and patient interviews, however, identified four additional patients who left the facility for extended periods, during which they lived on the streets or in homeless shelters, and four additional patients who used illicit drugs and consumed alcohol excessively. On review of county jail records, we found that eight patients (44%) had been detained in the county jail at least once since January 2007.
Contact Investigation Findings
We identified four sites where outbreak patients had spent time during their infectious periods: the assisted living facility, the psychiatric hospital where the index patient had repeatedly been hospitalized, the county jail, and another psychiatric hospital where two other patients received psychiatric care.
Outcomes of contact investigations at the assisted living facility and the psychiatric hospital where the index patient was repeatedly hospitalized are summarized in
Table 2. Fifty-five percent of contacts at these two facilities combined had evidence of TB infection. At the assisted living facility before the July 2009 active case-finding activity, 75 (68%) of 134 exposed residents had been evaluated. Of these, 66 (88%) had a TST reaction ≥5 mm, including three residents with prior TST results of 0 mm, suggesting recent infection in these three persons. Among 14 of 15 staff who were evaluated, seven (50%) had a positive TST result, three of whom were previously positive and four of whom had a 0-mm TST result within the previous 2 years but whose TST results during the contact investigations ranged from 13 to 19 mm (i.e., TST conversion) (
Table 2). In contrast, no TST conversions were documented among 11 staff who had been evaluated for TB as part of an annual employee TB screening in 2007; at that time, three of the 11 (27%) had a previous positive TST (exact measurements unknown) and eight had a negative TST result.
At the psychiatric hospital, 23 (14%) of the 166 patient contacts were located and evaluated. The remainder did not respond to letters informing them of a TB exposure or did not have recorded addresses. Of 23 evaluated contacts, 11 (48%) had a positive TST, although none had baseline test results for comparison, limiting the ability to identify recent infections. Of 78 staff contacts at the psychiatric hospital, 74 (95%) were evaluated. Of these, seven (10%) were known to have previous positive TST results, and 11 (15%) who had negative baseline results in 2007 had a TST reaction ≥5 mm. The remaining 56 had negative TST results.
Contact investigations at the county jail identified two persons who had close contact with an infectious case. Both individuals were evaluated and had negative TST results. Contact investigations performed at the other psychiatric hospital identified 115 possible contacts, none of whom could be located and evaluated.
Outcome of Location-Based Active Case-Finding
During active case-finding on-site at the assisted living facility in July 2009, 69 persons were screened for TB, including four staff and 65 residents (
Table 3). Sixty-five participants had been screened previously but had been reexposed since their last screening. Four residents were referred to a nearby hospital for further clinical evaluation because of an abnormal chest X-ray and a previous positive TST; however, no additional TB cases were found.
Discussion
We describe a large TB outbreak of 18 cases associated with an assisted living facility for adults with mental illness. Of 18 outbreak patients, 16 had a schizophrenia spectrum disorder and 17 had known TB risk factors, such as a recent history of incarceration (
2), substance use (
4), homelessness (
1), and smoking (
18). Evaluation of 75 residents exposed to TB at the assisted living facility from August 29, 2008 (when the index patient was diagnosed), through July 6, 2009, showed that 66 (88%) were infected with
M. tuberculosis, an extraordinarily high proportion. By comparison, the prevalence of latent TB infection among reported contacts of pulmonary TB patients with positive sputum smears in the United States has been estimated at 20%–30% (
19). These data, combined with the magnitude of the outbreak, suggest an elevated risk for TB infection among adults with mental illness and a risk for sustained transmission when they inhabit crowded congregate settings.
To our knowledge, this is the first report to demonstrate the vulnerability of persons with mental illness to TB outbreaks. While a few small studies, conducted as general surveys and not as part of an outbreak investigation, have previously demonstrated an elevated prevalence of TB infection among adults with mental illness (range, 17%–36%) (
20–
22), none have described the occurrence of TB outbreaks and risks of TB transmission in this population.
One of the major contributing factors of this outbreak was delayed diagnosis, evidenced by a median infectious period of 133 days among outbreak patients. The index patient, whose TB was infectious for approximately 8 months, continued to reside at the assisted living facility and was admitted to a psychiatric facility four times during his infectious period. As a result, a chain of TB transmission was initiated at the assisted living facility, where 14 additional residents were subsequently diagnosed with TB. In addition, the index patient served as the likely TB source for another patient and a health care provider at the psychiatric facility where he was repeatedly hospitalized.
Because persons with mental illness often exhibit low health care-seeking behavior, which may derive from an inability to recognize their own health problems or a general distrust of the health care system (
23–
25), they may be especially prone to delays in diagnosis—a factor that has contributed to previous TB outbreaks (
6,
7,
26). A lack of clarity about who is responsible for the medical care of patients with mental illness and the possibility of impaired communication between such patients and their health care providers about risk factors and symptoms further increase the chances of diagnostic delays (
24,
25). In this outbreak, more than half of the patients did not report for medical evaluation but instead were diagnosed with TB as a result of the health department's contact investigations. Two patients, neither infected with HIV, died from TB shortly after their TB diagnosis was made, indicating late-stage disease. The underdocumentation of TB risk factors in patients' medical charts supports the hypothesis that once patients with severe mental illness do seek care for TB symptoms, risk factors are often not elicited, not reliably communicated, or not recorded. Maintaining a high level of suspicion about TB risk factors in patients with mental illness and systematically inquiring about these factors could help providers avoid diagnostic delays.
In addition to delayed diagnosis, treatment nonadherence among patients contributed to this outbreak. Nonadherence to medication can prolong the infectious period, during which time
M. tuberculosis can continue to spread or lead to the emergence of drug-resistant TB strains. Nine patients had trouble adhering to prescribed treatment, and five of them required involuntary hospital admission to ensure completion of treatment. Poor insight, aversion to side effects, and poor alliance with treating clinicians are cited as reasons for low adherence to prescribed medication among persons with mental illness (
27) and pose substantial challenges to TB control efforts. Recognizing and addressing these challenges early in the course of treatment could limit TB transmission and morbidity.
TB contact investigations remained incomplete for this outbreak because patients' mental illness made it difficult for investigators to elicit names of persons who were exposed to the patients and to sites where the patients visited or stayed while contagious. Even when names of contacts were known, resource constraints and characteristics of the population, such as substance use and homelessness, limited the ability of public health officials to locate, detect, and treat individuals for active TB disease or latent TB infection. Slightly less than half of the identified contacts of TB cases from the two main transmission sites (the assisted living facility and the psychiatric hospital) were evaluated. Among persons with untreated infection, about 10% will develop TB disease, approximately half doing so in the first 1–2 years after exposure (
16). Contacts who are not found and evaluated therefore represent missed opportunities for prevention of TB disease and transmission.
This investigation had several limitations. Because not all TB cases in Florida had been genotyped at the time of this outbreak, additional cases linked to the outbreak could have been missed, preventing appreciation of the full scope of the outbreak. Difficulties in locating contacts limited our ability to identify additional cases, which may also have resulted in an underestimate of the outbreak's magnitude. Finally, we did not have data on baseline TST results for most of the contacts, which hindered our ability to draw conclusions about the timing of infection for contacts found to have M. tuberculosis infection (i.e., a positive TST). Nonetheless, the magnitude of this outbreak among adults with mental illness, the frequency of TB risk factors among patients, and the similarity of the outbreak settings to other environments where adults with mental illness reside and receive treatment suggest an elevated risk for TB transmission among adults with mental illness.
Despite often having many risk factors for TB, adults with severe mental illness are not widely recognized to have an elevated risk of TB infection. Additional research on the risk of TB in this population would help in the shaping of education messages to clinicians about this risk. To more effectively contain the spread of TB among persons with mental illness, earlier diagnosis of disease is essential, and clinicians caring for such patients should maintain a low threshold for suspecting TB disease, especially among those living in congregate settings. Interrupting disease transmission as early as possible will also require resources to provide alternative housing until TB patients residing in congregate settings have completed enough treatment to render them noncontagious as well as resources to carry out contact investigations in this challenging and often transient population. Finally, because health departments need to act quickly when problems with TB treatment adherence arise, assessing all patients with mental illness for the potential of treatment nonadherence at the time of diagnosis could help TB programs anticipate and prepare for some of these problems.