A Randomized Controlled Trial of 7-Day Intensive and Standard Weekly Cognitive Therapy for PTSD and Emotion-Focused Supportive Therapy
Abstract
Objective
Method
Results
Conclusions
Method
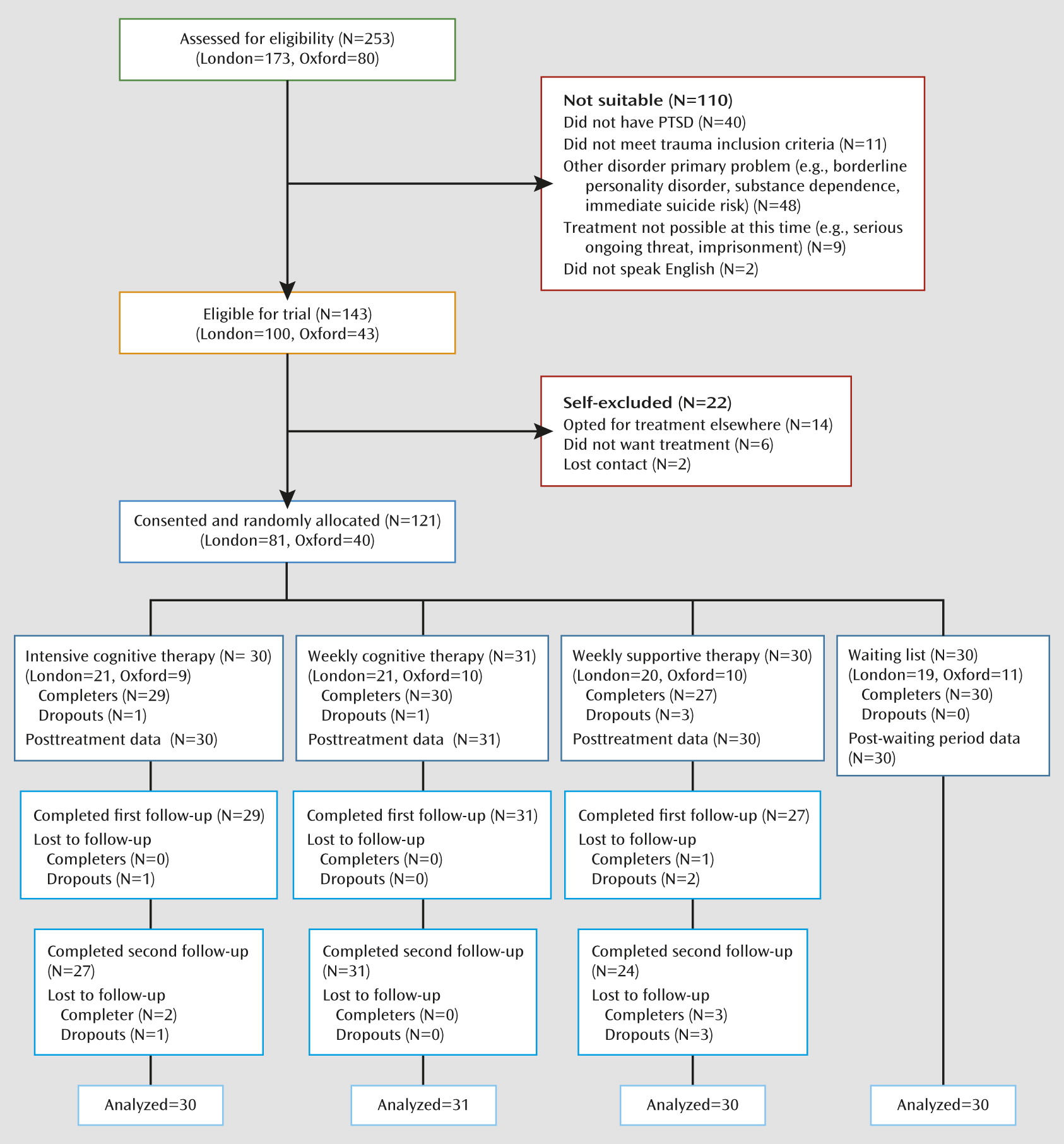
Participants
| Characteristics | Intensive Cognitive Therapy (N=30) | Standard Weekly Cognitive Therapy (N=31) | Supportive Therapy (N=30) | Waiting List (N=30) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 39.7 | 12.4 | 41.5 | 11.7 | 37.8 | 9.9 | 36.8 | 10.5 |
| N | % | N | % | N | % | N | % | |
| Sex | ||||||||
| Female | 18 | 60.0 | 18 | 58.1 | 17 | 56.7 | 18 | 60.0 |
| Male | 12 | 40.0 | 13 | 43.9 | 13 | 43.4 | 12 | 40.0 |
| Ethnic group | ||||||||
| Caucasian | 22 | 73.3 | 20 | 64.5 | 22 | 73.3 | 21 | 70.0 |
| Ethnic minority | 8 | 26.7 | 11 | 35.5 | 8 | 26.7 | 9 | 30.0 |
| Marital status | ||||||||
| Never married | 9 | 30.0 | 10 | 32.3 | 12 | 40.0 | 10 | 33.3 |
| Divorced/separated/widowed | 3 | 10.0 | 4 | 12.9 | 4 | 13.4 | 5 | 16.7 |
| Married/cohabitating | 18 | 60.0 | 17 | 54.8 | 14 | 46.7 | 15 | 50.0 |
| Education | ||||||||
| College/university | 6 | 20.0 | 8 | 25.8 | 8 | 26.7 | 10 | 33.3 |
| High school examination (age 18) | 1 | 3.3 | 6 | 19.4 | 6 | 20.0 | 6 | 20.0 |
| Standard school examination (age 16) | 18 | 60.0 | 12 | 38.7 | 12 | 40.0 | 13 | 43.3 |
| None | 5 | 16.7 | 5 | 16.1 | 4 | 13.3 | 1 | 3.3 |
| Current employment | ||||||||
| Unemployed | 7 | 23.3 | 7 | 22.6 | 9 | 30.0 | 5 | 16.7 |
| On disability/retired | 2 | 6.7 | 3 | 9.7 | 3 | 10.0 | 3 | 10.0 |
| Sick leave | 7 | 23.3 | 3 | 9.7 | 5 | 16.7 | 4 | 13.3 |
| Working full- or part-time | 14 | 46.7 | 18 | 58.1 | 13 | 43.3 | 18 | 60.0 |
| Profession | ||||||||
| Professional | 5 | 17.2 | 4 | 12.9 | 6 | 20.0 | 6 | 20.7 |
| White collar | 8 | 27.6 | 17 | 54.8 | 7 | 23.3 | 12 | 41.4 |
| Blue collar | 10 | 34.5 | 6 | 19.4 | 10 | 33.3 | 6 | 20.7 |
| Homemaker/student/not working | 6 | 20.6 | 4 | 12.9 | 7 | 23.3 | 5 | 17.2 |
| Traumas | ||||||||
| Type of main traumatic event | ||||||||
| Interpersonal violence | 12 | 40.0 | 12 | 38.7 | 11 | 36.7 | 10 | 33.3 |
| Accidents/disaster | 11 | 36.7 | 11 | 35.5 | 14 | 46.7 | 10 | 33.3 |
| Death/harm to others | 2 | 6.7 | 1 | 3.2 | 2 | 6.7 | 4 | 13.3 |
| Other | 5 | 16.7 | 7 | 22.6 | 3 | 10.0 | 6 | 20.0 |
| Time since main traumatic event | ||||||||
| 3 months – 1 year | 10 | 33.3 | 14 | 45.2 | 8 | 27.8 | 14 | 46.7 |
| 1–2 years | 10 | 33.3 | 5 | 16.1 | 7 | 24.1 | 6 | 20.0 |
| 2–4 years | 7 | 23.3 | 11 | 35.5 | 8 | 27.6 | 3 | 10.0 |
| >4 years | 3 | 10.0 | 1 | 3.2 | 6 | 20.7 | 7 | 23.3 |
| History of other trauma | ||||||||
| Yes | 22 | 63.3 | 21 | 67.7 | 23 | 76.7 | 20 | 66.7 |
| No | 8 | 26.7 | 10 | 32.3 | 7 | 23.3 | 10 | 33.3 |
| Reported history of childhood abuse | ||||||||
| Yes | 5 | 16.7 | 2 | 6.5 | 4 | 13.3 | 3 | 10.0 |
| No | 25 | 83.3 | 29 | 93.5 | 26 | 86.7 | 27 | 90.0 |
| Comorbidity | ||||||||
| Anxiety disorder | ||||||||
| Yes | 10 | 33.3 | 7 | 22.6 | 10 | 33.3 | 10 | 33.3 |
| No | 20 | 66.7 | 24 | 77.4 | 20 | 66.7 | 20 | 66.7 |
| Depressive disorder | ||||||||
| Yes | 12 | 40.0 | 7 | 22.6 | 11 | 36.7 | 14 | 46.7 |
| No | 18 | 60.0 | 24 | 77.4 | 19 | 63.3 | 16 | 53.3 |
| Substance abuse | ||||||||
| Yes | 6 | 20.0 | 6 | 19.4 | 6 | 20.0 | 2 | 6.7 |
| No | 24 | 80.0 | 25 | 80.6 | 24 | 80.0 | 28 | 93.3 |
| History of substance dependence | ||||||||
| Yes | 2 | 6.7 | 4 | 12.9 | 2 | 6.7 | 1 | 3.3 |
| No | 28 | 93.3 | 27 | 87.1 | 28 | 93.3 | 29 | 96.7 |
| Axis II disorder | ||||||||
| Yes | 7 | 23.3 | 5 | 16.1 | 4 | 13.3 | 8 | 26.7 |
| No | 23 | 76.7 | 26 | 83.9 | 26 | 86.7 | 22 | 73.3 |
| Treatment history | ||||||||
| Previous treatment for PTSD | ||||||||
| Yes | 10 | 33.3 | 11 | 35.5 | 12 | 40.0 | 11 | 36.7 |
| No | 20 | 66.7 | 20 | 64.5 | 18 | 60.0 | 19 | 63.3 |
| Psychotropic medication pretreatment | ||||||||
| Yes | 5 | 16.7 | 11 | 35.5 | 12 | 40.0 | 8 | 26.7 |
| No | 25 | 83.3 | 20 | 64.5 | 18 | 60.0 | 22 | 73.3 |
| Changes in medication | ||||||||
| Discontinued before 14 weeks | 1 | 20.0 | 5 | 45.5 | 3 | 25.0 | 2 | 25 |
| in follow-up | 1 | 20.0 | 1 | 9.1 | 3 | 25.0 | – | – |
| Stayed on medication | 3 | 60.0 | 5 | 45.5 | 6 | 50.0 | 6 | 75 |
| Started medication during study | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other psychological treatment during study | ||||||||
| Trauma-related | 0 | 0 | 0 | 0 | 1 | 3.3 | 0 | 0 |
| For other problems | 0 | 0 | 1 | 3.2 | 0 | 0 | 0 | 0 |
| Treatment received in trial | Mean | SD | Mean | SD | Mean | SD | ||
| Number of sessions | ||||||||
| Before 14 weeks | 10.13 | 2.18 | 10.10 | 3.26 | 10.27 | 3.21 | ||
| Booster | 1.90 | 0.80 | 2.07 | 1.46 | 2.20 | 1.32 | ||
| Treatment credibility | 23.63 | 4.40 | 24.29 | 4.60 | 22.00 | 5.12 | ||
| Therapeutic alliance | ||||||||
| Patient rating | 5.94 | 0.56 | 5.70 | 0.68 | 5.53 | 0.51 | ||
| Therapist rating | 5.69 | 0.47 | 5.74 | 0.40 | 5.67 | 0.48 | ||
Random Allocation and Masking
Treatment Conditions
Standard cognitive therapy for PTSD.
Seven-day intensive cognitive therapy for PTSD.
Emotion-focused supportive therapy.
Waiting list.
Outcome Measures
Primary Outcome Measures
Clinician-rated PTSD symptoms.
Severity of PTSD symptoms.
Secondary Outcome Measures
Disability.
General anxiety and depression.
Quality of life.
Therapist Training and Treatment Fidelity
Data Analysis
Results
Adverse Effects, Dropouts, and Symptom Deterioration
| 1: Intensive Cognitive Therapy (N=30) | 2: Standard Cognitive Therapy (N=31) | 3: Supportive Therapy (N=30) | 4: Waiting List (N=30) | Analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variablea | N | % | N | % | N | % | N | % | χ2 | df | Significant Contrasts |
| Dropouts | 1 | 3.3 | 1 | 3.2 | 3 | 10 | 0 | 0 | 0.26 | 3, 121 | |
| Symptom deterioration | |||||||||||
| Self-reports (PDS) | 0 | 0 | 0 | 0.0 | 1 | 3.3 | 0 | 0.0 | 3.06 | 3, 121 | |
| Assessor-rated (CAPS) | 0 | 0 | 1 | 3.2 | 3 | 10.0 | 6 | 20.0 | 9.31* | 3, 121 | 1, 2<4 |
| Loss of diagnosis (CAPS) | |||||||||||
| Posttreatment/wait (14 weeks) | 22 | 73.3 | 24 | 77.4 | 13 | 43.3 | 2 | 6.7 | 38.92*** | 3, 121 | 1, 2>3 > 4 |
| Follow-up 1 (27 weeks) | 22 | 73.3 | 23 | 74.2 | 11 | 36.7 | N/A | 11.70** | 2, 91 | 1, 2>3 | |
| Follow-up 2 (40 weeks) | 20 | 66.7 | 23 | 74.2 | 12 | 40.0 | N/A | 8.18* | 2, 91 | 1, 2>3 | |
| Total remission (assessor-rated, CAPS) | |||||||||||
| Posttreatment or wait (14 weeks) | 14 | 46.7 | 16 | 51.6 | 6 | 20.0 | 1 | 3.3 | 22.19*** | 3, 121 | 1, 2>3>4 |
| Follow-up 1 (27 weeks) | 12 | 40.0 | 21 | 67.7 | 5 | 16.7 | N/A | 16.41*** | 2, 91 | 1, 2>3 | |
| Follow-up 2 (40 weeks) | 16 | 53.3 | 23 | 74.2 | 8 | 26.7 | N/A | 13.84** | 2, 91 | 1, 2>3 | |
| Total remission (self-report, PDS) | |||||||||||
| Posttreatment or wait (14 weeks) | 17 | 56.7 | 20 | 64.5 | 9 | 30.0 | 1 | 3.3 | 29.53*** | 3, 121 | 1, 2>3>4 |
| Follow-up 1 (27 weeks) | 15 | 50.0 | 22 | 71.0 | 7 | 23.3 | N/A | 13.90** | 2, 91 | 1, 2>3 | |
| Follow-up 2 (40 weeks) | 17 | 56.7 | 18 | 58.1 | 9 | 30.0 | N/A | 6.05* | 2, 91 | 1, 2>3 | |
Comparison of Treatment Conditions With Waiting List Condition
| Measurea | Intensive Cognitive Therapy (N=30) | Standard Cognitive Therapy (N=31) | Supportive Therapy (N=30) | Waiting List (N=30) | ||||
|---|---|---|---|---|---|---|---|---|
| Primary outcomes | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Independent assessor (CAPS) | ||||||||
| Baseline | 78.72 | 19.80 | 70.60 | 13.45 | 74.60 | 15.39 | 69.95 | 14.17 |
| 14 weeks (posttreatment) | 32.22 | 27.20 | 26.97 | 28.68 | 47.88 | 31.77 | 65.28 | 20.64 |
| 27 weeks (follow-up 1) | 35.56 | 26.26 | 20.86 | 25.23 | 49.32 | 32.46 | ||
| 40 weeks (follow-up 2) | 35.33 | 35.11 | 20.96 | 27.71 | 49.04 | 38.01 | ||
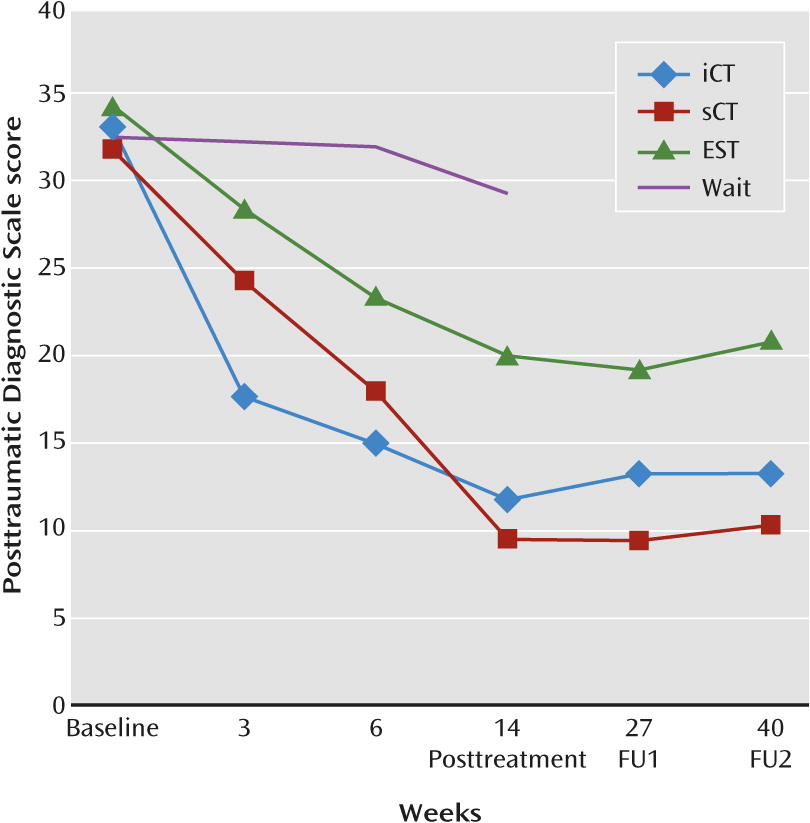
| Self-report (PDS) | ||||||||
| Baseline | 33.21 | 7.66 | 32.44 | 6.94 | 34.26 | 7.40 | 32.46 | 7.60 |
| 6 weeks | 14.85 | 8.92 | 16.33 | 11.58 | 23.30 | 12.90 | 31.92 | 6.84 |
| 14 weeks (posttreatment) | 11.98 | 9.60 | 9.39 | 10.88 | 19.98 | 13.67 | 29.24 | 9.36 |
| 27 weeks (follow-up 1) | 13.91 | 11.63 | 10.15 | 11.86 | 18.93 | 12.98 | ||
| 40 weeks (follow-up 2) | 13.03 | 13.99 | 9.63 | 11.26 | 20.94 | 15.40 | ||
| Secondary outcomes | ||||||||
| Disability (SDS) | ||||||||
| Baseline | 20.48 | 5.55 | 21.39 | 5.11 | 19.65 | 6.97 | 17.28 | 7.74 |
| 6 weeks | 10.72 | 7.51 | 14.02 | 9.35 | 16.60 | 7.90 | 17.22 | 6.67 |
| 14 weeks (posttreatment) | 9.30 | 8.20 | 10.02 | 9.76 | 14.28 | 9.09 | 17.20 | 6.38 |
| 27 weeks (follow-up 1) | 10.61 | 8.80 | 8.68 | 9.50 | 13.67 | 9.86 | ||
| 40 weeks (follow-up 2) | 9.72 | 9.22 | 9.37 | 10.07 | 14.47 | 11.35 | ||
| Anxiety (BAI) | ||||||||
| Baseline | 26.23 | 13.12 | 28.42 | 14.17 | 25.12 | 11.31 | 23.57 | 9.12 |
| 6 weeks | 13.55 | 12.16 | 13.88 | 14.01 | 17.01 | 13.30 | 23.26 | 10.88 |
| 14 weeks (posttreatment) | 11.57 | 11.94 | 9.24 | 12.09 | 16.35 | 14.56 | 22.13 | 10.59 |
| 27 weeks (follow-up 1) | 10.37 | 11.59 | 9.63 | 13.71 | 15.50 | 13.74 | ||
| 40 weeks (follow-up 2) | 11.85 | 13.35 | 9.00 | 12.61 | 15.99 | 16.15 | ||
| Depression (BDI) | ||||||||
| Baseline | 23.93 | 9.86 | 21.90 | 10.77 | 26.18 | 10.68 | 23.47 | 8.96 |
| 6 weeks | 14.34 | 9.30 | 13.39 | 10.70 | 19.79 | 12.42 | 21.26 | 8.06 |
| 14 weeks (posttreatment) | 12.10 | 9.97 | 11.07 | 11.80 | 17.00 | 12.82 | 20.85 | 10.02 |
| 27 weeks (follow-up 1) | 12.03 | 11.25 | 10.54 | 12.70 | 16.29 | 12.10 | ||
| 40 weeks (follow-up 2) | 12.84 | 12.54 | 9.44 | 12.18 | 18.60 | 14.05 | ||
| Quality of life | ||||||||
| Baseline | 36.93 | 12.84 | 39.36 | 21.87 | 38.78 | 18.40 | 45.68 | 20.98 |
| 6 weeks | 49.54 | 17.23 | 57.49 | 20.82 | 44.86 | 25.25 | 41.74 | 15.13 |
| 14 weeks (posttreatment) | 52.67 | 20.21 | 62.93 | 21.70 | 49.22 | 24.97 | 46.75 | 19.00 |
| 27 weeks (follow-up 1) | 58.10 | 22.78 | 60.43 | 23.31 | 49.61 | 25.67 | ||
| 40 weeks (follow-up 2) | 54.57 | 20.74 | 65.11 | 22.46 | 50.38 | 25.53 | ||
| Comparison and Measurea | Intensive Cognitive Therapy | Standard Weekly Cognitive Therapy | Supportive Therapy | Waiting List | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Within-group pre-post effect sizes | d | d | d | d | ||||||
| PTSD symptoms (CAPS) | 1.95 | 1.95 | 1.07 | 0.26 | ||||||
| PTSD symptoms (PDS) | 2.45 | 2.53 | 1.30 | 0.38 | ||||||
| Disability | 1.60 | 1.50 | 0.66 | 0.01 | ||||||
| Anxiety | 1.17 | 1.46 | 0.67 | 0.15 | ||||||
| Depression | 1.19 | 0.96 | 0.78 | 0.28 | ||||||
| Quality of life | 0.93 | 1.08 | 0.48 | 0.05 | ||||||
| Between-group effect sizes | Adjusted Difference | 95% CI | d | Adjusted Difference | 95% CI | d | Adjusted Difference | 95% CI | d | d |
| Waiting list and | ||||||||||
| PTSD symptoms (CAPS) | 39.55*** | 26.60–52.51 | 1.57 | 38.80*** | 26.19–51.40 | 1.55 | 20.84** | 8.06–33.61 | 0.84 | |
| PTSD symptoms (PDS) | 17.72*** | 12.54–22.90 | 1.75 | 19.84*** | 14.71–24.97 | 1.96 | 10.35*** | 5.15–15.54 | 1.02 | |
| Disability | 9.96*** | 6.10–13.81 | 1.33 | 9.82*** | 5.95–13.68 | 1.30 | 4.45* | 0.62–8.28 | 0.59 | |
| Anxiety | 11.98*** | 6.54–17.43 | 1.13 | 15.48*** | 10.04–20.91 | 1.45 | 6.61* | 1.18–12.05 | 0.62 | |
| Depression | 9.04*** | 4.26–13.81 | 0.97 | 8.81*** | 4.06–13.55 | 0.95 | 5.54* | 0.75–10.34 | 0.59 | |
| Quality of life | –12.43** | –21.28 to –3.58 | 0.73 | –20.67*** | –29.39 to –11.95 | 1.21 | –7.98 | –16.79 to 0.83 | 0.47 | |
| Supportive therapy and | ||||||||||
| PTSD symptoms (CAPS) | 18.72** | 5.96–31.45 | 0.75 | 17.96** | 5.31–30.62 | 0.72 | ||||
| PTSD symptoms (PDS) | 7.37** | 2.19–12.55 | 0.73 | 9.49*** | 4.34–14.64 | 0.94 | ||||
| Disability | 5.51** | 1.71–9.31 | 0.74 | 5.37** | 1.59–9.15 | 0.72 | ||||
| Anxiety | 5.37* | 0.06–10.80 | 0.51 | 8.86** | 3.46–14.27 | 0.83 | ||||
| Depression | 3.49 | –1.30 to 8.28 | 0.37 | 3.26 | –1.50 to 8.05 | 0.35 | ||||
| Quality of life | –4.45 | –13.17 to 4.28 | 0.26 | –12.69** | –21.33 to –4.04 | 0.74 | ||||
| Standard weekly cognitive therapy and | ||||||||||
| PTSD symptoms (CAPS) | 0.76 | –12.06 to 13.57 | 0.03 | |||||||
| PTSD symptoms (PDS) | –2.12 | –7.26 to 3.02 | 0.21 | |||||||
| Disability | 0.14 | –3.63 to 3.91 | 0.02 | |||||||
| Anxiety | –3.49 | –8.89 to 1.90 | 0.33 | |||||||
| Depression | 0.23 | –4.52 to 4.98 | 0.02 | |||||||
| Quality of life | 8.24 | –0.42 to 16.90 | 0.48 | |||||||
Comparison of Treatment Conditions
Speed of Recovery
Additional Comparison of Intensive and Standard Weekly Cognitive Therapy Including Waiting List Patients
Discussion
Footnotes
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

