The passage of the Affordable Care Act (ACA) accelerated the development and implementation of innovative models along the range of opportunities for integration, from improving treatment of mental health conditions in general medical settings to addressing the general medical conditions that lead to early mortality in populations with serious mental illnesses in mental health settings. Of major concern is that 60% of patients with a psychiatric diagnosis do not receive any form of treatment, and over half of those who do will get their care in a general medical setting. Unfortunately, in primary care settings, only 13% of the mental health care delivered is considered to be “minimally adequate” (
1). In addition, the presence of a psychiatric diagnosis can increase the overall costs of health care by two or three times, leading to the conclusion that significant cost savings within the health care system can be achieved by adequately addressing mental health and general medical conditions concurrently (
2). The shortage of a sufficient psychiatric workforce to address these needs, coupled with forces such as stigma that deter engagement in treatment, has led to the call for psychiatrists to work with other professions to develop new delivery models to provide effective care to the greatest number of people possible.
“Integrated behavioral health care” has been defined as follows by the Agency for Healthcare Research and Quality (
3):
The care a patient experiences as a result of a team of primary care and behavioral health clinicians, working together with patients and families, using a systematic and cost-effective approach to provide patient-centered care for a defined population.
The collaborative care model originated in the early work of Wayne Katon and colleagues at the University of Washington, who were looking for new ways to assist primary care providers in the diagnosis and treatment of mental disorders by providing psychiatric consultation in the primary care setting (
4). In the 1990s, Jürgen Unützer piloted the Improving Mood—Promoting Access to Collaborative Treatment (IMPACT) trial (
5), adding elements of the chronic care model (
6), including care managers and population-based tools, for the treatment of depression in adults age 60 and over. The IMPACT trial, the largest study of this model ever completed, demonstrated a 50% greater improvement in depression treatment outcomes in the intervention group compared with the usual care group, with significant patient (
5) and primary care provider (
7) satisfaction. Although not included in the original study, a recent survey of psychiatrists working in integrated care settings also demonstrated satisfaction working in this model (
10). In addition, 4 years after the completion of the IMPACT trial, a study found a significant reduction in overall health care costs in the intervention group (
8), demonstrating that the IMPACT model can meet the goals of the “triple aim” in health care: improved outcomes, reduced costs, and patient satisfaction (
9).
Replications of the IMPACT trial for the treatment of depression, referred to now as the collaborative care model, have been conducted, and more than 80 trials have demonstrated its effectiveness in a wide range of age groups, ethnic populations, and payer sources (
11–
13). An evidence base utilizing this model for the treatment of other mental health conditions is being developed, including good results for the treatment of anxiety disorders (
14) and emerging data for other conditions. Experimentation with varying ways to deliver collaborative care has also been tested, primarily in rural areas where telemedicine can extend services to remote locations, and in a study by Fortney et al. (
15), telemedicine-based collaborative care provided at a medical center demonstrated better outcomes than a practice-based intervention. In the area of child and adolescent psychiatry, an even more limited specialty resource, pediatric access lines provide services consisting of televideo for care management and psychiatric consultation to primary care settings (
16). Lastly, Katon and colleagues (
17) applied the model to the treatment of depression, diabetes, and coronary heart disease in a multicondition collaborative care trial called TEAMcare and demonstrated improvement in all conditions, an important outcome for patient-centered medical homes and other primary care treatment settings.
Widespread implementation of collaborative care has been hampered by siloed funding streams and lack of mechanisms to reimburse providers for indirect patient care, most of which is not billable in the current fee-for-service environment. This includes aspects of the model such as non-face-to-face contacts between the mental health provider—often referred to as a behavior health provider or care manager, usually trained in social work, psychology, or nursing—and the patient, curbside consultation between the psychiatric consultant, primary care provider, and behavioral health provider, and time to complete caseload-focused registry reviews. New funding mechanisms being tested in many states as a part of the ACA, such as bundled payments, case rates, and global capitation, must succeed in finding equitable ways to reimburse for this model for it to remain viable.
Core Principles of Effective Collaborative Care
A group of experts convened by the Advancing Integrated Mental Health Solutions Center developed a consensus on the essential features of the collaborative care model. The discussion crystallized the ideas into five core principles, which are summarized in
Table 1.
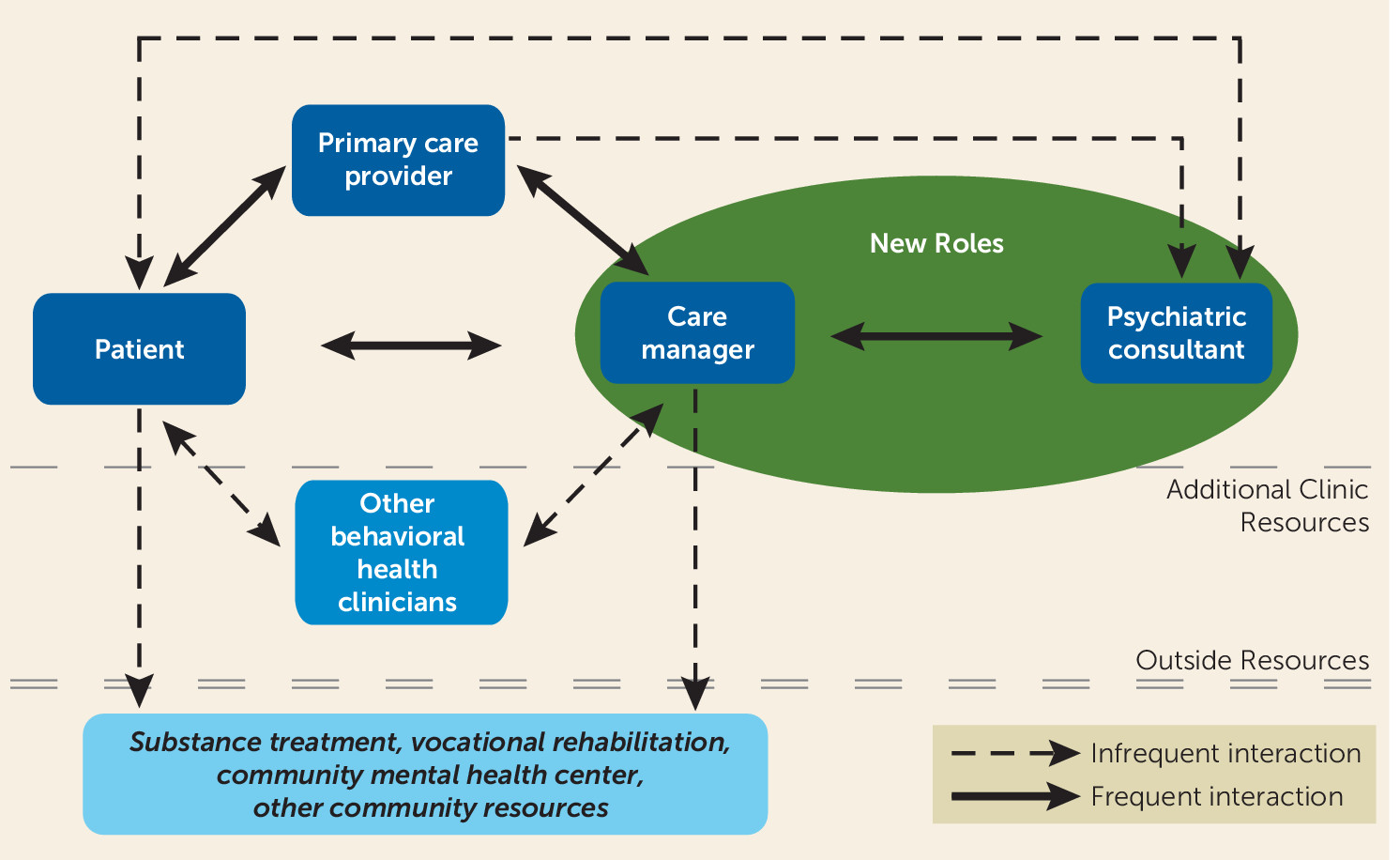
The Collaborative Care Team
The core members of the team include primary care providers, behavioral health providers, and psychiatric consultants (psychiatric nurse practitioners and physician assistants fill this role in some settings). The behavioral health provider is located in the primary care clinic with the primary care provider, utilizing screening tools and patient concerns to identify patients in need of mental health interventions. It is essential that behavioral health providers fit well into the fast-paced environment of primary care with a willingness to be interrupted and provide brief interventions (in contrast to traditional psychotherapies). Their skill set includes evidence-based brief interventions proven to work in the primary care setting, such as motivational interviewing, behavioral activation, and problem solving therapy. Flexibility, tenacity, an outgoing personality, and strong clinical skills are essential.
Preferably via a “warm hand-off,” the primary care provider introduces the patient to the behavioral health provider during the course of the primary care appointment, and the behavioral health provider then engages the patient and begins the assessment and treatment process. The team follows a “stepped care” approach that allows for immediate and appropriate treatment to be provided in the clinic without having to resort to referral to specialty mental health services unless this need is identified. This reserves higher levels of care for patients who are not improving or who have a more complicated presentation (
18). Tools such as the Patient Health Questionnaire–9 (PHQ) (
19), the 7-item Generalized Anxiety Disorder scale (GAD) (
20), and the Alcohol Use Disorders Identification Test (AUDIT) (
21) are commonly used, and the PHQ and GAD can be used for tracking progress in addition to screening. Over the course of treatment, the team refines the diagnosis and provides medication adjustments, brief behavioral interventions, and education. Adjusting treatment, including referral to specialty mental health care if needed, continues until treatment targets are met. The interactions of the team are illustrated in
Figure 1.
The Psychiatrist’s Roles in the Collaborative Care Model
The psychiatrist is a vital member of the collaborative care team. The roles of the psychiatrist are both specific and fluid, with opportunities to address clinical breadth as well as clinical depth in approaches to treatment. The psychiatrist plays several roles as a member of the team, including consultant (both direct and indirect) and educator, and he or she provides clinical and team leadership, including serving as a champion of the model. Some of the attributes of successful psychiatric consultants include being flexible, team oriented, and willing to tolerate interruptions, and enjoying educating others. Hiring someone without these characteristics can be detrimental to the process; it is fair to say that this work is not for everyone.
The infrequent use of
direct consultation (also referred to as formal consultation) in this model is one of its key features, promoting the extension of psychiatric expertise by allowing psychiatrists to utilize their face-to-face time (whether in person or via televideo) for only those patients who are not improving and providing
indirect consultation (see below) during the rest of the treatment process. In the original IMPACT trial, only 5%−7% of patients required direct evaluation by the psychiatrist (
5). These direct evaluations usually involve one or two visits with the psychiatrist, who provides a written summary of suggestions for the primary care provider and behavioral health provider to consider. Overall responsibility for the care of the patient remains with the primary care provider, and the consultant psychiatric provider does not order medications or additional tests and typically does not build a caseload of patients to follow on a routine basis.
Indirect consultation (also referred to as informal or “curbside” consultation) is the most frequent activity of psychiatrists working on these teams. It involves providing advice without directly evaluating patients, and it is critical to the extension of psychiatric expertise to more people in need. One primary goal of the consultation is to provide information immediately, so that the treatment can move forward at the time of the primary care appointment. This requires a willingness to be interrupted or return a call (or text or e-mail), ideally within an hour or at specified times during the day. Most consultation requests are for pharmacologic recommendations, followed by diagnostic clarification, and then recommendations for other forms of treatment (
10). Consultations typically take 3–5 minutes (personal communication from J. Kern, December 2014, based on unpublished data from 4,838 consultations) and cover a broad range of topics. The most common questions, by diagnostic category, have to do with mood, anxiety, and substance use disorders (
10).
Often the primary care provider will have the behavioral health provider make the call to the psychiatric consultant, utilizing the behavioral health provider as a conduit for information and mental health expertise in synthesizing the information being relayed. The psychiatric consultant usually does not document these brief consultations, and the primary care provider and behavioral health provider may or may not do so, depending on their practice preference. The psychiatric consultant gathers additional information from the primary care provider and behavioral health provider to help the team confirm a diagnosis or develop a provisional diagnosis and initiate a treatment plan. Because providing consultation for patients who have not been directly evaluated and making recommendations through a series of approximations may cause some uncertainty, more seasoned clinicians with a greater depth of expertise may find this work more suitable than clinicians with less experience. However, working with residents to hone these skills is important, since much of the excitement around practicing in integrated care settings is coming from the newly minted psychiatric workforce.
Consultation requests cover a broad range of age groups and diagnoses, and it is important for the consultant psychiatrist to be prepared to provide recommendations in a variety of areas. This often requires stretching one’s scope of practice to encompass areas in which one may have less familiarity and comfort. Additional course work and consultation with colleagues in other psychiatric specialty areas may be needed, in addition to refreshing one’s knowledge of general medical conditions, to be more conversant with primary care providers. An example of this is a family medicine physician calling a consultant psychiatrist, who is trained in adult psychiatry, with a question regarding treatment recommendations for a child. Rather than declining a consultation because of a lack of formal training in child and adolescent psychiatry, one reasonable course of action for the psychiatrist would be to inform the primary care provider that he or she will research the issue and call back. A desired outcome of this process of indirect consultation is developing the capacity of the primary care provider to recognize patterns of care in treating mental health conditions. As competency and confidence build, the consultant psychiatrist will begin to notice the primary care providers and behavioral health providers begin to ask more difficult questions as they learn to apply knowledge gained from the process of repeated consultations for similar clinical situations. In addition, the trust that develops between the team members as they gain confidence in each other’s areas of expertise and in their ability to apply what they have learned leads to fewer calls to the consultant psychiatrist over time.
It is unclear what constitutes a successful consultation experience, but several key factors are highlighted in
Table 2. The items in the category “build mutual trust and rapport” are considered to be some of the unspoken rules in the consultation process, and developing mutual respect and trust is crucial. Failure of the psychiatric consultant to adhere to them can lead to an unpleasant and unhelpful experience for other members of the team (
22). This is important to consider, as historically psychiatrists have been perceived by primary care providers as being unavailable (
23) and perhaps unwilling (
24) to provide consultation. The process of indirect consultation not only builds the capacity of the behavioral health provider and the primary care provider to treat mental health conditions but also promotes the development of trusting relationships between all team members. This is important, as primary care providers are being asked to step out of their comfort zone and provide care that is typically considered more within the scope of psychiatric practice, and trusting the consultant to be there and guide them through the process is an important feature in the success of the model.
Psychiatrists often have liability concerns about providing consultation for patients they have not directly evaluated. There are two things to consider in the provision of indirect consultation: 1) establishment of a doctor-patient relationship and 2) the nature of the administrative relationship between the providers. As for the first, historically, in many states, indirect consultation usually does not attain the threshold required in establishing a doctor-patient relationship, a step necessary in determining whether there is a duty to a patient in a malpractice situation. As for the second, care is being delivered by different providers, which establishes a form of “split treatment” familiar to psychiatrists. A supervisory relationship with the behavioral health provider or primary care provider, which is infrequent in these models, has the highest form of liability, since they report to the psychiatrist, who is then responsible for the oversight of the care they deliver. More frequently, the relationship is seen as consultative, with each party practicing independently. This form of split treatment traditionally carries the least liability. It is important to have the primary care provider remain in charge of all patient care, including ordering medications and any additional testing. The advice given by the consulting psychiatrist may or may not be implemented by the primary care provider or behavioral health provider and is rarely documented by the consultant in the patient’s medical record. Comprehensive guidance on this topic may be found in an APA resource document published in 2014 (
25).
Caseload-focused registry review is another form of indirect consultation and a necessary component of this population-based care model to allow the leveraging of psychiatric expertise to larger populations. Behavioral health providers or other designated staff enter patient information into a database, referred to as a registry, that includes results of screening and tracking tools (such as the PHQ and the GAD), medications prescribed, current mental health treatment, follow-up contacts, and other data deemed necessary by the team. On a regularly scheduled basis, often every 2–4 weeks, depending on the size of the caseload, the behavioral health provider and psychiatric consultant review the registry, focusing attention on the patients who are not improving and discussing options to intensify or “step up” their care. Twenty or more patients may be reviewed in an hour, and recommendations might include medication adjustments, changes in behavioral approaches, scheduling a face-to-face patient visit with the psychiatrist, or referral to a higher level of specialty mental health care. In addition to individual patient recommendations, aggregate data from the registry can be utilized in many ways, including determining whether there are specific areas that need more focus or areas of success that warrant dissemination. Pooled data is necessary if an organization is being reimbursed for the services rendered based on outcomes or other quality measures.
Education is an important aspect of the consultant psychiatrist’s duties, and it occurs in most interactions with the intent to build the capacity of the team members to treat mental health conditions. As such, every consultation request should be viewed as an opportunity to teach. The primary care provider and behavioral health provider are looking for information and guidance, and providing a brief explanation of why a specific recommendation was made goes a long way toward this goal and helps them gain confidence in their skills. More formal education on specific topics is usually welcome and can be provided over a meal or at other specified times. Sharing journal articles and joint attendance at meetings can also be helpful. Regardless of how the information is obtained, an important aspect of retaining knowledge is the ever-present availability of the consultant psychiatrist to reinforce the didactics through actual patient care experiences. It is important to appreciate that the psychiatrist is also a learner in this process, with much to gain from the knowledge and experience of the other members of the team.
Leadership opportunities exist for all members of the team, and psychiatrists are especially suited to fill this role. Sharing a background of medical education with the primary care providers and expertise in treating psychiatric disorders with the behavioral health providers, psychiatrists can help mitigate problems that occur as a result of cultural differences between the systems of care. The environments are quite different (
Table 3) and can lead to differing expectations of team members and approaches to patient care. Anticipating difficulties beforehand can lead to less frustration and should be the norm. Resistance to the model by team members who may initially be reluctant to change their familiar approach to care is a common barrier, but negotiable by the perceptive psychiatrist trained in group dynamics and expertise in behavior change. Buy-in from all team members, including administrative, nursing, and other staff, is essential, and “champions” within any of these areas can spark enthusiasm and make the system work more efficiently. An interesting multisite study (
26) highlighted the effects that these intangible differences can have. All sites received the same training and postimplementation support, and they had similar patient characteristics, but they demonstrated remarkably different outcomes, presumably as a result of these other influences. The role of the consulting psychiatrist is crucial to the team’s success. One study (
27) demonstrated that having an “engaged psychiatrist” had significant influence in patients reaching remission. While other examples of integrated care exist, it is the inclusion of psychiatric expertise and adherence to the guiding principles of the collaborative care model that can lead to more effective treatment (
28).
Summary and Conclusions
Each team member has a clear role on the collaborative care team, and the psychiatrist needs to be available to provide consultation and guidance in a readily accessible manner. Indirect consultation with primary care providers and behavioral health providers is a crucial part of the system of care, and key elements such as developing mutual respect and trust must be adhered to. Psychiatrists can prepare for working in integrated care environments by establishing collegial relationships with primary care providers and improving their general medical knowledge and the treatment of common mental health presentations in the primary care setting. Cultural differences between primary care and mental health care need to be well understood, and active monitoring of the team dynamics is an important role psychiatrists can play.
Integrating primary care and mental health provides new opportunities and challenges for psychiatrists. Understanding the fundamentals of the process allows a sophisticated application of psychiatric skills, already in short supply, to be leveraged across larger populations of patients. To meet this challenge, psychiatrists will need to be competent in their roles and be prepared to provide leadership as teams navigate these new relationships.
Acknowledgments
The author wishes to acknowledge the pioneering work of Wayne Katon, M.D., in the development, testing, and championing of the collaborative care model. He died March 1, 2015.