“Everything You Know Is Wrong”
—The Firesign Theatre, 1974
In this issue, Moffitt and colleagues (
1) pose a fundamental question: Is adult attention deficit hyperactivity disorder (ADHD) a childhood-onset neurodevelopmental disorder? Their provocative answer, based on the first follow-back and follow-forward analysis of a longitudinal community sample is: not necessarily.
For decades, ADHD and its nosological predecessors were “known” to afflict only elementary school-age boys. By the early 1990s, longitudinal follow-up studies documented that children with ADHD did not simply “grow out of it” (
2), even when hyperactivity receded. Revision of the diagnostic criteria in 1994 to encompass the predominantly inattentive subtype of ADHD increased the prevalence of ADHD diagnoses in adults, adolescents, and females of all ages (
3). Since then, ADHD investigators have extended their focus to adults.
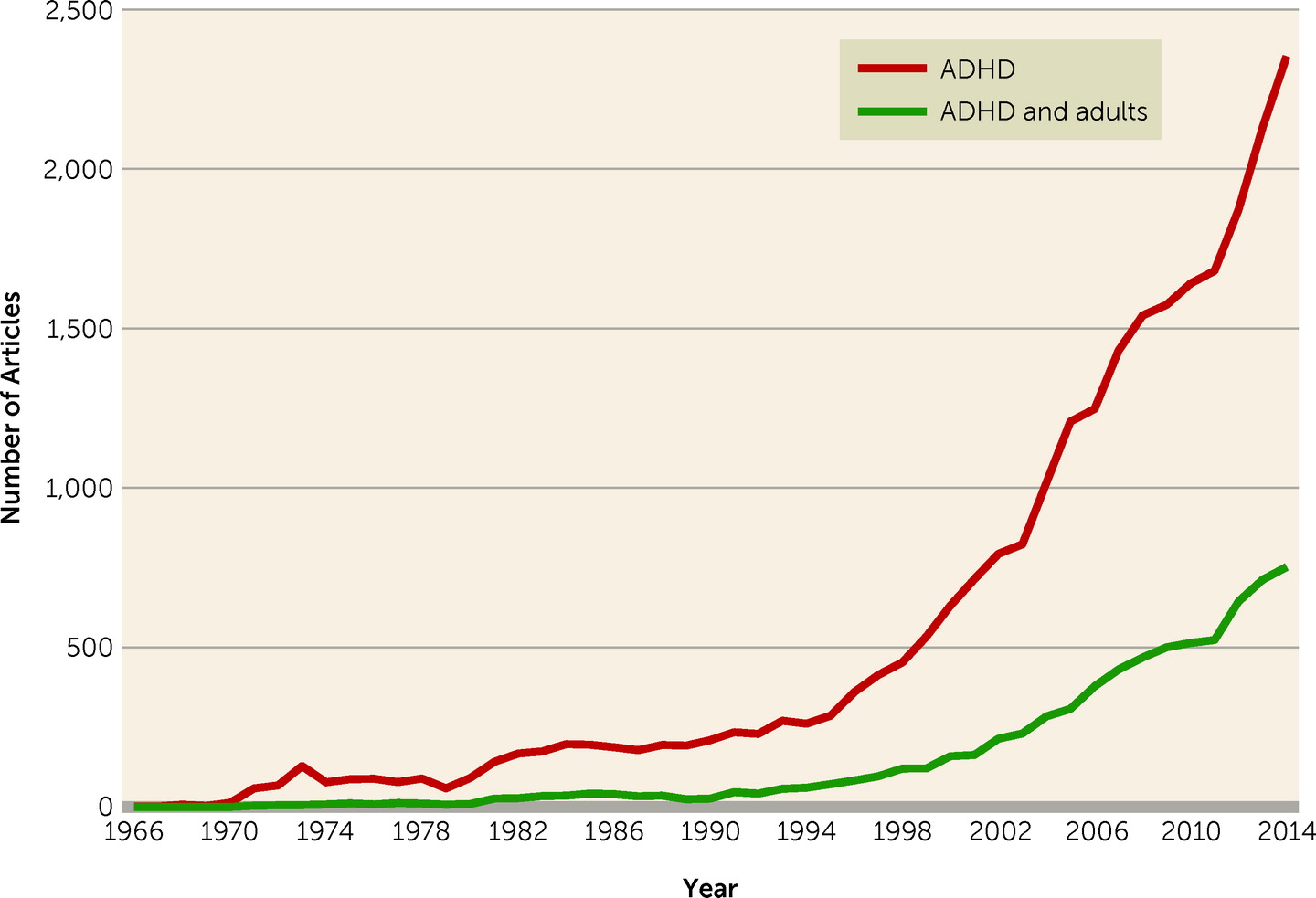
A paradigmatic, albeit untested, assumption of this growing literature (
Figure 1) has been that ADHD in affected adults represents a continuation of the childhood condition. This motivated the DSM-5 ADHD and Disruptive Behavior Disorders Work Group to assert that “ADHD begins in childhood” and to provide formal criteria for its diagnosis in older adolescents and adults using the same items as are applied in children.
In their study in this issue, Moffitt et al. examined the assumed continuity of ADHD in the Dunedin representative birth cohort of 1,037 individuals followed to age 38. Contemporaneous parent and teacher ratings identified 61 participants (6%) as meeting DSM-III criteria for ADHD in childhood. At age 38, 31 participants (3.1%) met DSM-5 criteria for ADHD, based on self-reports and informant reports. These prevalences are as expected. Surprisingly, however, the two sets of affected individuals barely overlapped. A grand total of three participants exhibited the expected continuity from childhood to adulthood.
This near-total lack of continuity has two parts. First, only about 5% of children in the Dunedin cohort with childhood ADHD continued to manifest the full DSM-5 syndrome in adulthood, although as a group they still exhibited substantial impairment. Moffitt and colleagues suggest that this rate of “decay” in meeting full diagnostic criteria is consistent with the limited extant literature (
4). It is certainly far below the rate of 22% who met full DSM-IV ADHD criteria in the New York Longitudinal Study at about the same age (
5). Inevitable differences between representative community samples and clinically ascertained samples may account for some of this gap. This gap further supports a nosological lacuna, corresponding to residual ADHD in adulthood (
4).
The second unexpected finding is the emergence of a substantial group of individuals who met all DSM-5 criteria for ADHD except that of onset by age 12. About 90% of these individuals were de novo cases—they had not met childhood criteria, nor come close, and they differed in multiple ways from those who had. Childhood ADHD probands exhibited neurocognitive impairments in childhood that were largely maintained in adulthood. By contrast, in adult ADHD probands, general intellectual ability was comparable to that of non-ADHD comparison subjects, and neuropsychological impairments were negligible, both in childhood and in adulthood. Still, both groups reported marked subjective cognitive difficulties as adults, and both exhibited objective evidence of psychosocial impairment: lower income, poor credit scores, cash flow problems, poor savings behavior, more government support, and higher numbers of insurance claims.
The inescapable conclusion is that a substantial number of individuals in a representative community sample exhibit impairing symptoms that are consistent with ADHD in all aspects except childhood onset. What might explain this? The possibility of malingering was excluded by the lack of potential secondary gain. At age 38, prodromal dementia also seems unlikely. The possibility that the impairments might be secondary to substance use disorders cannot be dismissed, but seems insufficient, as 55% of the adult ADHD participants had no other current diagnoses at age 38 (
1). As the authors write, the final “intriguing possibility is that adult ADHD is a bona fide disorder that has unfortunately been mistaken for the neurodevelopmental disorder of ADHD because of surface similarities, and given the wrong name” (
1).
Acceptance of such a novel entity will require independent replication, but that is unlikely to be rapidly forthcoming, as representative longitudinal samples followed prospectively from childhood are still “maturing” (
6). In the meantime, the plausibility of such a revolutionary interpretation is indirectly supported by another unexpected observation.
In the New York Longitudinal Study (
5), 23 of 80 (29%) individuals in the comparison group who had been recruited as nonhyperactive adolescents were diagnosed by blind clinical interviewers as having probable ADHD in their late 30s to early 40s (
7). Based on then-current DSM-IV-TR criteria, they were classified as having ADHD not otherwise specified, primarily because they lacked childhood onset. In brain structure, they did not differ significantly from the remaining 57 non-ADHD comparison subjects in any region, while they differed substantially in multiple brain areas from the 17 adults with persistent ADHD who were scanned (
7). As in the Moffitt et al. results (
1), this suggests that alternative mechanisms may be at play, despite the symptomatic overlap.
Some insight into a potential mechanism is offered by the work of Arnsten and colleagues in the nonhuman primate. In a landmark study (
8), their group noted specific loss of the persistent firing in prefrontal neurons that subserve working memory beginning by middle adulthood (12- and 13-year old male rhesus monkeys), whereas the firing of cue-onset neurons did not differ between young adults (7- and 9-year olds) and older animals (ranging up to 21 years old). The age-related degradation in the ability of neurons to detect preferred from nonpreferred spatial directions was ameliorated by pharmacologic manipulations that reversed age-related increases in cyclic adenosine monophosphate (cAMP) signaling or blocked the effects of excess cAMP on downstream potassium channels (
8). The finding that the persistent firing that undergirds working memory in primates is particularly sensitive to age-related deterioration raises the question of whether other core executive functions, such as response inhibition, may be equally vulnerable. If so, the adult onset of an ADHD-like syndrome would be an expected outcome in primates such as humans.
Against this background, considering the novel Dunedin results in light of The Firesign Theatre’s comical warning, “Everything You Know Is Wrong,” suggests an intriguing line of investigation. In the New York Longitudinal Study, brain structure differences (decreased gray matter/cortex) in adulthood were more reflective of childhood diagnosis than of adult diagnostic status (
7). Despite the challenges of relating neuropsychological performance to subjective assessments of executive function (
9), studies examining the neurobiology, neuropsychology, and functional profiles of individuals with prospectively confirmed lack of childhood ADHD who nevertheless currently meet adult ADHD criteria may reveal a novel treatable syndrome
and its associated mechanism. Taking The Firesign Theatre seriously may open a path to precision medicine in the age of Research Domain Criteria (
10).
Acknowledgments
The author appreciates edits suggested by Felice Kaufmann, Ph.D.