Body dysmorphic disorder is characterized by a distressing or impairing preoccupation with slight or imagined defects in physical appearance associated with repetitive, compulsive behaviors in response to these concerns. In DSM-5, body dysmorphic disorder is classified as an obsessive-compulsive and related disorder, and pharmacological treatments for body dysmorphic disorder have been informed in part by treatments for obsessive-compulsive disorder (OCD). Patients with body dysmorphic disorder, as is seen in OCD, have been shown to have a selective efficacy of treatment response to serotonin reuptake inhibitors (SRIs). Double-blind crossover trials in body dysmorphic disorder demonstrate that the SRI clomipramine improves severity of body dysmorphic disorder and that the norepinephrine-reuptake inhibitor desipramine is not as effective (
1). It has been shown that continuing treatment with selective serotonin reuptake inhibitors (SSRIs) reduces the likelihood of relapse during continuation treatment in OCD (
2–
4) and that relapse of OCD upon discontinuation is associated with worsening of quality of life and level of disability (
5), but such work has not been conducted to date in body dysmorphic disorder. While both disorders are chronic conditions, patients with body dysmorphic disorder have even poorer insight; more common co-occurrence with depression, social anxiety disorder, and substance use disorders; and higher risk of suicidal ideation than those with OCD (
6). Thus, information from a prospective study on relapse prevention, as well as on the efficacy of ongoing treatment in body dysmorphic disorder, is of critical importance and is the focus of the article by Phillips et al. in this issue (
7).
In fact, optimal duration of treatment is a central question in the development of all psychiatric treatments. It is important to understand the consequences of discontinuing medication, just as it is to understand the consequences of discontinuing psychosocial or neuromodulation treatment. We have come to appreciate that anxiety disorders and obsessive-compulsive and related disorders are chronic disorders, but our understanding of the optimal length of treatment for these disorders is limited. Freud contributed to our appreciation that ongoing, rather than very brief, treatments of neurotic disorders could be of longer-lasting benefit. It is well established in cases of schizophrenia and bipolar disorder that ongoing medication management is paramount and that discontinuation of and/or nonadherence to effective medication treatment is associated with relapse of illness. Relapse prevention studies examine the question of what happens to patients when ongoing effective treatments are discontinued, and such knowledge is crucial in body dysmorphic disorder.
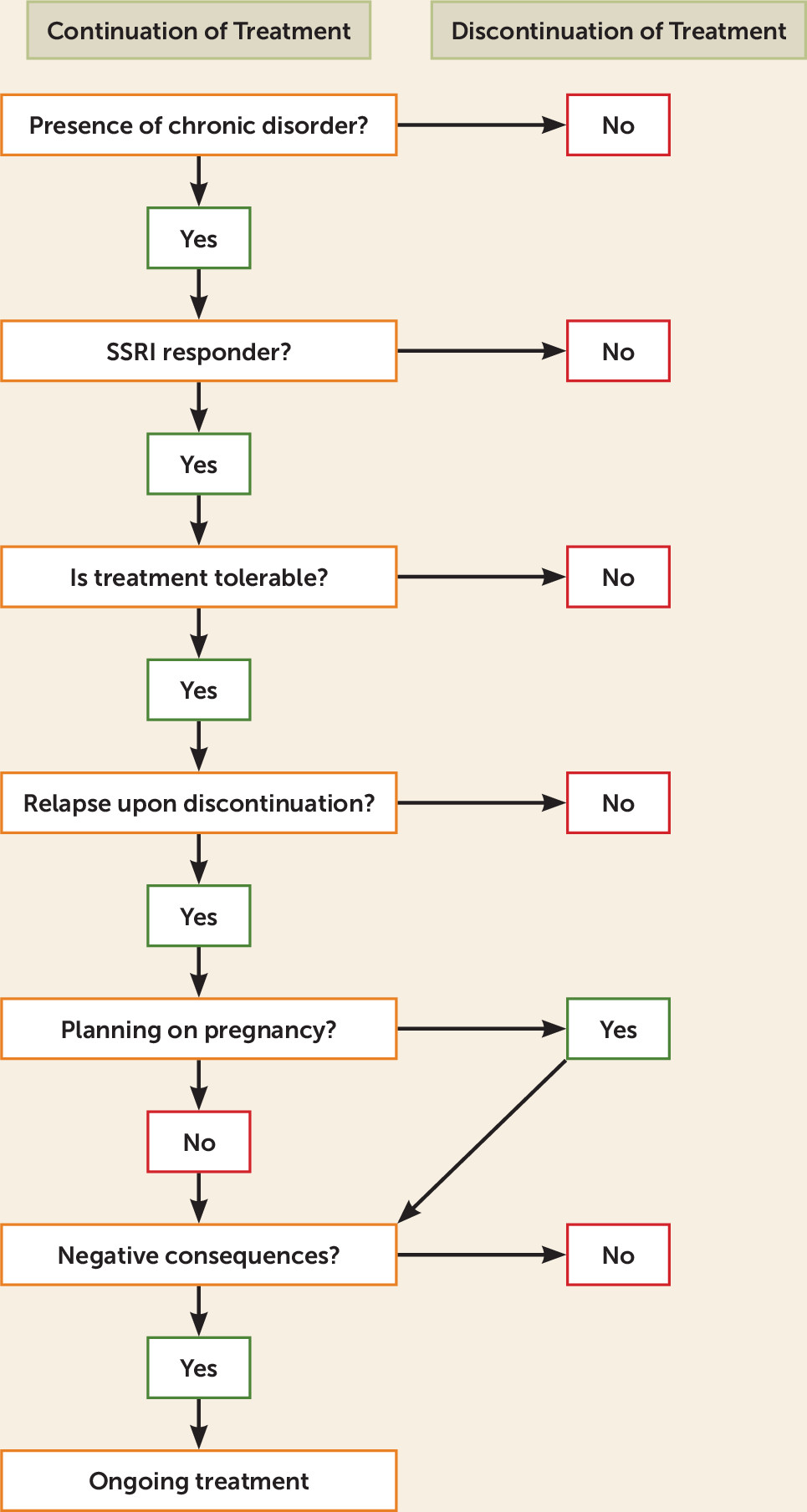
In this issue, Phillips et al. examine pharmacotherapy continuation and discontinuation in patients with body dysmorphic disorder (
7; see also
Figure 1). The study was split into two phases. In phase 1, patients were provided with open-label escitalopram for 14 weeks, which had been previously suggested as being safe and efficacious for use in treatment of body dysmorphic disorder (
8). Permitted dosages were varied to improve tolerability. Nonresponders were removed from the study at the end of phase 1. Subjects who had completed phase 1, responded to escitalopram treatment, and agreed to continue in the study were carried forward into phase 2. Subjects were randomly divided into groups: one discontinuing escitalopram to start placebo and the other continuing monotherapy with escitalopram. Assessments were conducted regularly throughout.
Of the 100 subjects in phase 1, 67% of the escitalopram-treated subjects and 81.1% of completers were responders. In addition, 20% of those treated and 25.7% of completers fully remitted. Scores on the Yale-Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder (BDD-YBOCS) decreased by an average of 54.4% in the completer population. Body dysmorphic disorder severity and insight, depressive symptoms, psychosocial function, and quality of life significantly improved from baseline to end of phase 1. Responsivity did not significantly differ between delusional and nondelusional subjects, and neither was it significantly influenced by baseline symptom severity or duration, associated depressive symptoms, gender, or minority status. The 58 responders who continued into phase 2 were randomized into groups to continue escitalopram treatment or to discontinue escitalopram for placebo. Time to relapse was significantly longer with escitalopram than with placebo; by the end of phase 2, relapse proportions were 40% in the case of placebo as opposed to 18% for escitalopram continuation. Phase 2 subjects who continued escitalopram treatment continued to improve beyond initial improvements in phase 1 by an average of 4.1 points, according to the BDD-YBOCS scores, with 35.7% of subjects showing further improvement. Overall, 25% of escitalopram-treated subjects and 46.7% of placebo-treated subjects experienced at least one adverse event possibly related to study medication, and no serious adverse events occurred during either treatment phase.
The use of escitalopram in the treatment of body dysmorphic disorder and in relapse prevention requires further characterization, particularly in the form of larger sample sizes and longer follow-up periods. Self-reported relapse is further complicated by the possibility of discontinuation symptoms being mistaken for true relapse. It is also important to note that the exclusion criteria for subject selection removed often severe and strongly associated comorbidities, such as suicide risk and substance abuse (
9). The use of a placebo is also not completely representative of what occurs in clinical practice, where the patient exerts personal agency in discontinuation of treatment. A deepened understanding of relapse in the context of body dysmorphic disorder is both informed by and contributes to our understanding of related disorders as well, particularly within obsessive-compulsive and related disorders.
Recent treatment guidelines, such as the 2014 British Association of Psychopharmacology guidelines for the pharmacological treatment of anxiety disorders, posttraumatic stress disorders, and obsessive-compulsive disorders, proposed that optimal treatment of OCD involves indefinite pharmacological treatment with SSRIs (
10). Most (but not all) placebo-controlled trials of relapse prevention in OCD patients suggest that for those who have responded to previous acute treatment, there is a significant benefit in staying on active medication (escitalopram, fluoxetine in high doses, paroxetine, and sertraline) compared with beginning placebo, for up to 12 months (
2). However, the optimal duration of continuation treatment is unclear; the current recommendation in SSRI-responsive patients is to continue drug treatment for at least 12 months. In the absence of evidence for relapse-risk reduction over time, guidelines suggest ongoing treatment. This is of particular concern in patient groups who often discontinue SSRI treatment, such as women planning to become pregnant. This group would be at risk of relapse given the results presented in this issue by Phillips et al.
Relapse of OCD is associated with considerable impact on quality of life and disability; in a relapse prevention study of OCD with escitalopram (the same agent studied by Phillips et al. in body dysmorphic disorder), an increase in the YBOCS total score of at least 5 points was associated with significant impairment in quality of life (on all domains of the Medical Outcomes Study 36-item Short-Form Health Survey, including mental health, role-emotional function, and social function) and disability (on all Sheehan Disability Scale measurements, including family life, social life, and work) (
5). Thus, patients who relapsed upon discontinuation were more likely to lose their jobs; get divorced; and manifest impairment in work, family, and social life. Patients who relapse may even fare worse in work and relationships (role-emotional function) compared with their level of functioning with their initial illness. Thus, future studies are needed to examine ways to increase medication adherence in body dysmorphic disorder and to develop strategies to enhance compliance for long-term treatments.