People with depression view themselves through a critical lens. They see themselves as “worthless, incapable of any achievement, and morally despicable,” according to Freud (
1), and as “defective, inadequate, diseased, or deprived,” according to Beck and colleagues (
2). Such disturbances in self-appraisal are a fundamental feature of depression, and they are specifically addressed by effective psychotherapies for the illness (
2,
3).
Neurobiological research into self-appraisal processes has consistently implicated activity of midline cortical regions, in particular the medial prefrontal cortex and the posterior cingulate cortex (
4,
5). These regions are core components of the so-called default mode network, which shows greater activity and connectivity when a person is at rest than when engaged with external tasks. The substantial overlap between self-related and resting-state brain activity can be explained, at least in part, by the fact that people spend more time introspecting and daydreaming when they are not engaged with the external environment (
6,
7).
We recently characterized a dynamic network model of self-directed cognition composed of the medial prefrontal cortex, the posterior cingulate cortex, and the inferior parietal lobule (
8). Self-related processes—at rest and when one is prompted to explicitly think about one’s attributes—are supported by activity in posterior regions and regulated by feedback from the medial prefrontal cortex, with this structure’s regulatory influence further enhanced by the more effortful self-directed cognition required by explicit self-appraisal.
Alterations in functioning of the medial prefrontal cortex have frequently been implicated in major depressive disorder. Early nuclear imaging studies of depression reported increased activity in the medial prefrontal cortex during rest (
9–
11). More recent functional MRI (fMRI) studies have reported increased resting-state connectivity between the medial prefrontal cortex and other default mode regions (
12–
14). While these resting-state abnormalities suggest a possible brain substrate for the alterations in self-appraisal observed in depression, they do not demonstrate it directly. Studies that have examined the response to self-referential stimuli in depression have been inconsistent, reporting that activity in the medial prefrontal cortex is both increased (
15,
16) and decreased (
17,
18), leaving the mechanisms linking alterations in medial prefrontal cortical functioning with disturbed self-appraisal in depression uncertain.
There is a clear need for more sophisticated brain models, including the use of computational models that allow for a more concise mapping between brain activity and psychological states (
19). Dynamic causal modeling provides a principled means of characterizing the role of the medial prefrontal cortex in depression by measuring its dynamic interactions—or
effective connectivity—with other regions, inferring the strength and direction of regional interactions (
20).
The aim of this study was to examine disturbed self-appraisal processes in depression, with an emphasis on the medial prefrontal cortex. Our study included adolescents and young adults, allowing us to focus on a developmental period when self-related concepts have become especially salient (
21,
22) and when vulnerability to depression has risen substantially from childhood (
23). The increased salience of the self, and greater vulnerability to depression, are likely related to neurodevelopmental processes that continue throughout adolescence and early adulthood (
24), not ending until the mid-20s (
25,
26). We hypothesized that disturbed self-appraisal—we use the term “disturbed” in its everyday sense, as referring to a disruption of normal functioning—would be reflected in depressed young people appraising themselves in more negative terms and that this would be associated with altered interactions between the medial prefrontal cortex and the posterior cingulate cortex. We additionally sought to investigate how variability in the clinical presentation of depression, including comorbid anxiety, covaried with alterations in network parameters related to self-appraisal.
Method
Participants
Eighty-six unmedicated depressed participants were recruited from mental health clinics in the western and northern suburbs of Melbourne, Australia. Patients were between 15 and 25 years of age and had major depressive disorder, as assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (
27). The depression was of at least moderate severity, defined as a score ≥20 on the Montgomery-Åsberg Depression Rating Scale (MADRS). These young patients were typically in the early phases of illness, when the cumulative effects of treatments, recurrence, and chronicity have yet to accrue. Exclusion criteria were diagnoses of psychotic or bipolar disorders; full-scale IQ <85, as estimated by the Weschler Test of Adult Reading (
28); and current treatment with medication. Two-thirds of the depressed participants (66%) had a comorbid anxiety disorder, reflecting the relatively severe clinical presentation in these young people, all of whom were attending mental health services. The most common comorbid anxiety disorder was social anxiety disorder, which was present in 35% of patients (
Table 1).
This clinical cohort was compared with control participants matched for age and sex. Ninety-five healthy control participants were recruited by advertisements placed in online media. Exclusion criteria were current or past diagnoses of mental illness according to assessment with the SCID and an estimated IQ <85. These participants were included in our previous report of a brain model of self-directed cognition (
8). All participants (and their parents if they were under 18 years of age) provided informed consent to participate in the study, which was approved by the Melbourne Health Human Research and Ethics Committee.
Paradigm Design
Participants completed an fMRI task composed of three experimental conditions: self-appraisal, external attention, and rest-fixation. In the self-appraisal condition, participants were presented with a personality adjective and asked whether or not the word described them. Words were drawn from a frequently used list of personality adjectives (
29) and included words such as “skeptical,” “perfectionistic,” and “lucky.” We selected words that were distributed around the median rating for “likeableness” reported in the original data set, from the subset of words rated as most “meaningful” (
8). Participants viewed eight blocks of six words, presented for 5 seconds each, and responded to the question “Does this word describe you?” by pressing the left or right button on a response pad. In the external attention condition, participants viewed eight blocks of six words, also presented for 5 seconds each, and responded to the question “Does this word have four or more vowels?”
The two lists of 48 words that formed the self-appraisal and external attention conditions were matched on likeableness ratings and number of vowels and were counterbalanced across participants. Each 32-second block (2 seconds of instruction followed by six words presented for 5 seconds each) was interspersed with a 10-second rest-fixation block in which participants were asked to fixate on a centrally presented crosshair. Behavioral data (accuracy and response times) were analyzed with Stata, version 14.1 (StataCorp, College Station, Tex.).
Image Acquisition
Functional neuroimaging data were acquired using a 3-T GE Signa Excite system equipped with an eight-channel phased-array head coil in combination with ASSET parallel imaging. The functional sequence consisted of a single-shot gradient-recalled echo planar imaging sequence in the steady state (repetition time=2 seconds, echo time=35 ms, pulse angle=90°) in a 23-cm field of view, with a 64×64–pixel matrix and a slice thickness of 3.5 mm (no gap). Thirty-six interleaved slices were acquired parallel to the anterior-posterior commissure line with a 20° anterior tilt to better cover ventral prefrontal cortical brain regions. The total sequence time was 11 minutes 22 seconds, corresponding to 341 whole brain echo planar imaging volumes. A T1-weighted high-resolution anatomical image was acquired for each participant to assist with functional time series coregistration (140 contiguous slices, repetition time=7.9 seconds, echo time=3 seconds, flip angle=13°, in a 25.6-cm field of view, with a 256×256–pixel matrix and a slice thickness of 1 mm).
Image Preprocessing
Imaging data were processed with SPM12 (Wellcome Trust Centre for Neuroimaging, London) using MATLAB, version 8.2 (MathWorks, Natick, Mass.). Motion correction was performed by aligning each participant’s time series to the first image using least-squares minimization and a six-parameter rigid-body spatial transformation. Participants’ data were excluded if movement in the translational or rotational planes exceeded 2 mm or 2°, respectively. These realigned functional images were then coregistered to the participants’ respective T1 anatomical scans, which were segmented and spatially normalized to the International Consortium for Brain Mapping template using the unified segmentation approach. The functional images were interpolated to 2 mm isotropic resolution and were smoothed with a 5 mm full width at half maximum gaussian filter.
Of the 181 participants who completed the scanning session, 22 were subsequently excluded—10 because of excessive head movement during scanning (seven in the depressed group and three in the control group) and 12 because of poor performance on the external attention task, defined as less than 85% accuracy (eight in the depressed group and four in the control group). The final imaging sample thus included 71 depressed and 88 control participants (
Table 1). The groups showed a modest but significant difference in full-scale IQ, and IQ was added as a covariate in all group comparisons.
Defining the Nodes
The nodes for our dynamic causal modeling analyses were identified using a general linear model approach in SPM12. We defined the nodes as regions that were 1) more active during self-appraisal and rest-fixation than during external attention, and 2) additionally activated by self-appraisal over and above rest-fixation. We used the external attention condition as the implicit baseline. It was an appropriate baseline condition for our objectives, being matched with self-appraisal on stimulus features, but mandating specific attentional demands that suppressed the likelihood of task-independent activity. For each participant, primary regressors for the self-appraisal and rest-fixation conditions were defined by specifying the onset and duration of each block. The regressors were convolved with a canonical hemodynamic response function, and a high-pass filter set at 128 seconds was used to remove low-frequency drifts. Parameter estimates were calculated at each voxel using the general linear model with local autocorrelation correction.
As in our previous study (
8), the second-level analysis identified regions that showed significant conjunction between activation to rest-fixation and activation to self-appraisal minus rest-fixation. In other words, the nodes for our dynamic causal modeling analysis were composed of brain regions that were broadly activated by self-appraisal (across rest-fixation and self-appraisal conditions) but further activated by explicit self-appraisal. Whole brain, voxel-level, family-wise error corrected statistical thresholds were applied to define these regions (family-wise error corrected p<0.05).
As in our previous work, these contrasts identified regions in the medial prefrontal cortex, posterior cingulate cortex, and left inferior parietal lobule. Within these broader regions, we then defined subject-specific volumes of interest following the principles established by Stephan et al. (
30), which outline the requirement to define subject-specific time series whose precise anatomical location varies. The group coordinates for the volumes of interest were the maxima for the main effect of self-appraisal and rest-fixation for clusters in the medial prefrontal cortex, posterior cingulate cortex, and inferior parietal lobule. For each participant, we extracted regional time series, summarized as the first eigenvariate of voxels that showed significant activation to self-appraisal and rest-fixation (p<0.01) within 5 mm of the subject-specific maxima, which were themselves no more than 10 mm from the group maxima. The dynamic causal modeling analysis included only participants who had volumes of interest identified in each of the three regions according to these criteria. We extracted time series for all volumes of interest from 68 of the 71 depressed participants and from 82 of the 88 control participants.
Dynamic Causal Modeling
The aim of dynamic causal modeling is to infer the causal architecture of a network of neural regions. Using a Bayesian approach, a model is selected from a set of predefined models that is the most likely to generate the observed imaging data while also penalizing for model complexity. The dynamic causal models delineate how dynamics in one brain region influence dynamics in others, incorporating both the core set of interregional connections and the modulation of those influences by the experimental manipulations (
31). Effective connectivity between brain regions—the directed influence one region has on another—can be either positive or negative, such that an increase in activity in one region causes an increase or decrease, respectively, in the rate of change in another (for more detailed descriptions, see references
31,
32).
For this study, a three-region deterministic dynamic causal model was specified for each participant, with bidirectional effective connections between the medial prefrontal cortex, posterior cingulate cortex, and inferior parietal lobule. We defined a space of 32 candidate models where “broad self” (self-appraisal and rest-fixation) drove either the medial prefrontal cortex (models 1–16) or the posterior cingulate cortex (models 17–32). Self-appraisal modulated efferent connections from the medial prefrontal cortex to the posterior cingulate cortex, the inferior parietal lobule, both, or neither, and/or connections from the posterior cingulate cortex to the medial prefrontal cortex, the inferior parietal lobule, both, or neither (i.e., a 2×4×4=32 candidate model space; see Figure S1 in the data supplement that accompanies the online edition of this article).
Within the depressed and control groups, the models were compared using random-effects Bayesian model selection in DCM12 in SPM12. We computed posterior probabilities and protected exceedance probabilities within each group (
33,
34). The protected exceedance probability, which represents the probability that a given model is more frequent than the others (above and beyond chance), was our primary measure for model selection (
33). The strength of effective connectivity and modulatory effects was summarized using random-effects Bayesian model averaging. Bayesian model averaging, which is the recommended approach for comparing parameter estimates from dynamic causal models between groups, involves computing the average model parameters, weighted by the posterior probability of each model (
31). The model space was partitioned according to whether “broad self” drove the medial prefrontal cortex (models 1–16) or the posterior cingulate cortex (models 17–32), and average connectivity estimates (weighted by their posterior model probabilities) were obtained from models in the winning family for each group (
35). Between-group differences for the model parameters were examined using logistic regression in Stata, adjusting for estimated IQ, reaction times, age, and sex. Analyses of between-group differences for the model parameters were adjusted for multiple comparisons using the false discovery rate (
36) to determine significance (q<0.05).
We further analyzed associations between the relevant connectivity parameter and clinical and behavioral characteristics of the depressed participants. This included depression severity, as assessed by the MADRS. We performed a factor analysis of the MADRS to determine associations with symptom dimensions, using methods similar to those of previous analyses of the instrument (
37,
38). This involved calculating the principal-component factors, retaining those with an eigenvalue greater than 1, and subjecting them to oblique rotation. We then calculated partial correlations between the factors and our model parameter of interest, adjusted for total MADRS score, reaction times, age, and sex. Analyses of associations with clinical and behavioral variables were adjusted for multiple comparisons using the false discovery rate (
36) to determine significance (q<0.05). We also examined the effects of anxiety comorbidity in the depressed participants, focusing especially on social anxiety disorder, which was the most prevalent disorder.
Results
Behavioral Results
Overall task performance did not differ significantly between the depressed and control groups (
Table 1). There was no significant difference in accuracy in the external attention condition, and the groups demonstrated similar reaction times for the self-appraisal and external attention tasks. The depressed participants more often answered “yes” to the question “Does this word describe you?” (p<0.001), and the mean likeableness ratings for words that were affirmed as describing the self were significantly lower for the depressed compared with the control group (p<0.001).
Identifying a Common Model
The conjunction analyses of the rest-fixation (versus external attention baseline) and the self-appraisal minus rest-fixation contrasts identified, independently, three regions in each group—in the medial prefrontal cortex, the posterior cingulate cortex, and the left inferior parietal—showing a high degree of anatomical consistency (
Figure 1; see also Table S1 in the
online data supplement). There was evidence of increased posterior cingulate cortex activation to the self-appraisal condition in the depressed compared with the control group (p=0.01) (
Figure 1).
The three regions identified for each group were included in a dynamic network, and dynamic causal modeling was used to determine the network’s most likely structure, given the data. Notably, we validated our previously described model (
8), showing that for both the control and depressed groups, the same model outperformed the other models. This common winning model was composed of a driving influence of “broad self” (self-appraisal and rest-fixation) on the posterior cingulate cortex, with self-appraisal modulating both of the efferent connections from each of the posterior cingulate cortex and the medial prefrontal cortex (
Figure 2). In the control group, the winning model had a protected exceedance probability of 0.90, and in the depressed group, 0.92 (see Figure S2 in the
data supplement).
Estimating and Comparing the Model Parameters
Parameter estimates were calculated using Bayesian model averaging over a model space partitioned according to whether “broad self” drove activity in the posterior cingulate cortex or medial prefrontal cortex. We found clear evidence in both groups to suggest that “broad self” drove posterior cingulate cortex activity (in both groups, the exceedance probability was >0.99). In both groups, Bayesian model averaging over the 16 candidate models in the winning family demonstrated significant positive endogenous influences from the posterior cingulate cortex to the medial prefrontal cortex—directly and indirectly via the inferior parietal lobule—and significant negative endogenous influences from the medial prefrontal cortex to the posterior cingulate cortex. The modulatory effects of self-appraisal were such that the posterior cingulate cortex had a greater positive influence on the medial prefrontal cortex and inferior parietal lobule, and the medial prefrontal cortex had a greater negative influence on the posterior cingulate cortex. For the depressed group, but not the control group, the medial prefrontal cortex also had a significant negative influence on the inferior parietal lobule (
Figure 2,
Table 2).
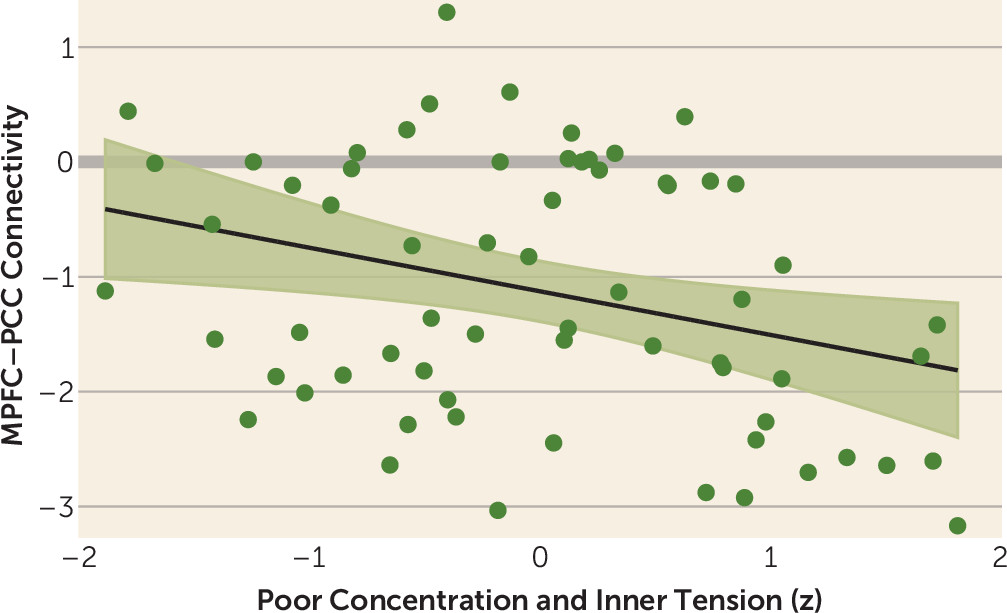
Between-group comparison showed that the modulatory influence of self-appraisal on effective connectivity between the medial prefrontal cortex and the posterior cingulate cortex (henceforth referred to as “MPFC-PCC connectivity”) was significantly more negative for the depressed compared with the control group (odds ratio=0.54, 95% CI=0.38, 0.77; p=0.0008) (
Figure 3,
Table 2). The influences of sex and age on the connectivity parameters are presented in Tables S2 and S3 in the
online data supplement.
Association With Clinical and Behavioral Variables
We examined associations between the strength of modulation of connectivity between the medial prefrontal cortex and posterior cingulate cortex and clinical and behavioral characteristics of the depressed participants. There was no association between MPFC-PCC connectivity and variables related to self-appraisal (proportion of personality adjectives affirmed or their valence), nor was there significant association between connectivity and total MADRS score. Our factor analysis of the MADRS revealed the presence of four underlying factors, similar to the analysis by Craighead and Evans (
38) (see Table S4 in the
data supplement). As in their analysis, we observed a factor that consisted of the MADRS items concentration difficulties (“difficulties in collecting one’s thoughts mounting to incapacitating lack of concentration”) and inner tension (“feelings of ill-defined discomfort, edginess, inner turmoil, mental tension”) (
39). The strength of modulation of MPFC-PCC connectivity was significantly negatively correlated with this factor (r=−0.32; 95% CI=−0.51, −0.08; p=0.01) (
Figure 4; see also Table S5 in the
data supplement), such that depressed patients who had greater difficulties with concentration and greater inner tension showed even more negative MPFC-PCC connectivity. Additional tests for associations between MPFC-PCC connectivity and clinical and behavioral variables, and between the concentration/tension factor and clinical and behavioral variables, are presented in Table S5.
Comparison of depressed participants with comorbid social anxiety disorder (N=24) with depressed participants without an anxiety disorder (N=23) showed significantly more negative modulation of MPFC-PCC connectivity in the former group (odds ratio=0.44; 95% CI=0.22, 0.87; p=0.02). Details of the subgroups with and without social anxiety disorder are presented in Table S6 in the data supplement.
Discussion
We studied brain network functioning in a large sample of unmedicated help-seeking depressed adolescents and young adults and found specific and novel disturbances in effective connectivity associated with self-appraisal processes. We first validated the same dynamic network model in depressed participants as in the control participants—one in which the medial prefrontal cortex acts to direct self-related processes by regulating posterior cingulate cortex activity, which is enhanced during explicit self-appraisal. The magnitude of this negative influence is even more pronounced in depression, suggesting that the medial prefrontal cortex has a “hyperregulatory” influence in the illness.
The medial prefrontal cortex, particularly the most rostral portion (Brodmann’s area 10) implicated in our model, is activated by a diverse range of tasks (
40). They have in common that they require integration of stimuli from different sources, such as in analogical reasoning, where one set of concepts is mapped to another (
41). In integrating stimuli from different sources, the rostral medial prefrontal cortex has a role in selectively attending to and switching between them (
42), thereby supporting cognitive flexibility (
43).
These integrative processes are important in the self-appraisal task, which requires mapping abstract semantic concepts to internal representations. In our model, the medial prefrontal cortex appears to modify self-representations generated by posterior cortical regions to integrate them with the meaning of the personality adjectives (
8).
The behavioral results of our study confirm that the self is appraised more negatively in depression and show that this is associated with more negative MPFC-PCC connectivity in the depressed compared with the control participants. The self-concept shows complex changes in depression: it is not only more negatively appraised, but also, as a result of the changing sense of self, less stable (
44). This more aversive and unstable self is likely to take more cognitive effort to appraise, consistent with our understanding of rostral medial prefrontal cortical function.
The particular aspects of self-appraisal that are associated with the MPFC-PCC connectivity parameter are difficult to confirm with our data, although we have provisional evidence. The strength of MPFC-PCC connectivity was associated with a depression factor composed of difficulty with concentration and inner tension. Depressed participants with high levels of the factor may have had more difficulty with the conceptual integration and cognitive flexibility demanded by the self-appraisal task. Of note, these participants were biased toward affirming the personality adjectives (see Table S5 in the
data supplement), likely exacerbating the appraisal demands. The demands of the task were conceivably even greater in participants with comorbid depression and social anxiety disorder. In both disorders there is evidence of an increase in self-focused attention that is accompanied by difficulties shifting attention between self-related and external stimuli (
45).
Our study has examined one aspect of self-related processing—the cognitive appraisal of the self’s personality attributes. Other aspects of the self are also disturbed in depression—for example, in its relationship to negative memory biases (
46) and interoceptive awareness (
47). Future studies could extend our model to study the importance of the medial prefrontal cortex in regulating the relevant networks. Similarly, we observed effects related to posterior cingulate cortex function that suggest broader imbalance in the default mode network’s contributions to self-disturbance, which could also be elaborated in future studies.
Other limitations of our study should be noted. It is not clear that the connectivity changes we have demonstrated are specific to depression. We showed that MPFC-PCC connectivity was even more disturbed in patients with comorbid major depressive disorder and social anxiety disorder, but we did not have a group with social anxiety disorder alone to clarify the extent to which the changes might be attributable to the disorder. Second, while there are clear advantages to studying young patients early in the course of illness—during a period in which self-related concepts are particularly salient and depression is less chronic and less likely to be influenced by treatments—the focus limits the extent to which the results might be generalized to the broader population of depressed adults. It is also a period in which neurodevelopmental processes are ongoing—a factor likely related to increased depression vulnerability—and while we accounted for linear age-related changes, it is possible that brain connectivity differences will be less prominent in later periods. It will be important to examine our model in older depressed populations. Last, factor analysis requires a degree of subjectivity in decisions related to the procedure, with no objective criteria for an optimal solution (
48). Our examination of connectivity associations with the MADRS concentration/tension factor should therefore be considered exploratory.
Our study of a large group of unmedicated participants with moderate to severe depression allowed us to apply a neural modeling approach that was able to more fully characterize the connectivity parameters that underlie disturbed self-appraisal processes in depression and map them to aspects of the clinical presentation. Our model demonstrates that the medial prefrontal cortex has a critical role in coordinating an integrated and dynamic neural representation of the self. Many studies have implicated abnormal medial prefrontal cortical function in depression (
9–
18), which these findings suggest might be a reflection, in part, of disturbances in the way the medial prefrontal cortex directs self-appraisal processes. The connectivity disturbances suggest themselves as targets for cognitive-behavioral therapy and other therapies that aim to affect change in the way the self is perceived, and they may aid in the development of a mechanistic understanding of therapy response.
Acknowledgments
Dr. Davey and Dr. Harrison were supported by NHMRC Career Development Fellowships (1061757 and 1124472, respectively). The authors thank R. Kerestes and K. Stephanou for their contributions to data collection, as well as staff from the Sunshine Hospital Medical Imaging Department (Western Health, Melbourne).