Deliberate self-harm is an important risk factor for subsequent suicide (
1,
2). Because one in seven adults who complete suicide have been treated for self-harm in the preceding year (
3,
4), suicide prevention commonly focuses on clinical management following self-harm events (
5,
6). Marked cross-national variation in underlying population rates of suicide (
7) as well as differences in study subject sampling contribute to differences in suicide risk following self-harm. In studies from other countries, the risk of suicide during the first year following self-harm varies from 0.8% to 3.0% for men and from 0.3% to 1.9% for women (
1,
2,
8–
10). In a study from a county in Minnesota, 1.9% (27 of 1,442) individuals who made nonfatal attempts died by suicide in the first year afterward (
11).
A few readily identifiable characteristics of self-harm patients have been linked to increased suicide risk. Suicide risk is greater for males than females (
12–
15) and for older than younger adults (
2,
7,
10,
15,
16). Compared with less violent self-harm methods, such as self-poisoning, more violent methods, such as firearms, have also been associated with a higher risk of subsequent suicide (
1,
10,
15,
17–
19), as has recent psychiatric hospitalization (
15), but whether this increased risk is concentrated within a specific interval after self-harm is unknown.
A key clinical challenge is to determine which self-harm patients have a particularly high risk of suicide during the first few weeks following the self-harm event. Because suicide has a low base rate, however, previous research has not included a sufficiently large number of patients to assess suicide risk factors over periods shorter than 1 year. As a result, there are currently no objective markers of short-term suicide risk following self-harm.
We examined repeat self-harm as well as suicide risk during the first year following self-harm among adults in the Medicaid program who were diagnosed with deliberate self-harm. Risk factors included demographic characteristics, recent treatment of common mental disorders, self-harm care setting, and self-harm method. Because the firearm suicide rate is eight times greater in the United States than in other high-income countries (
20), we specifically considered firearm-related self-harm events. In accord with previous research, we expected that male sex, older age, and violent methods would be related to higher suicide risk (
21). Because the suicide rate in the U.S. population is higher for white than black or Hispanic adults (
22), we anticipated that the risk of suicide following self-harm would also be greater for white than for black or Hispanic adults.
Method
Data Sources
The self-harm cohort was extracted from national Medicaid Analytic eXtract data from the Centers for Medicare and Medicaid Services (based on 45 states; data were unavailable for Arizona, Delaware, Nevada, Oregon, Rhode Island, and the District of Columbia) for the period 2001–2007. Dates and cause of death information were derived from linkage to the National Death Index, which provides a complete accounting of state-recorded deaths in the United States and is the most complete resource available for tracing mortality in national samples (
23). National Center for Health Statistics data were used to provide U.S. population suicide rates for 2001–2007 (
24).
Self-Harm Cohort Assembly
The cohort was restricted to adults 18–64 years of age with clinical diagnoses of deliberate self-harm (ICD-9 codes E950–958) excluding late effects (code E959) who were eligible for Medicaid services during the 180 days preceding the index self-harm event (see Table S1 in the data supplement that accompanies the online edition of this article).
The first eligible self-harm event was selected, and no patient contributed more than one observation to the cohort. The cohort was followed forward from the index date for 365 days, date of death from any cause, or end of available data, whichever came first. For deliberate self-harm events treated in outpatient or emergency department settings, the index date was the date of the deliberate self-harm treatment. For deliberate self-harm events treated on an inpatient basis, the index date was the date of hospital discharge from the associated inpatient admission.
Suicide
Consistent with the U.S. federal definition of suicide used by the Centers for Disease Control and Prevention, suicide was defined as deaths identified with ICD-10 codes X60–X84, Y87.0, or U03 (terrorism involving suicide) as the immediate cause of death in the National Death Index (
25). The primary outcome of interest was suicide after a nonfatal deliberate self-harm event. Fatal deliberate self-harm events were defined as suicides occurring during treatment episodes of the index self-harm event. In order to capture all suicides directly resulting from the index event, fatal events included suicide deaths on dates of service for events treated in outpatient and emergency settings and suicide deaths on the discharge date of events treated in inpatient settings.
Sociodemographic and Clinical Characteristics
Based on Medicaid eligibility data, cohort members were classified by age (into four categories: 18–34, 35–44, 45–54, and 55–64 years) at the time of the index self-harm event, by sex, and by race/ethnicity (white, non-Hispanic; black, non-Hispanic; and Hispanic). In addition to white race, the white group included American Indian/Alaska Native, Asian, Native Hawaiian/Other Pacific Islander, and more than one race. Cohort members were also classified by geographic region (West, Midwest, South, Northeast).
Variables representing mental health treatment on or within 180 days before the index self-harm event were used to characterize the occurrence of treatment of depressive disorders, substance use disorders, schizophrenia, bipolar disorder, anxiety disorders, personality disorders, and a residual group of other mental disorders (see Table S1 in the data supplement). At least one inpatient or two outpatient diagnoses defined each mental disorder group. A separate variable defined treatment for a substance use disorder and another mental disorder during this period. Separate variables defined any inpatient and outpatient mental health treatment and any treatment during the 180 days preceding the self-harm event.
The place of service code was used to classify the index self-harm event treatment setting as outpatient, emergency department, or inpatient. On the basis of ICD-9 codes, the method of self-harm for the index event was classified as violent, nonviolent, and other methods. Violent methods were subclassified as firearm-related methods and “other violent” methods, and nonviolent methods were subclassified as poisoning or cutting (see Table S1) (
26,
27).
Analysis
For self-harm patients who survived the initial event, we first determined, for each stratum of age, sex, race/ethnicity, and clinical variables, the number of patients, person-years of follow-up, number with one or more repeat self-harm events, and first repeat self-harm rates per 1,000 person-years of follow-up. We next compared the background characteristics of patients without repeat self-harm events, with repeat nonfatal self-harm events, and with suicide within 365 days of the initial event. We then compared the characteristics of three groups of suicide deaths within the first year: fatal initial events, suicides within 30 days of nonfatal events, and suicides within 31–365 days of nonfatal events. For the self-harm patients who survived the initial event, we then determined corresponding stratified rates of suicide risk per 100,000 person-years of follow-up. Cox proportional hazard models were used to determine unadjusted hazard ratios of repeat self-harm and suicide during the follow-up period with each stratification variable as the independent variable of interest. One model was then fitted including all background characteristics simultaneously to test independent effects. Separate models were also fitted for males and females. Kaplan-Meier cumulative risk curves were plotted for males and females, and the log-rank test was used to examine differences between the curves. A separate multinomial logistic regression model compared risk factors for the timing of suicide (no suicide, suicide in first 30 days, and suicide 31–365 days after the index event).
For comparison of suicide rates between the self-harm cohort (excluding initial fatal self-harm events) and U.S. population suicide rates, we determined the age-, sex-, and race/ethnicity-matched U.S. population annual mean suicide rates for 2001–2007. All statistical analyses were performed with SAS, version 9.4 (SAS Institute, Cary, N.C.).
Results
Patients With Nonfatal Initial Self-Harm Events
Most of the patients with nonfatal initial self-harm events were white, in the young adult age range (18–34 years), and female. The most commonly diagnosed psychiatric conditions were depression and alcohol use disorders; slightly less than one-quarter had received inpatient mental health care in the past 180 days. Compared with female patients, male patients were more likely to have diagnoses of schizophrenia or substance use disorders and less likely to have diagnoses of depressive, bipolar, anxiety, or personality disorders. Violent methods were more prevalent among male than female self-harm patients (see Table S2 in the online data supplement).
One-Year Repeated Nonfatal Self-Harm
In the self-harm cohort who did not complete suicide, 19.7% (12,012 of 61,054) or 263.2 per 1,000 persons-years were treated for repeated nonfatal self-harm during the follow-up year. The rate of repeat nonfatal self-harm was similar between men and women. The risk of repeat self-harm was higher for older than younger patients, and it was higher for white than black or Hispanic patients. Recent treatment for each of the specific mental disorders was also associated with a significantly higher risk of repeated self-harm. The risk of repeated self-harm did not differ significantly between patients who initially used violent methods and those who used nonviolent methods (
Table 1).
Repeated Nonfatal Self-Harm and Suicide
Compared with patients with repeat nonfatal self-harm events, patients who completed suicide during the follow-up period were more likely to be men and older adults and less likely to have black non-Hispanic race/ethnicity. Patients who completed suicide were also more likely than those with repeated nonfatal self-harm to have been treated in the emergency department and to have used a violent method, including specifically firearms, in their initial self-harm event (
Table 2).
Timing of Suicide Deaths
Compared to patients who had suicide deaths during the first 30 days (N=99) of follow-up and the following 335 days (N=144), patients whose initial self-harm events were fatal (N=189) were less likely to have been treated for depression, bipolar disorder, a personality disorder, or a substance use and other mental disorder, and they were less likely to have received inpatient mental health care in the 180 days preceding the initial event. However, they were significantly more likely than the other two groups to have used a violent method for the initial event. Although most adults whose initial self-harm event was fatal had received outpatient health care in the 180 days before their death (87.8%), only a minority (40.7%) had received outpatient
mental health care during this period (
Table 3).
One-Year Suicide Rates
During the first year following the index self-harm event, the suicide rate for the follow-up cohort was 439.1 per 100,000 person-years (
Table 4). The suicide rate of the age-, sex-, and race/ethnicity-matched U.S. general population was 11.8 per 100,000 person-years. The 1-year suicide rate for the follow-up cohort was therefore 37 times greater than the suicide rate in the general population.
Table 5 summarizes suicide rates by age, sex, and racial/ethnic group for the self-harm patients and the demographically matched general population.
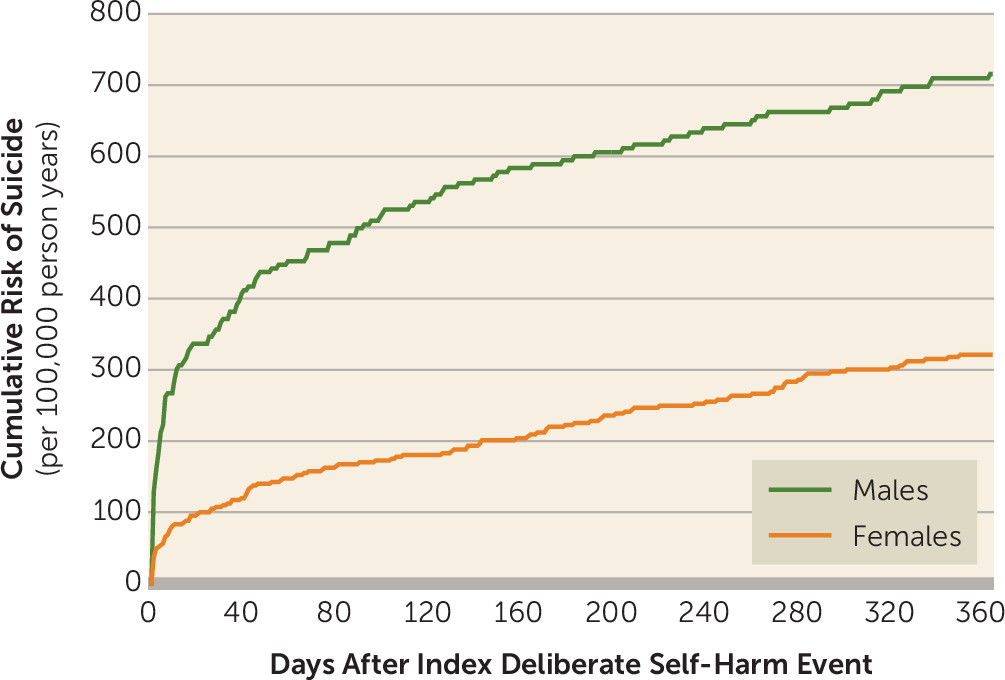
The crude 1-year suicide rate was more than twice as high for males as for females, and more than three times as high for older as for younger adults and for white adults as for black adults (
Table 4). The highest 1-year suicide rate, 5,822.3 per 100,000 person-years, or approximately 4.9% (31 of 633), was for patients who used firearms in their initial event. The cumulative 1-year risk of suicide following nonfatal self-harm was also significantly higher in males than in females, with a sharp increase in suicide risk among males during the first few days following initial self-harm (
Figure 1).
Suicide Following Nonfatal Events
Many patients who completed suicide in the year following their initial self-harm event used the same methods as they did in their initial event. This was especially true for self-harm events involving firearms (93.6%), other violent methods (87.0%), and poisoning (63.0%), but much less so for cutting (8.6%) (see Table S3 in the online data supplement).
Hazard of Suicide
In the adjusted Cox model, the hazard of suicide was significantly associated with older patient age, male sex, white as opposed to black race/ethnicity, treatment of self-harm event in an inpatient setting, and violent method of self-harm (see Table S4 in the data supplement). There were few differences in adjusted hazards of suicide between males and females, although recent inpatient mental health care and recent treatment of a drug use disorder were more strongly associated with suicide for females than for males (see Table S4).
Timing of Suicide Risk
Compared with use of nonviolent methods in self-harm events, use of violent methods was significantly more strongly related to suicide deaths during the first 30 days after the event (hazard ratio=17.5, 95% CI=11.2–27.3) (Table S5). This relationship was especially pronounced for self-harm events involving firearms. By contrast, patients whose self-harm events involved violent methods were not significantly more likely than those whose events involved nonviolent methods to die of suicide during the period from 31 to 365 days following the initial event (see Table S5 in the data supplement).
Discussion
Among self-harm patients, the 1-year suicide risk was 37 times higher than in the U.S. general population. Consistent with previous research from outside the United States, suicide risk was elevated for self-harm patients who used violent self-harm methods (
1,
10,
15–
19) and, to a lesser extent, for males and older adults (
1,
2,
8,
9,
12). In line with general U.S. population suicides rates (
22), the risk of suicide following self-harm was also higher for white than for black or Hispanic adults.
Fully two-thirds of suicides that occurred as a direct result of the initial self-harm event were attributable to violent methods, and over 40% of all initial suicide deaths were related to firearms. In accord with prior research (
18), surviving individuals who used violent as opposed to nonviolent methods were at increased risk for subsequent suicide. This risk was concentrated during the first month after the initial self-harm event. Among those who survived self-harm with violent methods, the risk of completing suicide over the following month was approximately 10 times greater than the risk over the subsequent 11 months. Moreover, if they survived the first 30 days after the initial event, they were not at significantly greater risk of suicide over the following 11 months than self-harm patients who used less violent methods. This risk pattern supports concerted efforts to protect patients who attempt suicide by highly lethal methods during the acute period after the self-harm event. During periods of extremely high risk, inpatient admission may facilitate crisis work, intensive supervision, and implementation of complex interventions, and it can help ensure patient safety. For patients who own firearms or live in homes with firearms, distributing trigger locks and urging family members to temporarily store household firearms away from the patient’s home (
28) can be a lifesaving intervention. Almost all of the suicide deaths following nonfatal firearm self-harm events were by firearms. In support of reducing access to firearms and other highly lethal means of suicide, previous research suggests that the self-harm methods people use depends to a significant degree on availability (
29) and that suicidal crises may be brief, sometimes lasting less than 1 hour (
30).
Our data show that the period immediately following self-harm events posed a high risk of suicide, especially for male patients. A Finnish study of patients who had been hospitalized for suicide attempts also reported that the suicide risk was highest during the first week following hospital discharge (
16), although that study did not separately assess risk in male and female patients. Clinical priority should be given to ensuring that these patients have prompt access to mental health services to facilitate clinical stabilization. One multinational study (
6) in low- and middle-income countries randomly assigned patients leaving emergency departments after suicide attempts to usual care or follow-up contacts focused on suicide risk prevention and referral. At 18-month follow-up, the intervention was associated with a significantly lower risk of suicide than usual care.
Among patients in our study whose initial self-harm events were fatal, most (87.8%) received some form of outpatient medical care during the 6 months preceding their event. A review of eight European studies using various methods similarly reported that, on average, 76.6% of individuals had at least one primary care visit in the year before suicide (
31). One strategy for engaging high-risk patients who do not present for specialty mental health care involves a health care system–wide approach that emphasizes cooperation and communication regarding care of suicidal patients across multiple levels of care (
32). However, suicide decedents are no more likely than matched comparison subjects to have any general health care contact during the preceding year (
33), and there is little evidence to suggest that screening tools can accurately identify suicide risk in primary care patients. A large number of identified low-risk patients could burden primary care physicians and mental health referral networks. Despite the high relative risk of suicide following deliberate self-harm, low absolute risk over the first year (1 in 228) complicates clinical suicide risk prediction. By contrast, approximately 1 in 5 patients repeated self-harm during that period, underscoring the importance of continuing mental health care for self-harm patients. Because of assessment challenges, the U.S. Preventive Services Task Force has determined that there is insufficient evidence to assess the balance of benefits and harms of routine screening of adult primary care patients for suicide risk (
34).
Among patients in our study whose initial self-harm event was fatal, only a minority (40.7%) received outpatient mental health care during the last 6 months of their lives. A review of 12 European studies reported a slightly lower average rate of mental health treatment (32%) in the year preceding suicide (
31). The large number of patients who do not receive mental health treatment prior to suicide constrains the overall effectiveness of mental health care–centered approaches to suicide prevention. Severely suicidal individuals who do not perceive a need for mental health treatment, or who conceal their suicidal plans, or who actively avoid specialty mental health care complicate suicide prevention. In a recent U.S. epidemiological study (
35), 43.7% of adults with past-year suicide attempts reported not having received any mental health care in the past year, and roughly three-quarters of them (one-third of all respondents with suicide attempts) did not perceive a need for mental health treatment.
Approximately 20% of the patients in our study repeated self-harm over the following year. This resembles the average 1-year percentage of repetition (18%) reported in a systematic review of 90 self-harm studies (
36). In accord with previous research, personality disorders and recent mental health treatment were associated with increased risk of repeated self-harm (
37). However, there was little difference in the risk of repeated self-harm between males and females, although male self-harm patients had a higher risk of suicide than corresponding female patients. This may be partly attributable to a tendency for men to use more lethal methods. Suicidal intent also tends to be greater among male than female self-harm patients (
38).
This study has several limitations. First, we have no means of validating the mental disorder diagnoses in the Medicaid claims data. Second, because of Medicaid eligibility rules, the study population included a disproportionately large number of adults with low incomes, individuals with disabilities, pregnant women, and women with dependent children. However, Medicaid is the single largest payer of mental health services in the United States (
39). Third, information was not available concerning several factors that are thought to increase suicide risk, such as hopelessness, problem-solving abilities, suicidal intent, recent stressful life events, and access to lethal means. In addition, community treatment, which may be more intensive and effective after severe or violent self-harm events, probably reduced the risk of suicide after many self-harm events. Fourth, stigma and misdiagnosis may have contributed to errors in the coding of deliberate self-harm and, together with low autopsy rates, to errors in the coding of suicide (
40). Fifth, our claims-based measure of deliberate self-harm does not capture self-harm events that do not result in medical care and does not distinguish self-harm injuries with suicidal from nonsuicidal intent. Sixth, it is not possible to determine the number of suicide deaths recorded on the date of hospital discharge that were a result of fatal reattempts during the inpatient stay or that occurred immediately after discharge. Finally, our data reflect suicide mortality patterns in the period 2001–2007, which may have changed in recent years, and a nonelderly adult population, which may not reflect risks in other age groups.