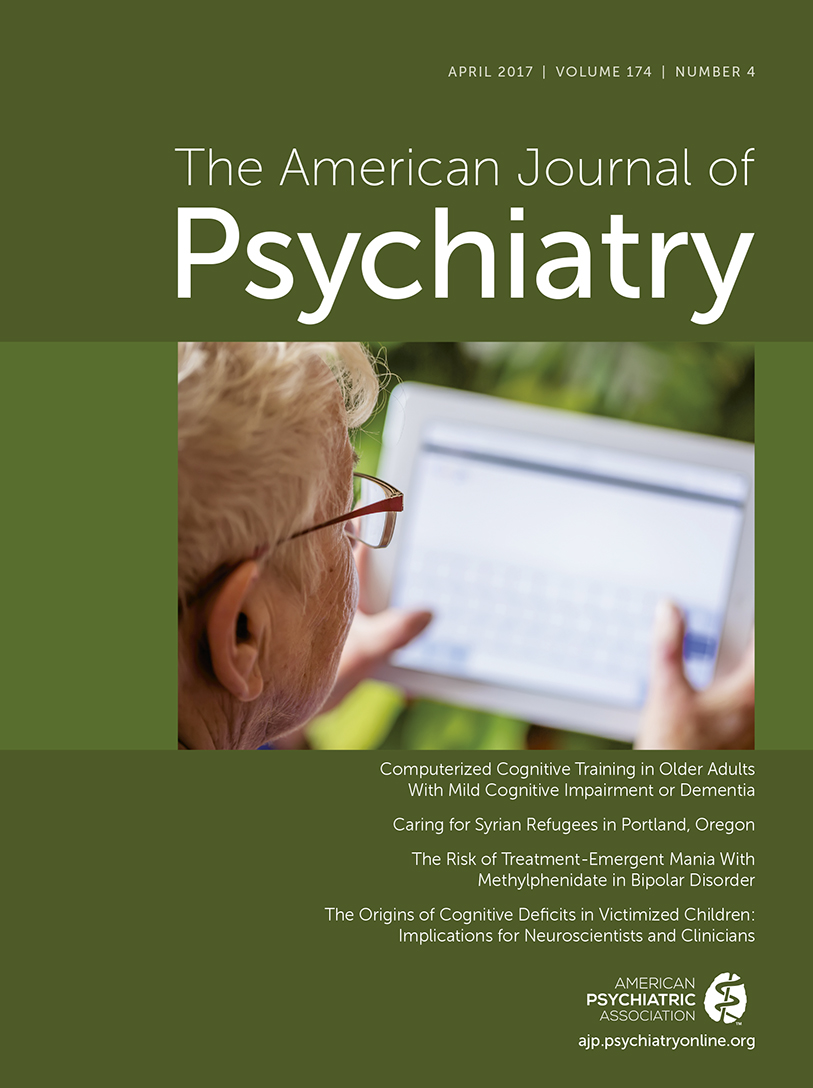
Global prevalence of dementia is currently 5%−7% of people >60 years old and projected to affect >115 million worldwide by 2050 (
1). Mild cognitive impairment is recognized as a proximal risk factor for dementia (
2), and so an important potential preventative strategy is therapeutic intervention targeting cognitive functions in individuals with mild cognitive impairment. In a review published in a previous issue of the
Journal, Keshavan et al. (
3) concluded that cognitive training offers “considerable promise” in the context of the treatment of mental disorders. An important question is whether computer-based cognitive therapy can assist in effective delivery of such training, and a new meta-analysis conducted by Hill et al. (
4) in the current issue of the
Journal, based crucially only on controlled clinical trial studies, provides encouraging support for this possibility.
In the past few years, several meta-analysis studies on the efficacy of computer-based cognitive training have been published both on the healthy aging population and on individuals with cognitive dysfunction. These meta-analyses have generally reported small to moderate effect sizes, although many studies included have been under-powered or lacking appropriate controls (
5,
6). In the excellent new meta-analysis published by Hill et al. (
4), they have focused exclusively on controlled clinical trials involving individuals >60 years old with mild cognitive impairment (17 studies, 686 participants) or dementia (12 studies, 389 participants) using computer-based cognitive training and including either active or passive control conditions. Studies mostly involved supervised training for at least 4 hours using drill-and-practice routines with a clear cognitive rationale or action video/virtual reality games. The meta-analysis reveals that for individuals with mild cognitive impairment, the overall effect size on cognitive outcomes is moderate (Hedge’s g=0.35), with no evidence of publication bias and no difference between active- and passive-controlled trials. Moderate effect sizes were found on general clinical measures and small or moderate effects on global cognition, verbal learning, verbal memory, nonverbal learning, working memory, attention, and psychosocial functioning. No significant effects on nonverbal memory, executive function, processing speed, language, visuospatial skills, or instrumental activities of daily living were found. While the authors concede that the lack of effect on executive functioning might be considered a drawback, given that this is a key component of cognitive dysfunction in mild cognitive impairment and other mental disorders, they point out that the training paradigms used by many studies included in their meta-analysis may not have been appropriate for enhancing executive function. For the dementia studies, while there was a small overall effect on cognitive outcomes (g=0.26), this was considered unreliable, since it was mainly driven by two studies with g>1 using virtual reality game approaches. Only four mild cognitive impairment and four dementia studies reported follow-up assessments with variable outcomes but mainly indicating weakening of effects over time.
The prevalence of computer and mobile telephone-based technologies worldwide and their popularity as entertainment, particularly in terms of interactive game playing, as well as communication and information devices, has led to their increasing use in a variety of e-learning contexts (
7). Claims of positive effects with commercial computer-based “brain-training” software are, however, often somewhat exaggerated and largely unsubstantiated (
8). Nevertheless, even general computer use may help reduce dementia risk (
9), and there is now increasing evidence suggesting that computer-based therapeutic tools can be used for treating cognitive decline not only in mild cognitive impairment (
4), but also following stroke (
10) and in psychiatric disorders such as depression (
11) and schizophrenia (
12).
Initial concerns about lack of computer skills in older individuals are becoming increasingly irrelevant with digital technologies now being widely used in all age groups. However, questions concerning whether computer-based training can be more effective than skilled therapists, which are the most effective training paradigms, and whether effects are long-lasting undoubtedly require more extensive research. Furthermore, an initial influential study demonstrating that specific skills learned during brain-training paradigms may not generalize (
13) raised issues about potential limitations for the utility of these approaches. However, subsequent research on the impact of virtual reality video games (see reference
14) or using strategy-based cognitive training (
15) has subsequently shown that learned effects can generalize beyond the context of a specific task.
Hill et al. (
4), in this issue of the
Journal, point out that for future studies to be sufficiently powered, group sizes >64 are indicated, which is considerably higher than the group sizes used in previous research. Caution is also required concerning potential placebo effects contributing to positive results, since even active controls do not necessarily avoid this pitfall (
16). Of fundamental importance going forward is to establish what is the most effective computer-based medium/strategy for producing generalizable, long-lasting beneficial effects across a wide range of cognitive functions, as well as the extent to which it can extend beyond use only under direct clinical supervision in the home environment where much longer periods of training are possible. These tasks/games must also be capable of being tailored to individual needs. The most widely used training approach gives subjects a series of individual tasks targeting different specific aspects of cognitive function, which can be tailored to specific individual ability in terms of initial difficulty. Several companies already provide commercial hardware and software versions with multiple tasks for use in a clinical rehabilitation setting, but their drawbacks tend to be that the graphics are often very simple and the tasks themselves repetitive and not particularly motivating. The cost of such systems can make them prohibitive for use outside of the clinic, which is also a limiting factor. An alternative approach is to tap into the expertise of the commercial gaming industry through exploiting the entertainment power of action video and virtual reality games (see reference
14) and additionally incorporating specific cognitive training elements and specialized in-built performance feedback indicators. This latter approach may ultimately offer the greatest potential not only in terms of helping prevent mild cognitive impairment from developing into dementia and restoring normal functioning, but also for treating cognitive dysfunction in individuals already with dementia. Several studies on the effects of action video games in healthy young adults have documented either structural (
17) or functional connectivity changes (
18) involving brain regions associated with cognitive function, and they could therefore also contribute to reduced risk of developing cognitive dysfunction through helping to increase cognitive reserve (
19). Importantly too, research using video games has reported successful and generalizable enhancement of executive function (see reference
14), and such games offer a greater possibility for affordable home-based use.
Undoubtedly, we still have a long way to go before research on computer-based cognitive therapy can realize its full potential. The inescapable reality, however, is that computer-based entertainment provides an incredibly powerful and pervasive medium, which, if appropriately harnessed, could achieve widespread therapeutic benefit. If properly researched and developed by clinicians, academia, and industry in collaboration, it could provide an unprecedented opportunity for guided self-help in preventing and treating mental disorders with cognitive dysfunction.