Alcohol consumption during pregnancy increases the risks of miscarriage, stillbirth, and a variety of physical and neurodevelopmental effects in offspring, collectively known as fetal alcohol spectrum disorders (
1). The World Health Organization (WHO) notes that “there is no safe level of alcohol use during pregnancy” (
2). WHO and the U.S. National Institute on Alcohol Abuse and Alcoholism have developed guidance for prevention or reduction of alcohol consumption during pregnancy to reduce alcohol-related harms due to prenatal exposure. However, while discouraged by much of the medical community and socially stigmatized in some environments, alcohol use during pregnancy persists.
In a national survey in the United States (
3), nearly 10% of pregnant women in the age range of 15–44 years reported alcohol use, with more than 2% reporting binge drinking; alcohol use was reported to be more common earlier in the pregnancy, and less common than among nonpregnant women. Attitudes toward alcohol consumption during pregnancy vary widely across Europe. In a multinational European study, 28.5% of U.K. women reported drinking during pregnancy, while Swedish women more closely resembled American women, with 7.2% continuing to drink (
4). Some evidence suggests that drinking during pregnancy is underreported (
5).
Although a nontrivial proportion of pregnant women continue to drink, the majority abstain, suggesting that pregnancy serves as a strong incentive to abstain from alcohol. During the economic recession of 2008–2009, when binge drinking prevalence increased overall in the United States, pregnancy was one of the strongest predictors of a decreased likelihood of binge drinking (
6). Even as past-30-day alcohol consumption and binge drinking have increased among nonpregnant U.S. women, these behaviors have decreased among pregnant women (
7). As noted in the context of prenatal illicit substance use (
8), women who misuse substances may be more likely to have an unplanned pregnancy (
9,
10), which would result in a positive association between pregnancy and alcohol misuse. However, the drive to protect one’s offspring from the adverse effects of alcohol is likely a counteracting factor, resulting in a negative association between pregnancy and alcohol misuse.
Drinking during pregnancy is associated with a variety of maternal characteristics. Swedish women with lower educational attainment, and those who live in smaller cities, are more likely to abstain during pregnancy (
4,
11). Those who smoked (
4) or exhibited heavier or more frequent drinking before pregnancy (
11–
13) reduced their drinking during pregnancy to a lesser degree than nonsmokers or light drinkers, respectively. Cognitive factors are also relevant. Women who report having used alcohol to enhance social interactions before pregnancy and those who perceived that small amounts of alcohol were not problematic were less likely to abstain (
13). In contrast, women who received a pamphlet detailing the negative effects of alcohol during pregnancy were more likely to reduce their drinking than those who received standard care (
14).
Alcohol consumption is distinct from, although correlated with, alcohol use disorder. Light or moderate, but nondependent, drinkers may abstain during pregnancy without undue effort. In contrast, problem drinking frequently involves motivational and volitional components, potentially because of neurobiological adaptations that reduce cognitive control over substance use (
15,
16). Indeed, the diagnostic criteria for alcohol use disorder include an inability to stop or reduce drinking despite one’s intentions and drinking for longer periods or in greater quantities than intended (
17). Thus, pregnancy may not be a sufficient incentive for women with alcohol use disorder to cease drinking. However, contingency management for alcohol use disorder—although used less commonly than for other substance use disorders (
18)—has demonstrated some success in increasing alcohol abstinence rates relative to standard care (
19–
21), suggesting that volitional capacity can be improved by extrinsic factors. Pregnancy is a qualitatively different motivator than the monetary incentives typically used in such programs. Rather than implicitly relying on immediate positive outcomes of monetary value to oneself, pregnancy-based motivation would rely on avoidance of distal negative outcomes for one’s offspring. This difference may mitigate the effectiveness of the “reward” (
22) and may be particularly relevant to alcohol use disorder, given its association with impulsivity and delay discounting (
23–
26).
Where pregnancy and alcohol misuse are negatively associated, it remains unclear whether this is due to a causal process or to other factors contributing to the coincidence of pregnancy and decreased alcohol misuse. In this study, we used Swedish national registries to investigate the potential causal association between pregnancy and alcohol use disorder. Although observational data preclude definitive conclusions about causality, we applied a range of analytic methods, in a statistically powerful sample, to clarify the nature of this association. First, we examined rates of alcohol use disorder in pregnant women relative to matched population-based control women. Second, given the prominent genetic influences on risk for alcohol use disorder (
27), we employed co-relative designs that enabled us to control for a degree of genetic liability while examining rates of alcohol use disorder in female relative pairs in which one member was pregnant and the other was not (i.e., discordant pairs). Third, we capitalized on the longitudinal nature of the registries to apply within-individual designs, comparing rates of alcohol use disorder registrations during pregnancy and nonpregnant time frames. Finally, we compared rates of alcohol use disorder in spouses before and during the pregnancy. Our study thus extends previous studies focused on alcohol consumption to address whether pregnancy may play a direct role in reduced incidence of alcohol use disorder.
Methods
Identification of Alcohol Use Disorder
We used several different Swedish population-based registers with national coverage, linking them with each person’s unique identification number, which was replaced by a serial number to preserve confidentiality. We secured ethical approval for the study from the Regional Ethical Review Board of Lund University (No. 2008/409). Alcohol use disorder was defined either by ICD codes for main and secondary diagnoses from Swedish medical registers (see the online supplement for a list of the ICD codes used) or by registrations of individuals in the Swedish Crime Register. Each individual could have several registrations in the criminal or medical registers. To avoid double-counting registrations, within each type of register (criminal and medical), we allowed for a 90-day period after each registration in which a new registration was not counted.
Sample
We selected all women born in Sweden between 1975 and 1992 who had at least one child registered in the Swedish multigenerational register for which the mother was likely first aware of being pregnant between the ages of 18 and 35. As in a previous study (
8), we estimated that women became aware of being pregnant 242 days before the birth.
Statistical Analysis
We matched each mother (N=322,029) to five unrelated control women (N=1,610,145) who had the same year and month of birth. The control women had to be alive and registered in Sweden at the time of the case subject’s pregnancy and not themselves registered as being mothers or having had a child within 9 months after the date of birth of the case subject’s child. For all control subjects, we examined alcohol use disorder during the same period as the case subject. We next replicated the matching approach but instead of using unrelated random individuals as controls, we matched on female cousins and full siblings, and we allowed for up to 3 years’ age difference between the case subject and the relative control subject. We matched 120,938 control cousins to 104,550 case subjects and 41,567 control siblings to 40,045 case subjects. By matching on cousins and siblings, we accounted for unmeasured genetic and environmental factors shared among cousins and siblings. Finally, we examined alcohol use disorder in a within-individual model comparing a 242-day period prior to the pregnancy to the pregnancy period.
We used conditional logistic regression, with a separate stratum for each case subject and their control(s), in which we compared alcohol use disorder in the case subject (i.e., alcohol use disorder during pregnancy) with alcohol use disorder in the control subjects (i.e., alcohol use disorder during a nonpregnant period). Model 1 was only a crude model, whereas in model 2 we adjusted for average parental educational (≤9 years, 10–11 years, ≥12 years) and school achievement of the individual (see reference
28 for how school achievement was defined). Odds ratios between 0 and 1 would indicate a reduced risk for alcohol use disorder during pregnancy (i.e., a protective effect of pregnancy), and odds ratios >1 would indicate an increased risk.
We then combined the population, full sibling, and cousin data sets and performed two co-relative analyses. The first allowed all coefficients for each sample to be independent. In the second, we modeled the genetic resemblance assuming that it equaled 0 for the population, 0.125 for cousins, and 0.5 for full siblings. We compared this model with the previous model, using Akaike’s information criterion, a model-fit statistic that balances goodness of fit and parsimony. If the second model fit the data well, we obtained improved estimation of the association between alcohol use disorder and pregnancy among all types of relatives. In this model we are also able to extrapolate an odds ratio for monozygotic twins (there were no monozygotic twins registered for alcohol use disorder while pregnant).
In additional analyses, we investigated whether the association between pregnancy and alcohol use disorder was moderated by the following variables: the average educational status across the individual’s parents; the individual’s school achievement; lifetime registration of alcohol use disorder in a parent of the mother (dichotomized as yes or no); alcohol use disorder registration of the individual prior to pregnancy; criminal registration of the individual prior to pregnancy (for a definition of criminal registration, see reference
29); drug abuse registration of the individual prior to pregnancy (for a definition of drug abuse, see reference
8); psychiatric registration of the individual prior to pregnancy; age at pregnancy (dichotomized as ≤25 years and >25 years); marital status (dichotomized as married or not married; in the analyses of married people, individuals who married during the control or hazard period were excluded); alcohol use disorder registration of the child’s father prior to pregnancy; and alcohol use disorder registration of the child’s father during pregnancy. These moderation analyses were performed only on the within-individual sample, using an interaction term (using the logit link) between the covariate of interest and the mother’s alcohol use disorder status. In the within-individual sample, we also tested whether the decrease in alcohol use disorder rates between control and pregnancy periods was the same for mothers and fathers. This was done by including an interaction term between a dummy variable indicating mother or father and alcohol use disorder status in mother and father.
Finally, we examined, using within-individual analyses only, the rates of alcohol use disorder in postpartum periods. Our control was the 242-day period prior to pregnancy, and we examined three 242-day postpartum risk periods: 0–242 days, 243–484 days, and 485–726 days after childbirth. We eliminated from these analyses mothers whose child died during the risk period. We included mothers who were no longer cohabiting with their child (the Ns were 1,088, 3,604, and 4,898, respectively, for the three postpartum risk periods) because these mothers had substantial elevations in rates of alcohol use disorder, suggesting that in some cases the child had been removed because of their problematic behavior. Excluding them would bias downward the postpartum alcohol use disorder rates.
In all these models, the within-individual and within-family clustering were taken into consideration. In models that included information on fathers, the father had to cohabit with the mother at the end of the year the child was born. All statistical analyses were performed using SAS, version 9.3 (SAS Institute, Cary, N.C.).
Results
Association Between Pregnancy and Alcohol Use Disorder Registration
Rates of alcohol use disorder among pregnant women were considerably lower than among matched control women (odds ratio=0.32, 95% CI=0.27, 0.37) (
Table 1). This association became stronger (that is, the odds ratio was closer to 0) after controlling for mean parental education and school achievement. These findings corresponded closely to the negative association between pregnancy and alcohol use disorder among cousins discordant for pregnancy (odds ratio=0.31, 95% CI=0.23, 0.42); similarly, accounting for potential confounders strengthened the observed association. When comparing alcohol use disorder rates in pregnant women and their discordant biological full sisters, the negative association was even more pronounced (odds ratio=0.22, 95% CI=0.13, 0.36).
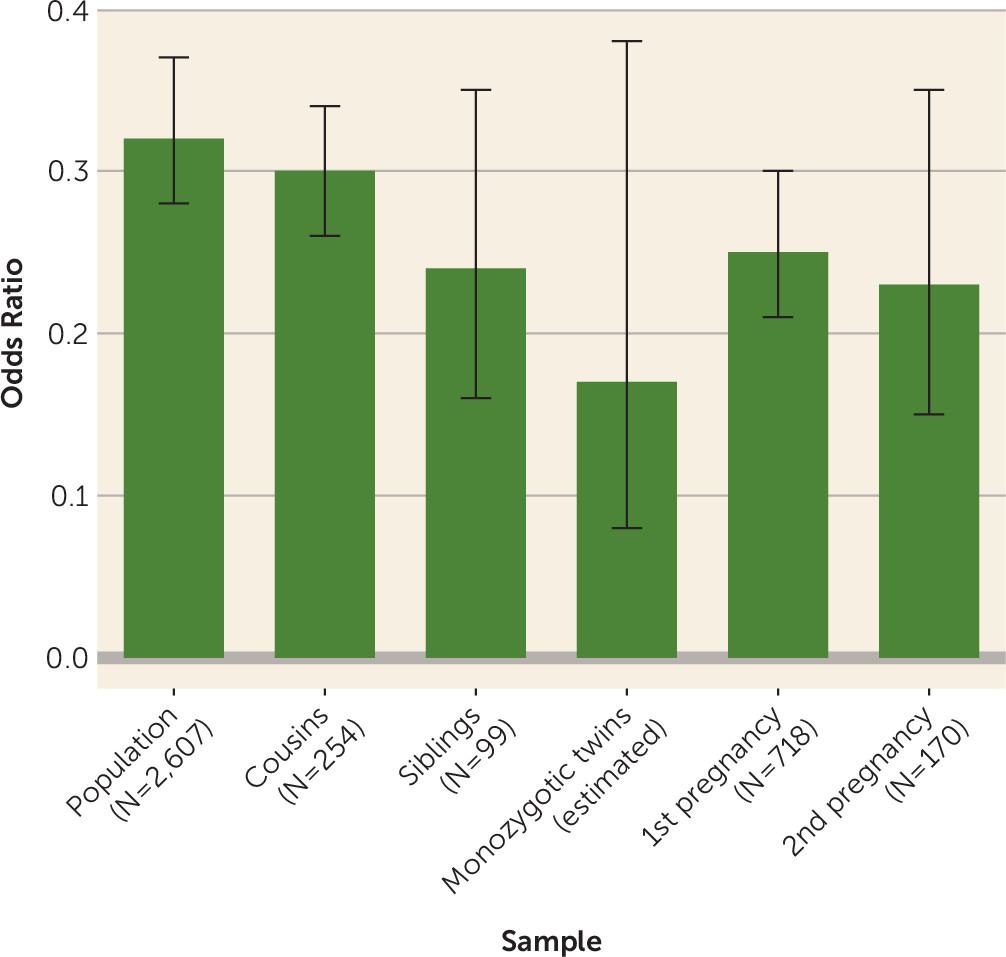
We used unadjusted results from the discordant cousin and sibling analyses to fit a co-relative model, extending to estimated odds ratios for discordant monozygotic twins. As shown in
Table 2, the estimated odds ratios decline monotonically, from 0.32 to 0.17, as a function of relatedness. These findings are illustrated in
Figure 1. The fit of the predicted model is superior to that of the observed model, as indicated by a lower Akaike’s information criterion value (
Table 2).
We conducted a series of within-individual analyses, first using periods prior to pregnancy as the control. Regardless of the control time frame—the 242 days prior to the estimated beginning of the pregnancy, 6 months prior to start of pregnancy, or 12 months prior to start of pregnancy—the risk of alcohol use disorder was consistently and substantially reduced during pregnancy (odds ratios, 0.25–0.26) (
Table 1). We next tested whether rates of alcohol use disorder were similar in the first and second halves of a pregnancy, and found no significant difference (odds ratio=1.08, 95% CI=0.78, 1.49). We also examined whether the negative association was observed during a second pregnancy, and obtained comparable results (odds ratio=0.23, 95% CI=0.15, 0.35) (
Table 1). Finally, we examined the persistence of the observed negative association during a range of postpartum periods (
Table 3). We found a gradual decrease in the protective effect of pregnancy across time, with the prevalence of alcohol use disorder in the immediate postpartum period (0–242 days after childbirth) only half that in the third period (485–726 days after childbirth). Even so, the confidence intervals for the odds ratios in the third period remained far below one.
Comparison With Fathers
We tested whether a similar association was observed among biological fathers, using the 287,292 cases where the father and mother were cohabitating at the end of the child’s year of birth. When examined together, the reduction in risk for an alcohol use disorder registration from the control to the pregnancy period was more pronounced for the mother (odds ratio=0.18, 95% CI=0.14, 0.23) than for the father (odds ratio=0.45, 95% CI=0.41, 0.49). This difference was also reflected in a model that treats mothers and fathers as independent: the reduction in risk in the control period compared with the pregnancy period was stronger in the mother relative to the father (odds ratio=0.56, 95% CI=0.47, 0.68).
Potential Moderating Factors
We considered a range of sociodemographic and psychopathological factors that may moderate the negative association between pregnancy and alcohol use disorder (
Table 4). We observed evidence of moderation (p<0.05) for only two factors: a criminal registration in the mother prior to pregnancy and age at pregnancy (<25 years or ≥25 years). Specifically, the negative association between pregnancy and alcohol use disorder was stronger among mothers with a criminal history relative to their counterparts without a criminal history; similarly, the negative association was more pronounced among younger mothers.
Discussion
We used national registry data to examine the potential causal relationship between pregnancy and reduced risk for alcohol use disorder among Swedish women. We considered a variety of contextual perspectives: matching to population controls, comparison with female relatives discordant for pregnancy, within-individual control periods, and comparisons between mothers and fathers. We consistently observed markedly lower rates of alcohol use disorder registrations during pregnancy, with the reduction in risk among mothers ranging from ∼70% to 80% across analyses. The findings are suggestive of “inverse confounding,” such that adjustment for potential sociodemographic or genetic confounders strengthened the observed association. These results are consistent with previous reports that women reduce their alcohol consumption during pregnancy (
6,
30,
31). We extend those findings to demonstrate that the observed association applies to a clinically relevant outcome, indicating that even among women at elevated genetic risk for or with a personal history of alcohol use disorder, pregnancy can be a critical motivating factor for modifying alcohol misuse.
We first compared pregnant women with matched control women and, accounting for covariates, found that the odds of an alcohol use disorder registration were reduced by 74% among pregnant women. When controlling for confounding factors by applying a co-relative design, we found that pregnancy was even more strongly protective against risk for alcohol use disorder, with the odds of alcohol use disorder reduced by 83% in the pregnant member of a discordant monozygotic twin pair. While the unique nature of pregnancy precludes comparison with other circumstances in which changes to drinking are expected (e.g., contingency management programs), these reductions are objectively substantial. Notably, previous studies have demonstrated that clear communication from clinicians, such as provision of a pamphlet or interpersonal discussions about the risks of prenatal alcohol use, may further reduce alcohol misuse, beyond the effects of pregnancy alone (
13,
14). Pregnancy may therefore present an important window of opportunity for intervention (
32).
Longitudinal data and the temporally discrete nature of pregnancy enabled us to use women as their own controls, comparing rates of alcohol use disorder during pregnancy and during periods preceding and following pregnancy. This approach is not subject to potential confounders that may complicate observed associations between pregnancy and alcohol use disorder. Given that many pregnancies are planned and women may modify their alcohol use in anticipation, we used a range of time frames as the reference; the quite stable results suggest that even if pregnancy is planned 6 to 12 months in advance, the actual pregnancy still represents a period of substantial reduction in risk of alcohol use disorder. This relationship was borne out in the postpartum periods as well. In the period immediately following pregnancy, the odds of alcohol use disorder were identical to those predicted for discordant monozygotic twins. In the next two successive periods, the odds increased but remained substantially lower than 1. Thus, the protective effect potentially conferred by pregnancy persists over time, with only minor decreases in strength; additional analyses could clarify the extent to which risk stabilizes. Previous work indicates that parenthood itself is inversely associated with risk of alcohol use disorder (
33,
34), and thus long-term decreases in risk relative to the prepregnancy period are likely.
We evaluated potential moderation of the association of pregnancy and alcohol use disorder by a variety of factors. We found that the risk of alcohol use disorder decreased during pregnancy more sharply among women with a history of criminal behavior. Similarly, women who became pregnant before age 25 exhibited a more pronounced reduction in risk of alcohol use disorder than those who became pregnant at a later age. These findings suggest that pregnancy may be an especially powerful motivator for healthful behavior among women who are otherwise at higher risk for alcohol use disorder. Interestingly, we observed no interaction between pregnancy and personal history of alcohol use disorder. Parental history of alcohol use disorder, an indicator of genetic and environmental alcohol use disorder risk, also did not moderate the association between pregnancy and alcohol use disorder. In conjunction with our co-relative analyses, this suggests that while genetic factors may inversely confound the observed association, the protective effect of pregnancy is robust even to the pronounced genetic component of alcohol use disorder liability. Indeed, the paucity of moderating factors underscores the consistency of pregnancy’s motivational capacity.
Pregnancy is also associated with reductions in alcohol use disorder among partners, although to a lesser extent than among mothers. Again, this suggests that factors other than fetal alcohol exposure contribute to the observed association; a previous study found that changing social contexts and concern for the mother motivated decreased alcohol consumption among the partners of pregnant women (
35). The discrepancy in risk reduction across mothers and fathers may be attributable to concerns about alcohol’s direct effect on the fetus: Brief interventions that educate pregnant women about alcohol’s teratogenic effects have been shown to decrease consumption (
14,
36). Notably, partner alcohol use disorder, prior to or during the pregnancy, did not moderate mothers’ alcohol use disorder risk. A Dutch study of pregnant women found that women drank less if their partner more strongly disapproved of drinking during pregnancy or if the partner drank less during the pregnancy (
37). Taking these findings together, it is possible that health-promoting partner behavior may discourage adverse outcomes in the mother, while the inverse may not be true: pregnant woman are unlikely to be differentially affected by “risky” partner behavior.
We note a number of limitations to this study. Our analyses were conducted on native-born Swedes and may not generalize to other populations; while we have no reason to believe that Swedish women are substantially different from women in other industrialized countries, the social resources available to pregnant Swedish women may facilitate decreases in alcohol misuse. We selected a birth cohort to maximize data availability during the time frame relevant to childbirth; this may come at the expense of detecting long-term changes in rates of alcohol use disorder, or specifically changes in the association between alcohol use disorder and pregnancy. Our use of registry data may be more likely to capture more severe cases of alcohol use disorder and therefore may be subject to false negatives; however, false negatives are a pitfall of nearly any study design, and registry records are less subject to recall or reporting bias than self-reports. The reliance on registry records also precludes examination of intra- or interpersonal factors, such as personality, motives for changes in alcohol use or misuse, quality of the relationship with one’s partner, and so on.
In summary, these findings suggest that pregnancy plays a pivotal motivational role in the reduction of alcohol use disorder. Our results are consistent with a causal role for pregnancy in alcohol use disorder risk reduction, although this should not be considered definitive, given the observational nature of the data. Negative associations were strong and consistent across all analyses and, overall, were robust to moderation by an array of factors that are otherwise reliable predictors of risk of alcohol use disorder. Both parents benefit from the reduction in alcohol use disorder risk during the pregnancy, with the association more pronounced for mothers, among whom it persists, with modest attenuation, into the postpartum period. In conjunction with evidence from alcohol use disorder treatment programs that include cash or prize rewards for abstinence, this putative protective role of pregnancy suggests that qualitatively different factors have the potential to motivate reduction in alcohol misuse, which may broaden the possibilities for intervention in alcohol use disorder treatment. These findings further suggest that the reduction in volition often associated with substance use disorders may be superseded by especially salient circumstances.
Acknowledgments
The authors thank the Swedish Twin Registry at the Karolinska Institute, which provided the twin data for this study.