Substance use disorders are common, with general population prevalence estimates between 8% and 10%, or over 21 million adults in the United States (
1), and annual health care costs in excess of $120 billion (
2,
3). Average life expectancy in the United States fell from 78.7 to 78.6 years between 2016 and 2017, with the decrease primarily attributable to increases in suicide and drug overdose (
4). Several articles in this issue of the
Journal report on studies using state-of-the-art tools and techniques to shed light on various aspects of substance use disorders. A better understanding of substance use disorders can improve prevention and treatment efforts and is critical to public health.
This issue contains two very interesting investigations of important aspects of adolescent substance use disorders. The connection between psychosocial stress, childhood adversity, and the development of substance use disorders is well established (
5). With the growth in scientific techniques that allow exploration of genetics and epigenetics, it is becoming possible to delineate the biological changes involved in this stress–substance use relationship, which is what Tay and colleagues have done (
6). In a study of over 1,200 adolescents, the authors found that hypermethylation of the ETS transcription factor (SPDEF) locus was associated with a greater number of stressful life events. Among individuals with the minor G allele, methylation moderated the association between psychosocial stress and substance abuse. In addition to demonstrating that methylation of a novel site was associated with stressful life events in this group of adolescents, a gene-by-environment interaction was found, indicating that the level of methylation was dependent on both genotype and stress exposure, which is consistent with what we know clinically about differential susceptibility to the impact of stress. Better understanding of the biological mechanisms underlying the impact of stress on substance use disorders will provide direction for intervention and prevention efforts.
The recent explosion of laws in the United States and Canada legalizing the recreational use of marijuana makes the study by Morin and colleagues (
7) particularly timely. In this population-based study, seventh-grade students in the Greater Montreal region were assessed annually for 4 years for alcohol and cannabis use and on cognitive tasks, including recall and working memory, perceptual reasoning, and inhibition. Cannabis use, but not alcohol use, demonstrated effects on inhibitory control, working and delayed memory recall, and perceptual reasoning. While basic science studies suggest an impact of cannabis on brain development (
8), and a number of studies have demonstrated the impact of cannabis use on cognitive function in adults (
9), this carefully executed study demonstrates the longitudinal impact of cannabis on cognitive function in adolescents. This is of critical importance because failure to learn in school, even for short periods, can interfere with subsequent capacity to achieve educational goals, leading to poor life achievement. Cannabis use affects functional connectivity of the brain (
10), particularly if use starts in adolescence or young adulthood, which may help explain the association between frequent use of cannabis from adolescence into adulthood and significant declines in IQ (
11).
Lower brain volumes have consistently been observed in individuals with substance use disorders, but data concerning specific brain regions have not been consistent across studies or substances. Mackey and colleagues (
12) pooled data from 23 laboratories in 14 countries to examine brain structure in over 2,000 individuals with dependence on alcohol, nicotine, cocaine, methamphetamine, or cannabis compared with a nondependent control group. While lower volume or thickness was found across substances in many brain regions, the insula and medial orbitofrontal cortex were the two areas most affected across substances. Comparing substances, the authors found that the most profound effects were in alcohol use disorders. Support vector machine multivariate classification of regional brain volumes successfully classified individuals with alcohol or nicotine dependence relative to nondependent control subjects. While the authors suggest that these differential patterns could serve as useful biomarkers of dependence on alcohol and nicotine, further exploration of the stability of these changes over time and their relationship to abstinence and active use would be important in delineating their utility as a potential biomarker.
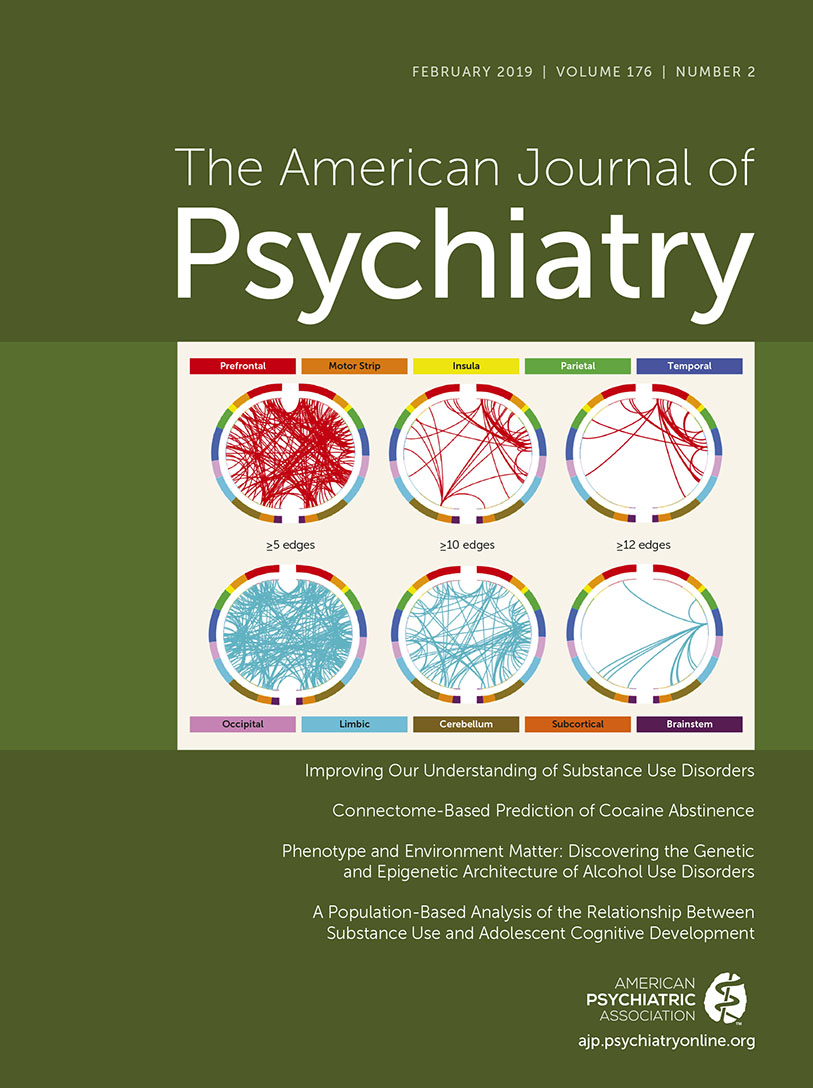
In this regard, the article by Yip and colleagues (
13) is of particular interest. Using connectome-based predictive modeling, an innovative machine learning approach to image analysis that generates whole-brain functional connectivity data (“connectomes”), the authors analyzed scans of cocaine-dependent individuals at the beginning and end of a 12-week treatment period. Neural networks identified at treatment entry were assessed for association with abstinence immediately following treatment and at 6-month follow-up. Not surprisingly, individuals able to achieve abstinence demonstrated greater integration of the cognitive/executive control system (with connectivity between frontoparietal and medial frontal networks) and integration of a reward responsiveness system (with increased connectivity between salience, motor/sensory, and subcortical networks). Within this context, cognitive/executive control networks likely contribute to abstinence via coordination of top-down processes (e.g., skills development, improved impulse control), while reward network integration supports motivational processes relevant to treatment (e.g., attention to alternate rewards). Of interest, connectivity strength did not change with treatment. The authors speculate that this information may be useful in the identification of targets for treatment intervention; however, exploration of the ability of substance use treatments to alter connectivity and the relationship between altered connectivity and abstinence is needed. Theoretically, cognitive-behavioral therapies should improve “top-down” control, whereas interventions involving contingency management should affect the salience/reward networks. In addition, further exploration of cognitive remediation strategies in the treatment of substance use disorders could be fruitful.
In an interesting study exploring pharmacologic treatments, Sullivan and colleagues (
14) present a well-designed study comparing different formulations of the opioid antagonist naltrexone. Once-daily administration of oral naltrexone was compared with once-per-month administration of extended-release injectable naltrexone in individuals with opioid use disorders. Significantly more patients were retained in the extended-release injectable naltrexone group, suggesting that having an antagonist “on board,” alleviating the daily decision to take medications, may help in relapse prevention. Relapse is often associated with impulsive decision making, environmental cues, and stressful life events. A long-acting antagonist may give an individual an opportunity to extinguish the learned association between environmental and internal cues and drug use. Several recent studies have demonstrated comparable efficacy of extended-release injectable naltrexone compared with buprenorphine (
15,
16), but this is the first study to compare the shorter-acting oral formulation with extended-release injectable naltrexone. In these studies, dropout rates were higher in the extended-release injectable naltrexone group during the induction phase, as individuals must undergo complete detoxification before extended-release injectable naltrexone can be initiated, but individuals who were successfully inducted reported less craving than the buprenorphine group. These studies suggest a clear role for antagonist therapy in opioid use disorders, but improved procedures for successful induction are needed.
In another article in this issue, Edwards and colleagues (
17) used longitudinal data from population-wide Swedish medical, pharmacy, and criminal records to evaluate rates of alcohol use disorder during pregnancy, conducting comparisons between pregnant women and matched control subjects as well as individual pre- and postpregnancy comparisons. Pregnancy was inversely associated with alcohol use disorder across all analyses. This research group previously conducted a similar analysis exploring drug abuse during pregnancy, with similar results: pregnancy was inversely associated with drug use (
18). Although concern for the health of offspring likely plays a major motivating role, when one considers the uniformity of this finding—regardless of family history or level of addiction—and the importance of abstinence during pregnancy to successful survival of the species, biological changes during pregnancy such as hormonal fluctuation could also play a role in this dramatic decrease in substance use. Further exploration of this robust phenomenon could provide useful information to guide the development of new treatments. In addition, interventions targeting maintenance of pregnancy-related gains in abstinence during the postpartum period should be explored. Considering the schedule disruption and stress often associated with the postpartum period, this area warrants attention.
Finally, using genome-wide association analysis of population-based cohorts, Sanchez-Roige and colleagues (
19) demonstrate that alcohol consumption and alcohol-based problems show significantly different patterns of association across a number of traits, including psychiatric disorders. While scores for alcohol-based problems were highly genetically correlated with schizophrenia, major depression, and attention deficit hyperactivity disorder (ADHD), alcohol consumption scores were negatively genetically correlated with major depression and ADHD. This finding demonstrates, once again, the close connections between substance use disorders and other psychiatric disorders and the value of understanding the connection between the two in driving the field forward.
Problems related to substance use disorders are a major public health concern, with daily headlines about opioid overdose and the changing landscape in marijuana regulation affecting access and attitudes. Research provides critical information to guide clinical practice and shape the appropriate public health response to these pressing issues.