In 2018, the APA Joint Reference Committee voted to approve a Resource Document developed by the APA Council on Consultation-Liaison Psychiatry’s Work Group on QTc Prolongation and Psychotropic Medications. The Work Group had been charged to develop a set of clinical considerations to guide psychiatrists on best practice prescription and monitoring of psychotropic medications that may prolong the QTc interval or increase the risk of torsades de pointes. The Resource Document was supported by and received the official endorsement of the American College of Cardiology. The following summarizes the Work Group report.
Over the past decade, there has been increased attention from the medical community about the role of QTc monitoring in the prescription of psychotropic medications. Psychiatrists frequently prescribe psychotropic drugs that may prolong cardiac repolarization, thereby increasing the risk for torsades de pointes (TdP), a potentially fatal cardiac arrhythmia. The corrected QT interval (QTc) on the electrocardiogram (ECG) is the most widely used and accepted marker of TdP risk by drug safety boards; however, there is not unanimity in the guidelines and warnings among the Food and Drug Administration (FDA) in the United States and analogous bodies in other countries. There is a paucity of strong evidence to guide clinicians, and to date there are no practice guidelines endorsed by the American Psychiatric Association (APA) or the American College of Cardiology (ACC). This resource document is not intended to be a practice guideline, rather an educational tool for clinicians to use when prescribing psychotropic medications.
Well-established risk factors for TdP include medications that prolong cardiac repolarization, bradycardia, female sex, increased age, hypokalemia, hypomagnesemia, congenital long-QT syndrome, personal history of structural heart disease, previous history of acquired QTc-prolongation, family history of sudden cardiac death, concurrent use of other QTc-prolonging medications, pharmacodynamic and pharmacokinetic drug interactions, drug toxicity, hepatic and/or renal dysfunction, and acute illness. It is essential to be aware of these risk factors to assess and monitor patients accordingly if a drug with a risk to prolong QTc interval is being considered or prescribed.
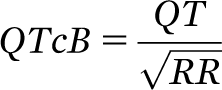
The duration of the QT interval varies depending upon the heart rate, and the QT interval needs to be “corrected” (QTc) for heart rate to make it more consistent and clinically meaningful. Several different formulae have been established to correct the QT interval for heart rate. It is important to recognize there is a lack of consensus as to which technique is optimal, and none are perfect. Bazett's formula
is the most common method used to correct QT interval for heart rate. However, a major limitation of Bazett's formula is that it overestimates QTc interval at heart rates higher than 60 beats per minute (bpm) and underestimates at rates lower than 60 bpm. The International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH) recently identified it as “an inferior method” and recommended using Fridericia’s formula
which is less influenced by extremes of HR.
In resource-poor settings, ECGs may not be easily accessible. Practitioners should not let the absence of an ECG preclude the prescription of a psychotropic medication; rather they must carefully consider known risks versus benefits of prescribing the medication. In settings where clinicians have access to an ECG machine in the absence of a cardiologist to read and interpret, clinicians of any medical specialty should feel comfortable with measurement, calculation, and documentation of the QTc.
Patients in the ICU setting are at increased risk of TdP given the very nature of having severe medical/surgical illness. It is essential for all members of the ICU team, psychiatry, cardiology, and other specialty services to work collaboratively and broadly to stratify and mitigate risk. An important risk/benefit consideration is the risk of not appropriately controlling agitation, which may result in harm to patient via self-removal of external devices. The intensive care unit should be considered the “safest” place in the hospital where patients are closely monitored, and staff are equipped to rapidly manage potential arrhythmias.
Routine cardiology consultation is not indicated when prescribing QTc prolonging medications to a patient without cardiac risk factors; however, many higher-risk clinical scenarios are best approached with cardiology input. In patients with known heart disease and one or more risk factors for drug-induced torsades, the clinician may consider consulting with the existing cardiologist when starting a medication with liability. In higher risk scenarios—including coadministration of high-risk medications (e.g. amiodarone and parenteral haloperidol), marked QTc prolongation (>500 msec), or a sudden increase of QTc (>60 msec from baseline)—referral to cardiology is appropriate. Patients on a known offending drug who experience cardiac symptoms such as syncope, dizziness, and palpitations should immediately be referred to cardiology. When prescribing medications known to increase risk of TdP to patients with a Cardiac Implantable Electronic Device (i.e. pacemaker or implantable cardioverter defibrillator), the clinician should not assume that the patient is “protected,” rather the presence of a cardiac device should trigger increased vigilance.
The practitioner caring for pediatric patients may wish to consult with a local cardiologist with the experience or training to deal with the complex issues present in the pediatric population. Given the limitations in the literature, as well as complexities related to categorizing risk in children and adolescents, making broad recommendations regarding the assessment and minimization of QTc prolongation in pediatric populations is beyond the scope of this resource document.
When reviewing studies on QTc prolongation and psychotropic medications, clinicians must understand the inherent limitations of available data and how this may impact guidance provided by regulatory agencies. For example, QT interval changes in the range of 10–20 msec, as found in the FDA citalopram studies, are below the limits of detection on an individual ECG and may only yield a signal in large samples. Clinicians should approach the decision to prescribe a psychotropic with known risk of QTc prolongation using a comprehensive risk-benefit analysis, including, but not limited to, the baseline QTc, comorbid conditions, as well as the risk of failure to adequately treat the presenting psychopathology.
The full Resource Document, which includes a comprehensive review of the literature and individual medications, is available in a
data supplement that accompanies the online version of this APA Official Action in the March 2020 issue of
The American Journal of Psychiatry (
ajp.psychiatryonline.org). The findings, opinions, and conclusions of this Resource Document do not necessarily represent the views of the officers, trustees, or all members of the American Psychiatric Association and do not represent APA policy.