Most psychiatric illnesses have their onset early in life, and many of them are hypothesized to be disorders of neurodevelopment. Because of the importance of development to psychiatry, this issue of the Journal is focused on new findings relevant to factors that are involved in the childhood and adolescent expression of psychopathology. As behavioral neuroscience moves forward, numerous findings from preclinical and clinical studies have emerged that emphasize the genetic and environmental factors that converge to result in illness vulnerability. In this issue, we learn about new findings relevant to the genetics of childhood-onset illnesses such as Tourette’s syndrome and attention deficit hyperactivity disorder (ADHD). We also learn about factors related to the within-family, nongenetic transmission of substance abuse, as well as early-life predictors of adolescent self-harm as it relates to violent crime.
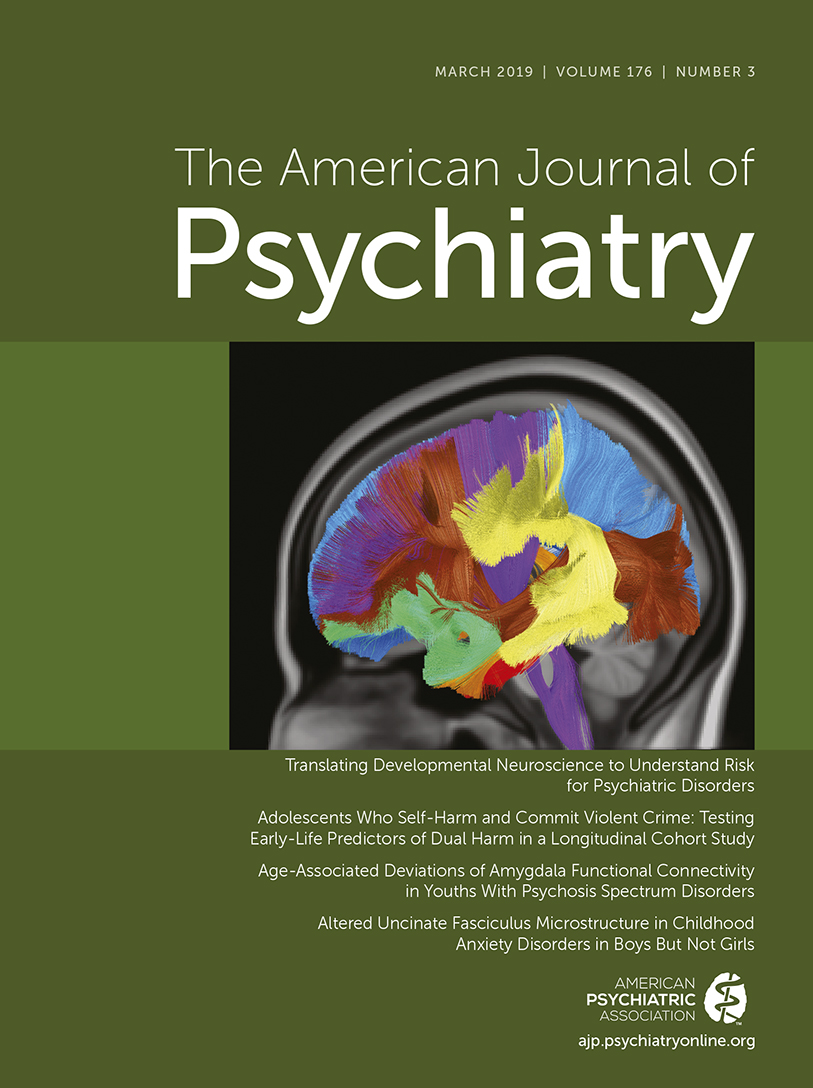
This issue begins with an overview by Drs. Heidi Meyer and Francis Lee that puts into perspective how findings from developmental neuroscience have informed our understanding of the early-life factors that confer risk for the development of psychiatric disorders. Dr. Lee is a leading clinician-scientist focusing on basic mechanisms linking neurodevelopment to psychopathology, and Dr. Meyer is a postdoctoral trainee in his laboratory. Their overview provides a framework for the importance of understanding the effects of environmental events during childhood and adolescence on the developmental trajectories of neural circuits that underlie cognition, motivation, and emotion regulation. Drs. Meyer and Lee also discuss two articles in this issue that are relevant to altered development of neural circuits that underlie emotion regulation and cognition. The article by Jalbrzikowski et al., studying youths with psychotic spectrum disorders, presents data suggesting that these individuals have alterations in the normative adolescent developmental trajectory of amygdala functional connectivity. The article by Tromp et al. addresses early-life mechanisms that may underlie alterations in prefrontal-subcortical connectivity associated with anxiety disorders by demonstrating diminished microstructural integrity in the uncinate fasciculus in preadolescent boys with anxiety disorders.
Two other articles in this issue directly address the genetic underpinnings of childhood-onset psychiatric illnesses: 1) Tourette’s syndrome and other tic disorders and 2) volumetric brain alterations that are associated with ADHD. In the article by Yu et al. and the Psychiatric Genomics Consortium Tourette Syndrome Workgroup, findings are presented from a genome-wide association meta-analysis representing the largest sample studied to date. The findings point to some shared genetics between tic disorders and Tourette’s syndrome and suggest that across these disorders, symptom severity is associated with a computed polygenic risk score. Interestingly, the dorsolateral prefrontal cortex, a region of the brain known to be involved with executive function, was found to preferentially express the identified risk genes. In relation to ADHD, research demonstrates reductions in total and subcortical regional brain volume that are associated with the illness. In this issue, the article by Klein et al. provides insights into this brain alteration by demonstrating a genetic correlation between reductions in total brain volume with ADHD risk. This suggests that these two features share similar genetic underpinnings. This work also identifies specific genes that may be important to the shared genetics between brain volume and ADHD risk, suggesting leads for further studies focused on mechanisms underlying ADHD-related decreases in brain volume.
Moving away from genes to psychosocial influences, Kendler et al. demonstrate that nongenetic contagion factors are important in the development and “transmission” of drug abuse. This study capitalizes on a large Swedish cohort by focusing analyses on the timing of the development of drug abuse among related family members. This design allows for the control of genetic influences. The findings demonstrate that the likelihood of drug abuse transmission is greater from parent to child (adolescent to early adulthood years), from older sibling to younger sibling, and greater in closer compared with more distant relatives. Taken together, and beyond genetic risk, these findings highlight the potential importance of within-family patterns of substance abuse and the social learning that may take place in relation to its intrafamilial transmission.
Substance dependence, childhood victimization, and higher rates of psychotic symptoms are factors that we learn, from the paper by Richmond-Rakerd et al., are associated with adolescents who engage in “dual-harm” behavior. These individuals not only engage in self-harm behavior but also have committed violent crimes. Notably, the findings from this work demonstrate that self-harm is associated with a marked increase in the likelihood of committing violent crimes, and the findings importantly underscore the need for early interventions focused on mitigating the influences of the risk factors identified in this study.
Taken together, the articles in this issue of the Journal underscore the importance of studying early development at multiple levels to better understand mechanisms that predispose to the emergence of psychopathology. While perhaps not a surprise to clinicians, these articles demonstrate the value of understanding the complicated developmental interactions among such factors as early stressors, genetic predispositions, and family behavior. As our science teaches us more about these early-life risk factors, the hope is that a better understanding of the environmental, familial, and genetic determinants of specific psychopathologies will enhance our abilities to transform vulnerability into resilience.