Depression, a common mental disorder, is highly prevalent worldwide and has been identified as a major contributor to global disease burden (
1). The prevalence of depression has been increasing rapidly, yet effective treatments often are not easily accessible, and the etiology of the disorder is unclear (
1,
2). Therefore, the task of identifying preventable risk factors for depression and developing relevant prevention strategies has drawn increasing attention. Ambient air pollution, one of the major environmental risk factors for human health, accounts for the onset and exacerbation of many multisystem diseases, including cardiovascular and pulmonary diseases (
3,
4). Recently, a growing number of epidemiological studies have examined the association between increases in ambient air pollutants and risk for depression (
5–
11) and other mental disorders, including psychological stress (
12), anxiety (
8), and even suicide (
13).
Several experimental studies have investigated the potential biological mechanisms between air pollution exposure and onset of depression, and increased inflammation and oxidative stress in the nervous system induced by air pollutants have been thought to be the major pathways behind the depressive symptoms after exposure (
14–
19). A recent meta-analysis summarized the literature on ambient particulate matter air pollution and risk of depression and found that long-term exposure but not short-term exposure to fine particles (PM
2.5, particulate matter with an aerodynamic diameter <2.5 μm) was associated with an increased risk of depression, which was defined by different methods (e.g., depressive symptoms assessed by different scales, or depression disorder diagnosis assessed by ICD codes) (
20). Only one of the studies included in that meta-analysis investigated hospital admissions for depression; the authors reported positive associations between short-term exposure to ambient particulate matter and hospital admissions for depression (
6). Evidence from epidemiological studies also suggests that short-term exposure to other air pollutants, such as inhalable particles (PM
10, particulate matter with an aerodynamic diameter <10 μm) and nitrogen dioxide (NO
2), were positively associated with risk of depression (
6,
7). However, the results reported in previous studies have been inconsistent, and most of them were conducted in high-income countries with relatively low levels of ambient air pollution. Specifically, evidence is still lacking for short-term exposure to different ambient air pollutants and hospital admission for depression, which indicates a more severe form of depression episode. Furthermore, few of these studies have investigated multiple major ambient air pollutants (including particulate matter and gaseous pollutants) simultaneously, although these pollutants may be associated with the same health conditions (
21). In addition, although the concentrations of ambient air pollution and prevalence rates of depression may vary geographically, few studies have paid attention to the variation in pollutant-depression associations across different regions. Therefore, additional research evidence, especially in areas with a wide range of ambient air pollution levels, is needed to clarify these issues. The large variations in both ambient air pollution levels and depression prevalence rates across China thus provide a unique opportunity to investigate the relationship between ambient air pollution and depression in different regions.
Using national morbidity data from social health insurance schemes in China, we conducted a two-stage time-series analysis to comprehensively investigate the association between short-term exposure to ambient air pollution and daily hospital admissions for depression during the period 2013–2017 in 75 Chinese cities.
Results
From the URBMI and UEBMI insurance databases, we identified a total of 111,620 hospital admissions for depression in the period 2013–2017 in 75 Chinese cities. Among the 75 cities, 37 are located in the southern region, with 52.45% of admitted patients.
Table 1 summarizes the demographic characteristics of admitted patients. Overall, 63.5% patients were female, 59.1% were in the 40- to 64-year age group, and 79.0% were identified in the UEBMI database.
Monthly variation in daily ambient air pollutant concentrations during the study period is shown in Figure S2 in the
online supplement. The daily average concentrations of PM
2.5, PM
10, NO
2, SO
2, O
3, and CO in the 75 cities during the study period were 54.4 μg/m
3, 91.3 μg/m
3, 34.6 μg/m
3, 26.5 μg/m
3, 64.2 μg/m
3, and 1.11 mg/m
3, respectively (
Table 2), and there were medium to high correlations between ambient air pollutants except O
3 and CO (see Table S2 in the
online supplement).
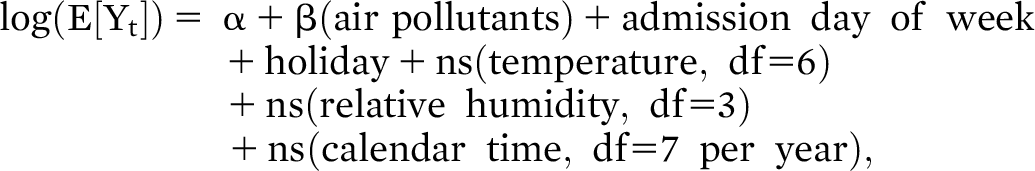
Figure 1 shows the overall percent changes in daily hospital admissions for depression associated with increasing air pollutants at single-day lags of 0–7 days and 01–07 days moving average. Overall, the effect estimates of all included air pollutants, with the exception of O
3, were significant at several lags. At lag01, we found significant increases of 0.52% (95% CI=0.03, 1.01), 0.41% (95% CI=0.05, 0.78), and 1.78% (95% CI=0.73, 2.83) in depression hospital admission for an increase of 10 μg/m
3 in PM
2.5, PM
10, and NO
2, respectively. Forest plots for overall analyses of depression hospital admission associated with different air pollutants at lag01 are shown in Figures S3–S8 in the
online supplement.
The associations between ambient air pollutants and depression admissions, stratified by geographical region, sex, age, and insurance type, were mostly significant at lag01, as shown in
Table 3. Results at other lags are shown in Figures S9–S12 in the
online supplement. The subgroup effect estimates at lag01 were generally significant for NO
2, except in the 19- to 39-year age group and those in URBMI. However, depression admissions significantly increased with increase in NO
2 concentration at lag0 among those in URBMI (see Figure S12 in the
online supplement). We did not observe evidence for significant effect modification by geographical region, sex, age, and insurance type for all effect estimates at the same lag time, although the estimated effects were generally higher in the southern region, in males, in patients 65 years old or older, and in those in URBMI.
The metaregression analysis results showed no evidence for significant effect modification by mean air pollutant levels, temperature, relative humidity, and GDP per capita for air pollutants (see Table S3 in the
online supplement).
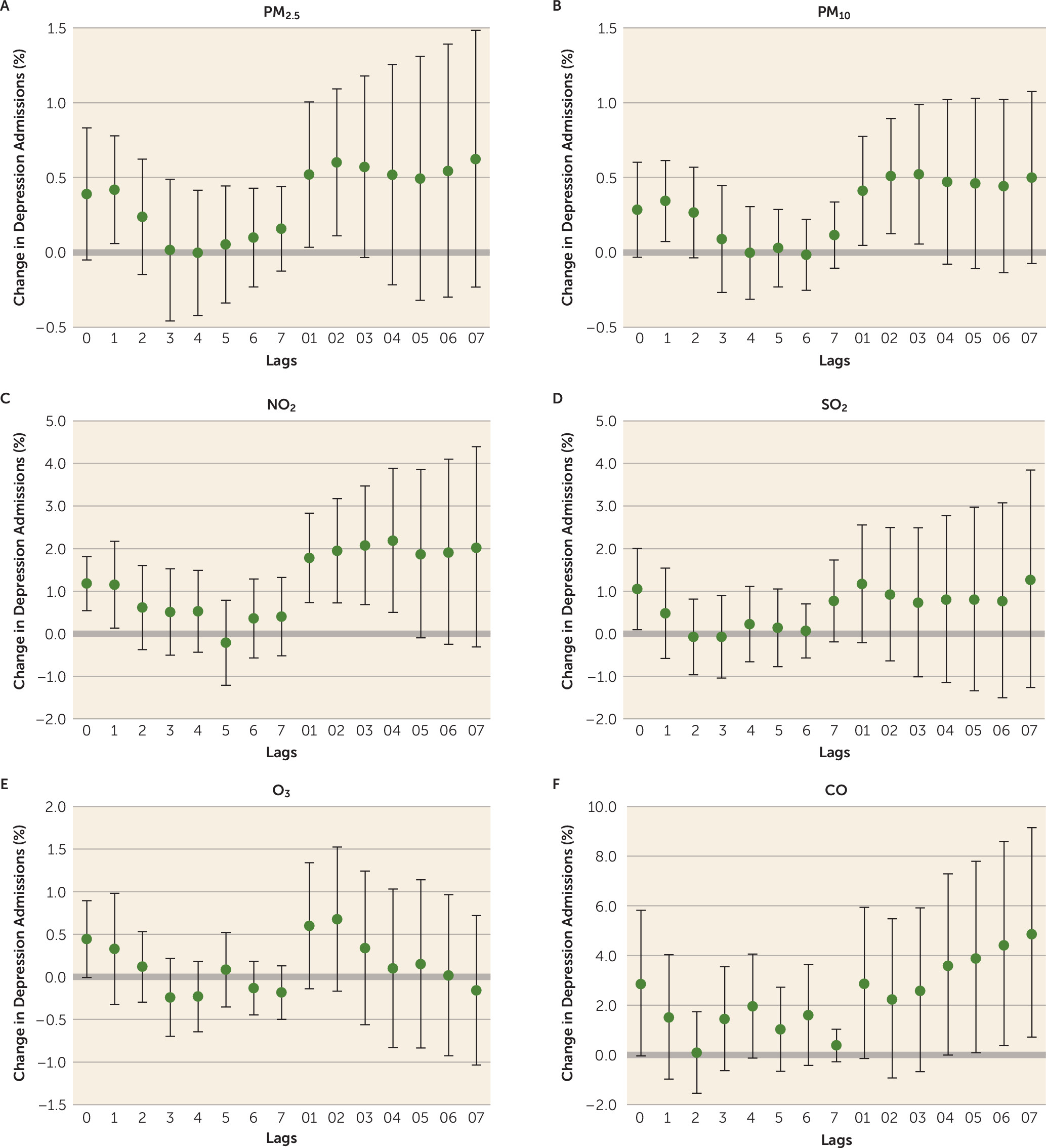
Figure 2 shows the exposure-response curve for the association between NO
2 concentrations (lag01) and risk for depression admission. The curve increased substantially at NO
2 concentrations above 40 μg/m
3.
In sensitivity analyses, the effect estimates of NO2 were robust under different df values of covariates (data not shown). Results of two-pollutant models suggest that only the effect estimates of NO2 were significant after controlling for other air pollutants at the same lag time (see Table S4 in the online supplement).
Discussion
To our knowledge, this is the largest study to explore the association between short-term exposure to multiple ambient air pollutants and hospital admission for depression. After conducting the two-stage analyses, we found that short-term exposures to ambient PM2.5, PM10, NO2, SO2, and CO were significantly associated with increased risk for hospital admission for depression. Moreover, the effect estimates of NO2 were generally consistent across different geographical regions and demographic characteristics, including sex, age, and insurance type, and were robust to adjustment for other air pollutants.
It is well known that exposure to ambient air pollution could cause increased respiratory and systemic inflammatory response and oxidative stress in the human body (
30,
31), and several experimental studies have demonstrated that the increased inflammatory response and oxidative stress could be expanded to the central nervous system in both short-term and long-term exposure scenarios (
14–
19). In fact, depression is a condition of typically insidious onset and relatively long course, and both epidemiological studies (
8,
10,
11) and toxicological studies (
17–
19) have found that long-term exposure to ambient air pollution is linked to the onset of depression. Similarly, long-term exposure to ambient air pollution has also been consistently associated with increased risk of cardiovascular and respiratory diseases, two types of chronic diseases with long courses (
3,
32). However, short-term changes in ambient air pollution within short periods have also been associated with the onset of acute cardiovascular events (e.g., acute ischemic coronary events or acute decompensated heart failure) and respiratory events (e.g., exacerbation of chronic obstructive pulmonary disease) (
33–
35). Therefore, it is thought that short-term changes in ambient air pollution may trigger significant changes in a health condition (e.g., exacerbation of chronic obstructive pulmonary disease) on the basis of changes already induced by prior long-term exposure to ambient air pollution (e.g., respiratory disease status). Among patients with admissions for depression, it is possible that many were suffering from preexisting depressive symptoms, and short-term changes in ambient air pollution could serve as the trigger to induce moderate to severe depressive symptoms requiring hospitalization for intensive treatment.
Several epidemiological studies have investigated the association of short-term exposure to ambient air pollution with risk of depression (
5–
7,
9,
20,
36), but only two of them used hospital admission data (
6,
36). A case-crossover study with 19,646 hospital admissions for depression (
6), drawn from electronic hospitalization summary reports of tertiary A hospitals, found that short-term elevations in ambient particulate matter were associated with an increased risk of hospitalization for depression in 26 Chinese cities in 2014 and 2015, and the estimated increases in hospital admissions for depression were 3.55% and 2.92% at lag 0 for an interquartile-range increase in PM
10 and PM
2.5 (76.9 μg/m
3 and 47.5 μg/m
3), respectively. Another study also found a significant positive association between short-term exposure to PM
2.5 and hospital admissions for depression (N=1,193) in 2015 and 2016 in Chengdu, a major city in Western China (
36). In addition, other studies have reported significant positive associations between short-term exposure to ambient air pollution and emergency department visits for depression in a limited number of cities (
5,
7,
9). Our study is able to expand the analyses for short-term exposure to ambient air pollution and hospital admission for depression to 75 Chinese cities, with a much larger number of admissions (N=111,620) over a period of 5 years, and is able to provide a detailed analysis for other gaseous pollutants, including NO
2, SO
2, O
3, and CO, along with ambient particulate matter. Our results support the positive associations between short-term exposures to ambient PM
2.5 and PM
10 and hospital admission for depression and suggest that the gaseous pollutants NO
2, SO
2, and CO were also associated with an increased risk of admission for depression.
In addition to particulate matter, several previous studies have also reported associations of depression-related outcomes with other air pollutants, including NO
2 (
5,
7,
9,
37), SO
2 (
5,
7,
9), O
3 (
5,
7,
9), and CO (
5,
9), but the results have been inconsistent. For example, a recent cohort study in England and Wales found that long-term exposure to ambient NO
2 was more strongly associated with increased adolescent psychotic experiences, a risk factor for depression, than PM
2.5 and PM
10 (
37). However, another study did not find any association for short-term exposure to NO
2 and emergency department visits for depression in Ontario’s hospitals in Canada (
7). Our study was able to comprehensively examine the potential effects of particulate matter and gaseous air pollutants on daily admissions for depression in a much larger population, and thus provided greater statistical power to investigate the independent impact on depression admissions for different air pollutants. Based on our study findings, we suppose that NO
2 may be the key air pollutant contributing to the increased depression risk. As mentioned earlier, increased oxidative stress may be one of the biological pathways behind the association between air pollution and depression. Specifically, oxidative stress occurs when there is an excess of free radicals over antioxidant defenses. The ambient air pollutant NO
2 functions directly as a nitrogen-centered free radical after being inhaled into the lungs, whereas other components of air pollutants mainly function as powerful oxidants to induce this pathway (
38). Increased oxidative stress in the nervous system is toxic to dopaminergic neurons (
15), which could contribute to the onset of depression, since depletion of dopamine in the central nervous system is one of the underlying pathophysiological mechanisms for depression (
39).
Results of subgroup analyses could offer insights into susceptible populations and suggest implications for research and public health promotion. Our subgroup study showed that the positive associations between NO
2 and hospital admission risk for depression were the most robust among the investigated air pollutants. In addition, the effect estimates were not modified by the mean air pollutant levels, city-specific levels of temperature, relative humidity, and GDP per capita. We found, too, that effect estimates of NO
2 appeared higher for males than for females at the same lag time, which is consistent with findings from a previous study (
5). We also found that the effect estimates of NO
2 in the age 65 or older group were all higher than in other age groups, which may be due to the potential high sensitivity of older people to air pollution effects (
6). The higher effect estimates of NO
2 found in URBMI compared with UEBMI may be related to the “healthy worker effect” (
40), which usually appears as a minor reduction of morbidity in occupational cohorts compared with the general population. Moreover, although the differences were statistically insignificant, we found that NO
2 and CO were more strongly associated with hospital admission risk for depression in the southern region compared with the northern region, potentially because of the variation of major air pollutant components between these regions as a result of China’s Huai River Policy, which provided free winter heating via the provision of coal for boilers to the northern cities but not to the southern cities. Northern cities generally have a higher proportion of air pollutants from the combustion of coal, such as total suspended particulates and SO
2, whereas air pollutants in southern cities are more closely associated with vehicle exhaust emissions, especially of NO
2 and CO (
26). Furthermore, doors and windows of buildings in the southern region are poorly sealed compared with those in the northern region, and gaseous pollutants are more likely to penetrate indoors, which may be one of the reasons why the estimated health effects in the southern region were more significant.
Our study has several strengths. Most previous studies have been restricted to a single city or region, or to large hospitals, and thus have limited representativeness and power to investigate the question of interest among the general population. This study investigated the short-term association between major ambient air pollutants and hospital admission risk for depression in a large number of cities in China by using national medical insurance data covering a large proportion of the general urban population, and thus has fair representativeness. Moreover, our investigation, based on multiple high-heterogeneity cities, provides research evidence for the potential modification effects of geographical region, weather conditions, air pollution levels, and socioeconomic status on the estimated risk of hospital admission for depression associated with air pollution.
Our study also has several limitations, which are similar to those of other studies using the same analytic method (
24,
25). First, ecological bias is inherent to the time-series analysis method. For example, we did not have specific individual diagnostic data to allow classification of depression admission cases into subgroups according to the severity of their symptoms, or as initial or recurrent admission for depression, a limitation that may affect the interpretation of the results into clinical practice. Second, since no specific exposure data were obtained for individual subjects, exposure measurement errors would occur from using ambient air pollution data at the city level instead of at the individual level or at the level of smaller geographical units. Nevertheless, previous studies have shown that fixed-site air monitoring measurements could reflect ambient air pollution levels of the urban background to a certain extent (
41), and the monitoring data have been commonly used as a proxy for population exposure to ambient air pollution in previous time-series analyses (
25,
42). Third, potential misclassification of depression diagnosis in insurance data should also be considered, although these possible errors would be expected to bias the risk estimates toward null (
43). Fourth, the collinearity among ambient air pollutants limit the interpretation of the effect estimates of single air pollutants in the two-pollutant models. Fifth, studies have shown that other factors, such as noise (
44), psychological stress (
45), poverty (
46), and population density (
47), may also influence the risk of depression, but related data were not available in this study. Although we considered the impact of GDP per capita on the results and no significant effect modification of the exposure-health associations by GDP per capita was found, future studies would benefit from investigating the potential confounding effects of these factors in the context of ambient air pollution. Finally, subgroup analyses for patients age 18 and under were not conducted because few cities met our inclusion criterion (≥200 admission cases) for subgroup analysis for patients in that age range. Because the brain and respiratory system are still developing in children and teenagers and are considered more vulnerable to ambient air pollution, future studies should also pay more attention to individuals in this age group.
In summary, our findings suggest that increases in short-term exposure to ambient air pollution are associated with increased risk of daily hospital admission for depression among the general urban population in China. Targeted strategies such as more stringent air pollution guidelines and air quality control measures may be helpful for promoting public mental health. Further studies are needed to confirm our findings and to investigate the underlying mechanisms for the reported associations.