In 2016, the U.S. Food and Drug Administration (FDA) issued a black box warning on the potential risk of respiratory depression after combined use of opioids and benzodiazepines or other CNS depressants, including sleep drugs (such as Z-drugs and barbiturates) (
3). Although the supporting evidence linking the risk of opioid overdose and benzodiazepine use was substantial (
4 –
7), no evidence was cited directly linking opioid overdose risk to Z-drug hypnotic agents. Instead, the warning was based on their similar pharmacological properties, even though benzodiazepines and Z-drugs preferentially bind to different subunits of the GABA receptor (
8,
9).
Despite the 2016 warning, the use of Z-drugs (zolpidem, zopiclone, zaleplon) remains widespread among prescription opioid users, regardless of the underlying indication. In the United States, it has been reported that the use of Z-drugs rose from 0.37% in 1999–2000 to 1.57% in 2013–2014, which reflects approximately 5 million individuals and a relative increase of 324%. Close to one-quarter of these patients co-use opioids (
10), which equates to about 1.2 million individuals. Physicians prescribing opioids may be unaware that their patients are taking hypnotic Z-drugs, especially when multiple health care providers are involved in the patient’s care. A 2014 study found that 48.5% of patients with pain who used zolpidem in the United States did so without the knowledge of their pain management provider (
11).
We thus designed a large cohort study of commercially insured beneficiaries to evaluate the risk of overdose among patients with prescriptions of both Z-drugs and prescription opioids compared with patients with opioid prescriptions alone.
METHODS
Data Source
The IBM MarketScan Commercial and Medicare Supplemental claims database (IBM MarketScan) includes patient demographic characteristics, insurance enrollment history, inpatient and outpatient medical claims, and outpatient prescription claims for nearly 115 million unique patients in the United States. The data are entered for billing purposes, and coding is considered high quality because the adjudication of the claim depends on its accuracy.
Study Population and Exposure
The source cohort comprised all patients 15 to 85 years of age in the MarketScan database who had filled an opioid prescription between January 1, 2004, and December 31, 2017. Within this source cohort, we first identified incident use of Z-drugs. The Z-drug exposure was considered to be incident if it was preceded by 180 days without Z-drug prescription fills. We required continuous medical and prescription drug benefit coverage for 180 days before the date of the Z-drug prescription fill, which was considered the index date, and no evidence of cancer or palliative care. In order to define concomitant use of Z-drugs and opioids (“exposure”), we required at least one opioid prescription to be filled within the 14-day window before the index. (See Figure S1 and Table S1 in the online supplement for, respectively, the study design and a complete list of opioid formulations included.) A patient could contribute multiple episodes of concomitant Z-drug and opioid use, as long as the inclusion criteria were met. We randomly selected one episode per patient per calendar year.
The reference cohort consisted of all episodes of prescription opioid use that met the same criteria as exposed treatment episodes: continuous enrollment for 180 days prior to the opioid prescription fill (i.e., index date) and no evidence of cancer or palliative care.
Next, exposed treatment episodes were matched 1:1 to a reference treatment episode in chronological order of their index dates. We matched treatment episodes on 1) calendar year; 2) type of opioid; 3) morphine equivalents for the prescription immediately preceding the index date for the exposed individual (matched ±50 morphine equivalents to the qualifying prescription for the reference individual), and for all prescriptions in the past 180 days (±100 morphine equivalents); 4) total number of days’ supply covered by all opioid prescriptions in the past 180 days (±5 days); and 5) hospitalization within the past 30 days (see Appendix 1 in the online supplement). Once an exposed treatment episode had been matched to a reference treatment episode, the individuals were no longer available for future matches. This procedure ensured that the final cohort was defined at the individual patient level (as opposed to the treatment episode level).
Outcome
The primary outcome was defined as any hospitalization or emergency department visit due to an overdose event within 30 days of the index date (including the index date itself), based on ICD-9 or ICD-10 diagnostic codes (see Table S2 in the online supplement). We excluded those outcomes with a suicide-related code on the same date.
Covariates
Potential confounders and proxies for confounders were identified during the 6 months before the index date. We considered a large number of patient characteristics to capture both overt risk factors for overdose and variables that may be proxies of risk factors that were unmeasured or incompletely measured in our data set (Table
1; see also Table S3 in the
online supplement).
Statistical Analysis
We compared baseline characteristics between patients who received Z-drugs and opioids concomitantly and those who received opioids alone. Patients were followed until the occurrence of the outcome, death, end of enrollment, end of the study period (December 31, 2017), or 30 days, whichever came first (see Figure S1 in the online supplement). Consistent with an intention-to-treat approach, we disregarded treatment changes that occurred during follow-up in the primary analysis. Incidence rates and their 95% confidence intervals were calculated for each group.
We used fine stratification on the propensity score to address confounding. The propensity score was estimated by fitting a logistic regression model with all the variables listed in Table
1. After exclusion of individuals from the nonoverlapping regions of the propensity score distribution, we created 50 equally sized strata based on the distribution of the propensity score among the exposed. Adjusted hazard ratios and 95% confidence intervals for the association between Z-drugs and the risk of overdose were estimated by means of a Cox proportional hazard regression model in which reference individuals were weighted by the propensity score distribution of the exposed individuals. The reference weights thus scaled up or down the number of reference individuals to match the proportion of exposed individuals in a given stratum (see Appendix 2 in the
online supplement). A discrete-time hazard model with a flexible function of time was used to estimate adjusted survival curves and to compute the absolute event-free survival at the end of follow-up (see Appendix 3 in the
online supplement) (
12,
13); 95% confidence intervals were obtained via nonparametric bootstrapping with 500 samples.
The robustness of our findings was evaluated on the basis of a number of subgroup and sensitivity analyses. We stratified our results by age (<40 years, 41–65 years, and ≥66 years) and gender. For sensitivity analyses, we extended the follow-up period from 30 to 90 days and conducted a 90-day as-treated analysis in which we censored patients when they changed treatment during follow-up, allowing for a 14-day grace period (i.e., for exposed patients, when they discontinued either the Z-drug or the opioid, and for the reference patients, when they discontinued the opioid or initiated a Z-drug) (see Appendix 4 in the
online supplement). To address the potential for outcome misclassification, we varied the definition of overdose by 1) including only diagnostic codes for opioid-related overdose (i.e., not allowing psychotropic-drug-related overdose codes), 2) requiring a respiratory failure code on the same date as the overdose, and 3) removing the codes for sedative/hypnotic overdose from the outcome definition, as these are more likely to be recorded for patients in the exposed group. To evaluate the potential for residual confounding due to a higher number of medical comorbidities among the exposed, we employed proton-pump inhibitor (PPI) prescriptions as a negative exposure control, as patients with multiple comorbidities are frequently treated with PPIs (
14). Since we would not expect PPIs to be associated with an increased risk of overdose, a null finding in this analysis would provide indirect evidence of no substantial residual confounding (see Appendix 5 in the
online supplement). We repeated the analyses excluding patients with any evidence of major psychiatric disorders to prevent residual confounding due to underlying psychiatric disease severity. Finally, we conducted an active comparator analysis in which we compared patients using opioids plus Z-drugs to patients using low-dose trazodone (≤50 mg) plus opioids, to address questions about comparative safety and inform clinical practice.
This study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (
15). All analyses were conducted using SAS, version 9.4 (SAS Institute, Cary, N.C.). The Brigham and Women’s Hospital institutional review board provided ethical approval.
RESULTS
The cohort consisted of 510,529 exposed patients matched to the same number of reference patients who met inclusion criteria (Figure
1).
Patients exposed to Z-drugs and opioids tended to be older and to have a higher number of medications prescribed, higher health care use, and a higher prevalence of certain psychiatric diagnoses (e.g., depression and anxiety) (see Table S8 in the
online supplement) and pain diagnoses (e.g., headache and joint pain) than reference patients (Table
1). After stratification on the propensity score, all measured patient characteristics were balanced (Table
1; see also Table S3 in the
online supplement).
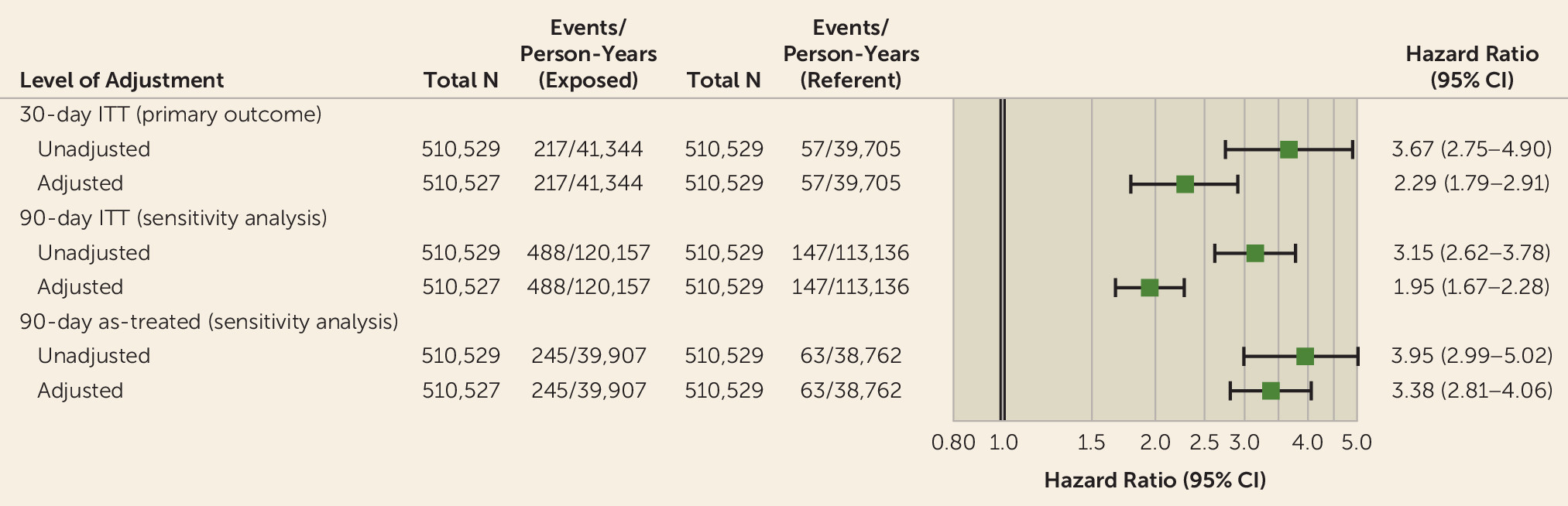
There were 217 overdose events per 41,344 person-years among patients who had prescriptions for both Z-drugs and opioids, corresponding to an incidence rate of 52.5 overdose events per 10,000 person-years (95% CI=45.9, 60.0), and 57 overdose events per 39,705 person-years among patients exposed to opioids alone, for an incidence rate of 14.4 overdose events per 10,000 person-years (95% CI=11.1, 18.6).
The unadjusted hazard ratio for overdose comparing patients who had prescriptions for both Z-drugs and opioids and patients exposed to opioids alone was 3.67 (95% CI=2.75, 4.90). After adjustment for all measured confounding variables through fine stratification on the propensity score (and removal of two exposed patients in the nonoverlapping area of the propensity score distribution), the hazard ratio attenuated to 2.29 (95% CI=1.79, 2.91) (Figure
2). The effect, stratified by age group, was 2.43 (95% CI=1.62, 3.64) for those under age 40, 2.11 (95% CI=1.52, 2.94) for those between ages 41 and 65, and 2.53 (95% CI=1.18, 5.38) for those older than age 65. The hazard ratio was 1.69 (95% CI=1.27, 2.27) for females and 2.51 (95% CI=1.45, 3.45) for males.
Adjusted survival curves are presented in Figure
3. The absolute risk difference at 30 days was 25.0 events per 10,000 exposed (95% CI=10.0, 32.0) (see Table S4 in the
online supplement). Extending the follow-up to 90 days resulted in an adjusted hazard ratio of 1.95 (95% CI=1.67, 2.28) for the intention-to-treat analysis and an adjusted hazard ratio of 3.38 (95% CI=2.81, 4.06) for the as-treated analysis (Figure
4). The absolute risk difference at 90 days was 110 events per 10,000 exposed (95% CI=60.0, 150.0) (Figure
3). Varying the definition of overdose did not meaningfully affect the results (see Table S5 and Figure S4 in the
online supplement). Finally, no increased risk was observed in the negative exposure control (proton-pump inhibitor) analyses (hazard ratio=1.04; 95% CI=0.82, 1.32) (see Appendix 5 in the
online supplement).
After restricting our cohort to patients without any recorded diagnoses for psychiatric disorders, we obtained a crude hazard ratio of 3.26 (95% CI=2.02, 5.24) and an adjusted hazard ratio of 1.95 (95% CI=1.31, 2.89), consistent with the results from the primary analysis (see Table S6 in the online supplement).
In the active comparator analysis, we matched 60,751 patients using opioids plus Z-drugs to 60,751 patients using opioids plus low-dose trazodone. Patients on Z-drugs received a lower number of concomitant psychotropic medications, had a fewer diagnoses (e.g., anxiety, depression, or insomnia), and had fewer psychiatry and emergency department visits in the past 180 days than patients on trazodone, but all characteristics were balanced after propensity score stratification (see Table S6 in the
online supplement). There were 29 events per 3,768 person-years in the opioid plus trazodone cohort (incidence rate=77.0 overdose events per 10,000 person-years) and 25 events per 3,765 person-years in the opioid plus Z-drugs cohort (incidence rate=66.4 overdose events per 10,000 person-years), corresponding to a crude hazard ratio of 0.86 (95% CI=0.51, 1.47) and an adjusted hazard ratio of 1.58 (95% CI=0.84, 2.96) (Figure
4).
DISCUSSION
In this population-based cohort study, we found a substantially increased risk of unintentional overdose associated with the coprescription of Z-drugs to patients receiving opioids as compared with patients using only prescription opioids, after accounting for a broad range of potential confounding factors. This finding was robust to all of the sensitivity analyses performed. The risk of unintentional overdose increased more than twofold in the 30-day intention-to-treat analysis and almost threefold in the 90-day as-treated analysis, suggesting that the cumulative dosage of Z-drugs may play a significant role in the risk of unintentional overdose.
This study substantially increases the evidence available on the topic. In 2016, the FDA issued a warning against the joint use of opioids and benzodiazepines, based on substantial evidence of an increased risk of overdose (
4 –
7) (an increased relative risk oscillating from 2.14 to 5.05) but also extended the warning to include Z-drugs despite the lack of direct evidence for these agents. One previous study (
16) suggested that the combination of Z-drugs and opioid maintenance treatment (methadone or buprenorphine) was associated with an increased risk of overdose death (hazard ratio=1.60, 95% CI=1.07, 2.39) and a potentially small increase in all-cause mortality (hazard ratio=1.28, 95% CI=0.93, 1.75). No effect on nonfatal overdoses was observed (hazard ratio=0.96, 95% CI=0.59, 1.59), but the confidence interval was wide. However, that study focused on opioid maintenance treatment, as opposed to prescription opioids, which represents a very different clinical context. In addition, in 2017, the FDA issued another communication urging physicians to be cautious about withholding opioid addiction medications from patients taking hypnotic agents, based on the limitations of that study (
17).
Although Z-drugs are widely perceived as safe (
18,
19), drug-induced respiratory depression has been reported in association with their use (
20,
21). Z-drugs bind the major modulatory site of the GABA
A receptor, the same receptor that exerts the effect of benzodiazepines, but Z-drugs exhibit a preferential affinity for a specific subunit. Given the number of previous reports suggesting that the coprescription of benzodiazepines and opioids yields an increased risk of unintentional overdose, especially in the first days of their combined use (
4,
5,
7), there is concern that a similar effect may occur when combining opioids and Z-drugs, which underlies the rationale for Z-drugs being included in the FDA warning. While we did observe an increased risk associated with the coprescription of Z-drugs and opioids, which may be attributed to the binding of GABA
A receptors (the same receptors that exert benzodiazepines’ action), the effect was smaller as compared with the previously reported estimate for the coprescription of benzodiazepines (
6,
7). A potential explanation is that zolpidem, the most widely used among the Z-drugs, has a very short half-life (as does zaleplon), whereas the half-life of benzodiazepines varies widely (
22). Given the same opioid, ingesting a short-acting agent (such as a Z-drug) may pose less of a risk than a longer-acting agent (such as a benzodiazepine). Trazodone, on the other hand, provides sedation through a mechanism that is not well understood. It acts as an antidepressant mainly through the blocking of 5-HT
2 receptors, and it also has alpha-1 adrenergic blocking properties (
23). Because trazodone does not interact with GABA neuromodulation, it is plausible that it carries a lower risk of unintentional overdose when combined with opioids. After adjusting for confounding, we did indeed observe a higher risk of unintentional overdose with Z-drugs compared with trazodone. This suggests that trazodone may be a safer alternative for the treatment of insomnia in patients using opioids, but this will need to be confirmed in subsequent studies. Furthermore, a careful evaluation of other risks associated with its use (e.g., anticholinergic effects, dysphoria, priapism) (
24) is also warranted.
After the FDA issued the warning against the coprescription of opioids and benzodiazepines in 2016, there has been evidence suggesting that their concomitant use has started to decline (
25). Our findings suggest that Z-drugs should not be considered a safe alternative. The most recent Centers for Disease Control and Prevention guidelines for the prescription of opioids for patients with chronic pain recommend that naloxone be prescribed for patients with a prior history of overdose, patients with substance abuse disorder, and patients taking benzodiazepines concomitantly (
26). The results from this study suggest the possibility that the concomitant use of Z-drugs should be added as a risk factor for overdose and an indication for naloxone.
This study has several important strengths. First, we employed an outcome definition that captured both opioid overdose and psychotropic medication overdose in an emergency department or hospital setting. This was done to capture all serious unintentional overdose events with a sedative profile that could correspond to either opioids or psychotropic medication, since the underlying causative medication may be unknown to the prescriber at the time of recording the diagnosis. Second, health care utilization data contain rich patient-level information that can be used to control confounding, such as other concomitant medication exposures that also have sedative properties and thus might potentially increase the risk of unintentional overdose (
27). In addition, we conducted a negative exposure control analysis to assess the potential for residual confounding affecting our results (
28). We found no evidence for an increased risk, providing confidence in the validity of our findings. Finally, this study benefits from a large sample size, which allowed reporting of precise estimates of the risk of unintentional overdose associated with the coprescription of Z-drugs and opioids.
However, this study has also some limitations. First, filling a prescription for a Z-drug does not mean that the medication was actually consumed during our 30-day follow-up period. If patients did not actually take their Z-drugs, this nondifferential misclassification of our exposure would bias the results toward the null, and our estimate of increased risk would be conservative (
29). Second, unintentional overdoses that were fatal prior to hospital admission would have been missed, resulting in decreased sensitivity of the outcome definition. However, as long as the proportion of such fatal overdoses is nondifferential between the exposed and the reference groups (that is, as long as concomitant use of Z-drugs does not disproportionately increase the risk of fatal overdoses), the relative risks should be unbiased. Third, as in every nonrandomized study, there is always concern about residual confounding due to unmeasured or poorly measured characteristics. For example, claims data do not reliably capture substance abuse, a well-established risk factor for overdose, and patients with substance abuse are also more likely to report sleeping problems. However, for the imperfectly measured substance abuse to explain our findings, it would have to be associated with Z-drug prescription and with overdose by at least a factor of 4.84. This strength of association is highly unlikely, since we controlled for a number of confounders and proxy measures in the analysis. Fourth, the presence of some intentional overdoses in our outcome definition could not be completely ruled out, and a higher risk of intentional overdoses could be explained by a more severe psychiatric illness presentation among Z-drug users. To address this potential residual confounding, we restricted the cohort to patients without a recorded psychiatric diagnosis, and we chose trazodone, a drug used for similar indications but with a different mechanism of action, as an active comparator agent. Results from both analyses were consistent with the main findings. Finally, this study only includes commercially insured individuals, and a publicly insured population, such as the Medicaid population, is known to have a higher burden of comorbid mental disorders and higher use of opioids. However, the biological effects studied are expected to generalize to other populations.
In summary, among patients receiving a prescription opioid medication, exposure to Z-drugs was associated with an increased risk of unintentional overdose after accounting for measured confounders. Although absolute risks were small, the potential implications of these findings are substantial given the growing number of opioid-treated patients receiving Z-drugs, which we estimated to be about 1.2 million individuals in the United States, based on the 2013–2014 NHANES survey (
10). This would correspond to approximately 13,000 events that could be prevented by rational prescription of these two agents. Clinicians need to weigh this risk when considering whether to coprescribe Z-drugs to patients taking prescription opioids.