Alcohol use disorder (AUD) is a dynamic condition marked by changes in a constellation of brain structures and functional concomitants that evolve with chronically excessive consumption and that change again with alcohol abstinence (
1). The changes, considered neuroadaptation, do not occur instantly. Rather, neuroadaptation to life without alcohol takes time and is complicated by the nature of alcohol dependence as a multisystem disorder. Accordingly, recovery trajectories of affected neural systems differ, and as a consequence, recovery trajectories of the associated affected behaviors are not in lockstep. A large segment of support for this conceptualization of AUD development and recovery, especially in its early postabstinence phase, derives from animal models of high alcohol exposure because of the control the experimenter has over influential factors, including dose, schedule of exposure, and course of withdrawal and recovery (
2).
In humans, these critical factors that occur early in the alcohol withdrawal phase can be observed only in a naturalistic setting, such as a detoxification clinic, which is seldom done for two salient reasons. First, recruiting people with AUD early in detoxification to participate in research is challenging because their medical needs take precedence over research protocols, and their affective state during detoxification is often negative. Second, there is a tradition of studying newly abstinent individuals at least 2 weeks after detoxification to avoid acute withdrawal effects as contaminants to brain imaging or neuropsychological findings. Given those limitations, controlled research has yielded a robust characterization of the postacute, residual effects of AUD. What the study by Blaine et al. in this issue of the
Journal (
3) succeeded in achieving is a rigorous examination of brain and physiological responsivity to alcohol cues and non-alcohol stressors during early detoxification, using a uniquely powerful prospective two-part paradigm in a clinical research setting:
•
Study 1 conducted research procedures 1–12 days after a person’s last drink, thereby allowing examination of the brain’s response to alcohol cues and stressors during acute abstinence.
•
Study 2 included persons recovering from AUD whose length of abstinence was 1–35 days, thereby allowing examination of the effects of varying intervals on alcohol craving and cortisol stress responses with reference to time to relapse and amount of alcohol consumed between the functional MRI (fMRI) and cortisol study date and the end of the subsequent 2-week behavioral treatment program.
•
For both studies, all research procedures, including fMRI scanning, were conducted at treatment entry, which occurred before outpatient behavioral treatment commenced.
•
Participants were required to arrive at the research clinic at 7 a.m. for fasting blood tests, ensuring control over consumption of food, drink, and cigarettes for accurate cortisol testing.
•
Smartphone surveys enabled real-time tracking of alcohol consumption during the subsequent 2 weeks of outpatient treatment.
•
The non-AUD comparison group, which included social drinkers, was well matched to the AUD group on age, sex, race, intelligence scores, and education, and the two groups underwent identical study procedures.
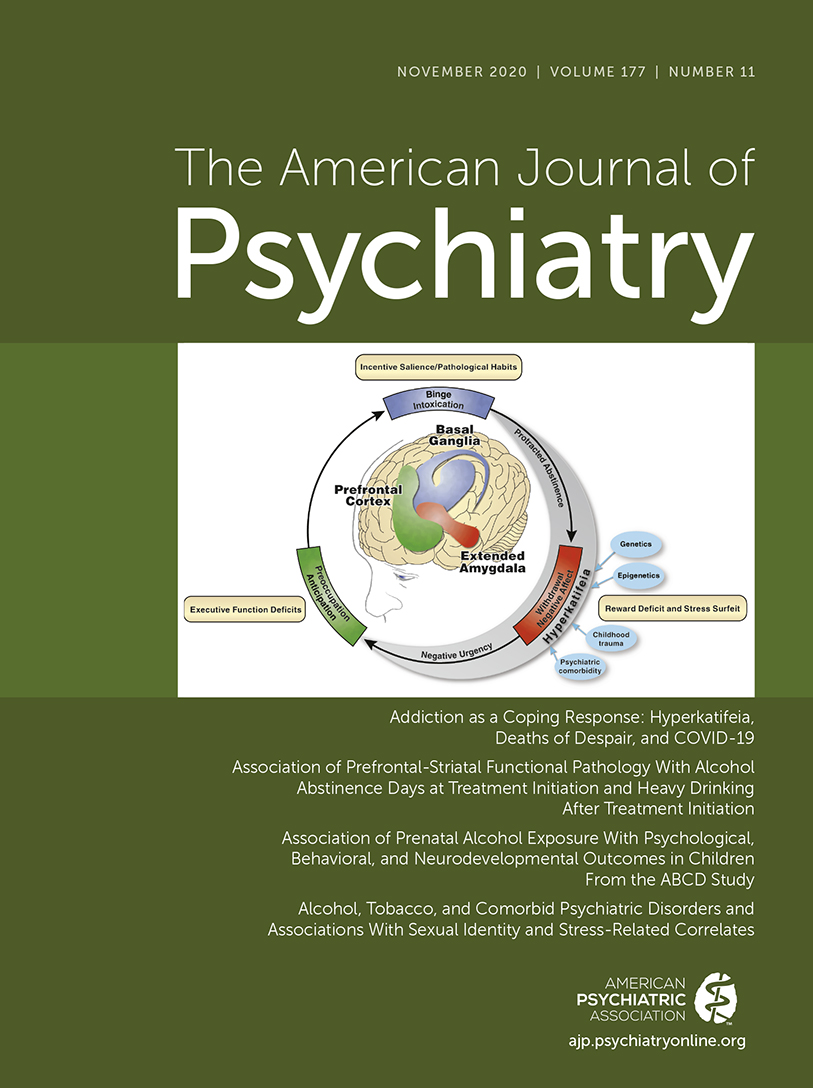
The fMRI paradigm comprised three visual conditions: appetitive alcohol cues, threatening stressors, and neutral photographs. Condition comparisons sought brain activation differences hypothesized to affect fronto-cingulo-striatal-limbic regions in the AUD group. For the neutral condition, results indicated that the AUD group exhibited hyperactivation in these brain regions, specifically, the ventromedial prefrontal cortex (vmPFC), including the rostral anterior cingulate cortex (rACC). For the stress-neutral and the alcohol cue-neutral contrasts, however, the AUD group showed regional hypoactivation in the vmPFC/rACC and the ventral and dorsal striatal regions. These differences between AUD and control group activation patterns were greater with fewer days of alcohol abstinence in the AUD group.
The functional ramifications of these findings are profound, indicating that the early days of abstinence count substantially. Indeed, each day of abstinence resulted in a 14% decrease in the likelihood of subsequent relapse. Why should relapse be so tied to early abstinence? Knowledge about a temporal continuum of dysregulation of the fronto-striatal and fronto-limbic systems related to days of sobriety contributes to a neurocircuitry and neuroadaptation understanding of emotional dysregulation also characteristic of the early hours and days of abstinence (
4) and reliance on these brain systems (
5).
Emotion regulation refers to the ability to modulate positive and negative emotional states, to control impulsive behavior, and to feel and express empathy. These abilities come under the umbrella of social cognition, which is a multifaceted psychological construct that describes the ability to understand and appropriately react to emotionally charged situations. These functions are targets in rehabilitation efforts to raise awareness of the untoward effects that AUD has on life and society, but early in recovery, salient impairment in social cognition, especially with respect to components of emotion regulation, poses a significant obstacle to therapy (
5). Neuroimaging studies like that of Blaine et al. provide evidence for this impairment based on brain functional differences from control subjects. Specifically, individuals in recovery from AUD process information related to alcohol and stress differently from control subjects (
3), which may provide a neural systems explanation for troubles reported in recognizing their own disabilities in memory (
5), in interpreting affect (
6), and in accurately engaging in other self-referential skills (
7). Indeed, early in abstinence, individuals with AUD often appear to be in denial of the harm drinking has on their lives and in recognizing their compromised cognitive abilities when in fact denial itself can be evidence of a cognitive deficit related to neural dysfunction and expressed as a mild anosognosia (
8). Consistent with this possibility is the abnormal dampening of activity reported by Blaine and colleagues in fronto-cingulo-striatal-limbic circuitry in response to alcohol cues and stressors that could be speculated to be a defense mechanism and a form of implicit protection against unchecked attention to such information. An alternative interpretation is that low alcohol-associated cue and stress responsivity indicates psychological and physiological adaptation to them.
To the extent that these speculations provide viable hypotheses regarding selective impairment in cognitive awareness and affect in early abstinence, they deserve further study—and may have translational relevance to clinical settings. For example, contact either through an inpatient clinic or through telehealth communication, as conducted in the Blaine et al. study, would provide continuous reminders, support, and reinforcement to sustain alcohol abstinence or drinking reduction during the early hours and days of withdrawal. This is both a highly vulnerable time for relapse and a critical time for initiating neural healing and recovery. In support of this scenario, structural MRI studies consistently show frontal regions to be selectively vulnerable to AUD (
9), to be predictive of relapse (
10), and to show functional recovery not only with abstinence but also with reduced drinking (
11). Recognition that neuroadaptation toward sustained sobriety is a dynamic process that takes time is consistent with positive findings using pharmacological treatment. For example, acamprosate has been useful in quelling cravings early in sobriety, and naltrexone has been used later in recovery to maintain sobriety (
12).
AUD is a serious medical problem. About 88,000 deaths occur annually in the United States from alcohol-related causes, making it the country’s third most prevalent cause of death (
13). Furthermore, nearly 6% of U.S. adults were estimated to have AUD in 2018. Substantial increases in binge drinking and chronically hazardous drinking among women (
14) and men (
15) are compounding the problem, which appears to have worsened with the coronavirus pandemic (
16). Before the pandemic, only ∼8% of individuals with AUD received treatment, a proportion that may be even less favorable given the rise in drinking during COVID-19 and restriction on rehabilitation enrollment related to alcohol and drug abstinence (
17). Notably, about one-quarter of admissions to publicly funded rehabilitation programs are due to alcohol abuse (
https://www.alcohol.org/statistics-information/). The Blaine et al. study provides compelling data for these acutely treated patients to seek continued treatment to aid in abating hazardous drinking and in harm reduction. It is now clear that the first few days of detoxification are critical for promoting prolonged sobriety. We also know from studies of social cognition and rehabilitation efforts that treatment strategies that work to reinforce sobriety when craving is at a peak are likely to change with the temporal course of abstinence and ensuing neuro-readaptation.