For much of the 20th century, psychotherapy was viewed as synonymous with psychiatry and was the primary treatment modality employed by outpatient psychiatrists (
1). Psychiatrists still view psychotherapy as core to their practice (
2). APA’s most recent practice guidelines recommend that patients be provided psychotherapy across a range of diagnoses, such as schizophrenia, major depressive disorder, bipolar disorder, panic disorder, and obsessive-compulsive disorder (OCD). Additionally, the 2020 program requirements of the Accreditation Council for Graduate Medical Education (ACGME) expect residents to have proficiency in the use of various psychotherapeutic approaches (
3). Indeed, clinical research demonstrates that state-of-the-art evidence-based individualized care often requires a combination of pharmacotherapy and psychotherapy (
4). Yet, since the 1980s, significant declines in psychiatrist provision of psychotherapy have been recorded. Between 1996–1997 and 2004–2005, the proportion of U.S. outpatient psychiatrist visits involving psychotherapy declined from 44.4% to 28.9% (
5). Increases in the use of pharmaceuticals and changing payment methods have been hypothesized to contribute to this decline (
5).
However, little is known about the state of psychotherapy provision by U.S. psychiatrists from 2006 onward. The Mental Health Parity and Addiction Equity Act (2008) and the Affordable Care Act (2010) have increased mental health care insurance coverage, new pharmaceuticals have expanded treatment options, and advances in evidence-based psychotherapeutic approaches have improved the effectiveness of psychotherapy for several common psychiatric disorders (
6). In light of these changes in the financing and delivery of mental health care and to help fill a gap in our understanding of recent trends in U.S. outpatient psychiatric practice, in this study we analyzed data from the 1996–2016 National Ambulatory Medical Care Survey (NAMCS), focusing on trends and patterns of psychotherapy provision.
METHODS
Data Analysis
We analyzed 21 years of data collected via NAMCS between January 1996 and December 2016 (
7). Each year, the Centers for Disease Control and Prevention’s National Center for Health Statistics fields a multistage probability survey, obtaining a nationally representative sample of outpatient visits to non-federally funded and non-hospital-based physicians’ practices. NAMCS’s sampling design utilizes geographic primary sampling units and stratified secondary sampling of physicians through the comprehensive master files of the American Medical Association and the American Osteopathic Association. For each participating physician, patient visits in a randomly selected week were systematically sampled. Weighting accounted for survey nonresponse, reducing potential response bias (
8). Telehealth, hospital, extended-care institution, and other nonoffice visits were excluded. To facilitate comparison with previous research (
5), community mental health center visits were retained in the main analyses but excluded from sensitivity analyses.
Study Sample
The analyses were restricted to patient visits with psychiatric diagnoses with ICD codes 290–319 (ICD-9-CM) for 1996–2015 or F codes (ICD-10-CM) for 2016. Only visits in which patients saw a psychiatrist were included.
Measures
The main outcome variable was whether psychotherapy was provided. NAMCS defines psychotherapy as “all treatments involving the intentional use of verbal techniques to explore or alter the patient’s emotional life in order to effect symptom reduction or behavior change.” In line with previous research (
5), this broad definition was refined to apply only to visits longer than 30 minutes. Twelve diagnostic categories were analyzed: major depressive disorder, dysthymic disorder, bipolar disorder, other mood disorders, generalized anxiety disorder, panic disorder, OCD, posttraumatic stress disorder (PTSD), social phobia, other anxiety disorders, schizophrenia, and personality disorders (see Table S1 in the
online supplement). Comorbidity was coded when diagnostic categories co-occurred. Prescriptions of up to six medications per visit were coded into four classes of psychotropics: antidepressants, antipsychotics, mood stabilizers, and sedative-hypnotics (see Table S2 in the
online supplement).
Other covariates included patients’ sociodemographic characteristics, including age, gender, race and ethnicity (White, Black or African American, Hispanic or Latino, or other), source of payment (private insurance, Medicare, Medicaid, patient self-pay, or other), office setting (freestanding solo practice, freestanding group practice, or health maintenance organization [HMO]/other), metropolitan or nonmetropolitan location, and region (U.S. Northeast, South, Midwest, or West).
Statistical Analysis
Visit-based analyses were weighted and adjusted using NAMCS’s complex survey design for each year, yielding nationally representative values. For temporal analyses, 1996–1997 versus 2015–2016 comparisons were conducted. A secondary analysis partitioned the study period a priori into three 7-year spans (1996–2002, 2003–2009, and 2010–2016). Risk difference modeling using binomial or multinomial logistic regression similarly adjusted for the complex survey design. Unless specified as multivariate, regression effects were individually modeled. Analyses were performed using the srvyr R package (version 1.0.0) and Stata/MP 16.0 (StataCorp, College Station, Tex.). Confidence intervals were calculated at 95%. Post hoc comparisons were reported after Bonferroni correction. All variables met National Center for Health Statistics reliability standards (≥30 observations per variable). The institutional review board at Columbia University exempted this study.
RESULTS
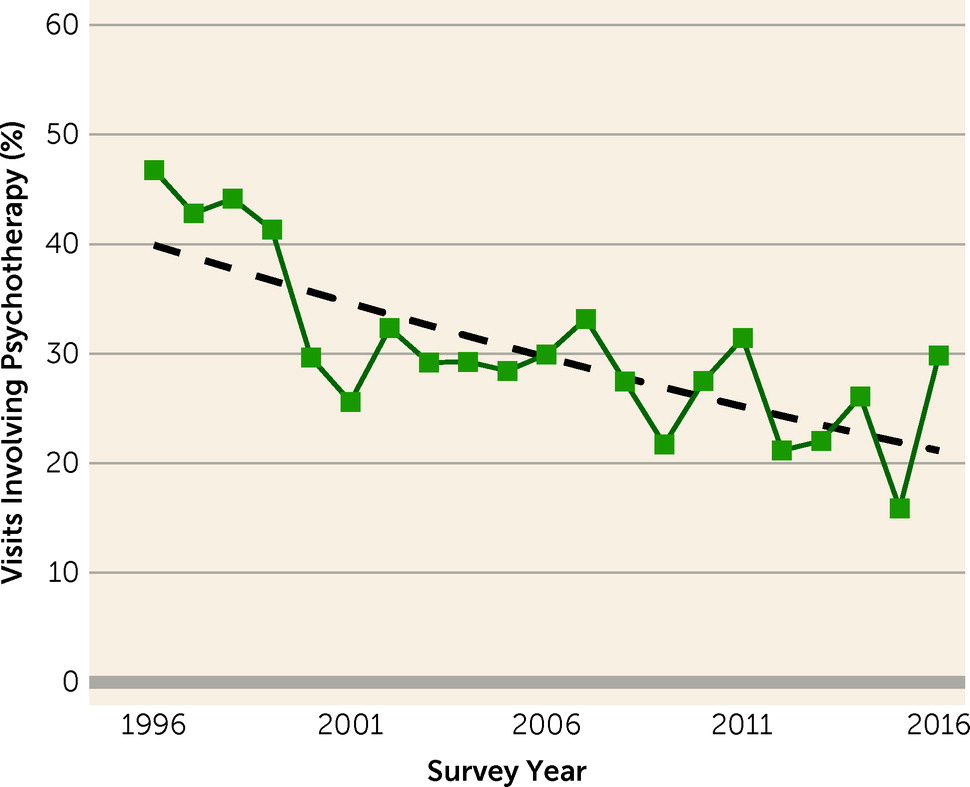
The mean number of physicians surveyed each year between 1996 and 2016 was 1,386; of these, 5.9% were psychiatrists. The overall sampled number of psychiatrist visits was 29,673, representing about 26 million national visits yearly. Logistic regression demonstrated a statistically significant yearly decline in the percentage of psychotherapy visits (risk difference=−0.9%, 95% CI=−1.3, −0.6, p<0.001). Whereas in 1996–1997, psychotherapy was involved in 44.4% of psychiatrist visits, the yearly mean percentages gradually and persistently trended downward, reaching 21.6% by 2015–2016 (
Figure 1).
Analyzing the data as three 7-year spans (1996–2002, 2003–2009, and 2010–2016) and stratifying visits by clinical, sociodemographic, geographic, and financial predictors (
Table 1) revealed a decline in psychiatrist psychotherapy provision in every category examined (for detailed data from this alternative partitioning, see Table S3 in the
online supplement). Except for patients over age 65 and those identifying as non-White and non-Hispanic, significant declines in psychotherapy provision occurred in all sociodemographic groups. Significant declines occurred independently of prescriptions for any psychotropic drug class and comorbidity, and for all diagnoses except schizophrenia. Significant declines were observed in the Northeast, the Midwest, and the South, in metropolitan and nonmetropolitan locations, and in all clinical settings. Sensitivity analyses excluding community mental health center visits did not meaningfully alter results (see Table S4 and Figure S1 in the
online supplement).
Correlates of Psychotherapy
While a downward trend manifested across the board, the likelihood that visits involved psychotherapy was heterogeneous. Modeling individual correlates for psychotherapy provision revealed these disparities (
Table 2). Visits by patients who were under age 25, visits by patients who identified as Black or Hispanic, and visits in which any class of psychotropic medication was prescribed were less likely to involve psychotherapy. Compared with private insurance, Medicare or Medicaid visits were also less likely to involve psychotherapy, yet self-pay visits were more likely to involve psychotherapy. Group practices and HMOs or other settings involved psychotherapy less frequently compared with solo practices. While psychiatric comorbidity was not associated with psychotherapy provision, a diagnosis of dysthymic disorder, OCD, other anxiety disorders, or personality disorders involved psychotherapy more often than other diagnoses, and a diagnosis of major depressive disorder, bipolar disorder, panic disorder, or schizophrenia involved psychotherapy less often. Metropolitan locations and those in the Northeast and the West also involved psychotherapy more frequently. A sensitivity analysis examining only the study years between 2010 and 2016 yielded similar trends (see Table S5 in the
online supplement).
After adjusting for visit characteristics in a multivariate model (
Table 2), a diagnosis of PTSD became significantly associated with psychotherapy provision, and a diagnosis of major depressive disorder or bipolar disorder, prescription for mood stabilizers, and racial identification as Black were no longer statistically significant. For patients who identified as Hispanic, however, psychotherapy provision remained less likely.
After controlling for all modeled visit characteristics, the downward trend through 1996–2016 remained significant and sizable (adjusted risk difference=−0.9%, 95% CI=−1.2, −0.5, p<0.001), indicating that additional unmeasured factors contributed to the decline. The model’s explanatory power increased by 23% through time, indicating that psychotherapy provision became more segregated along modeled covariates (Nagelkerke’s pseudo R2 was 0.26 for 1996–2002, 0.29 for 2003–2009, and 0.32 for 2010–2016). Between 2006 and 2011, NAMCS reported patients’ home zip code median household income and proportion of adults with bachelor’s degrees or higher quartiles. Logistic modeling showed that both variables positively predicted psychotherapy provision, even when controlling for previous covariates (income: adjusted risk difference=3.3%, 95% CI=1.6, 5.1, p<0.001; education: adjusted risk difference=5.8%, 95% CI=4.1, 7.4, p<0.001).
Provider Heterogeneity
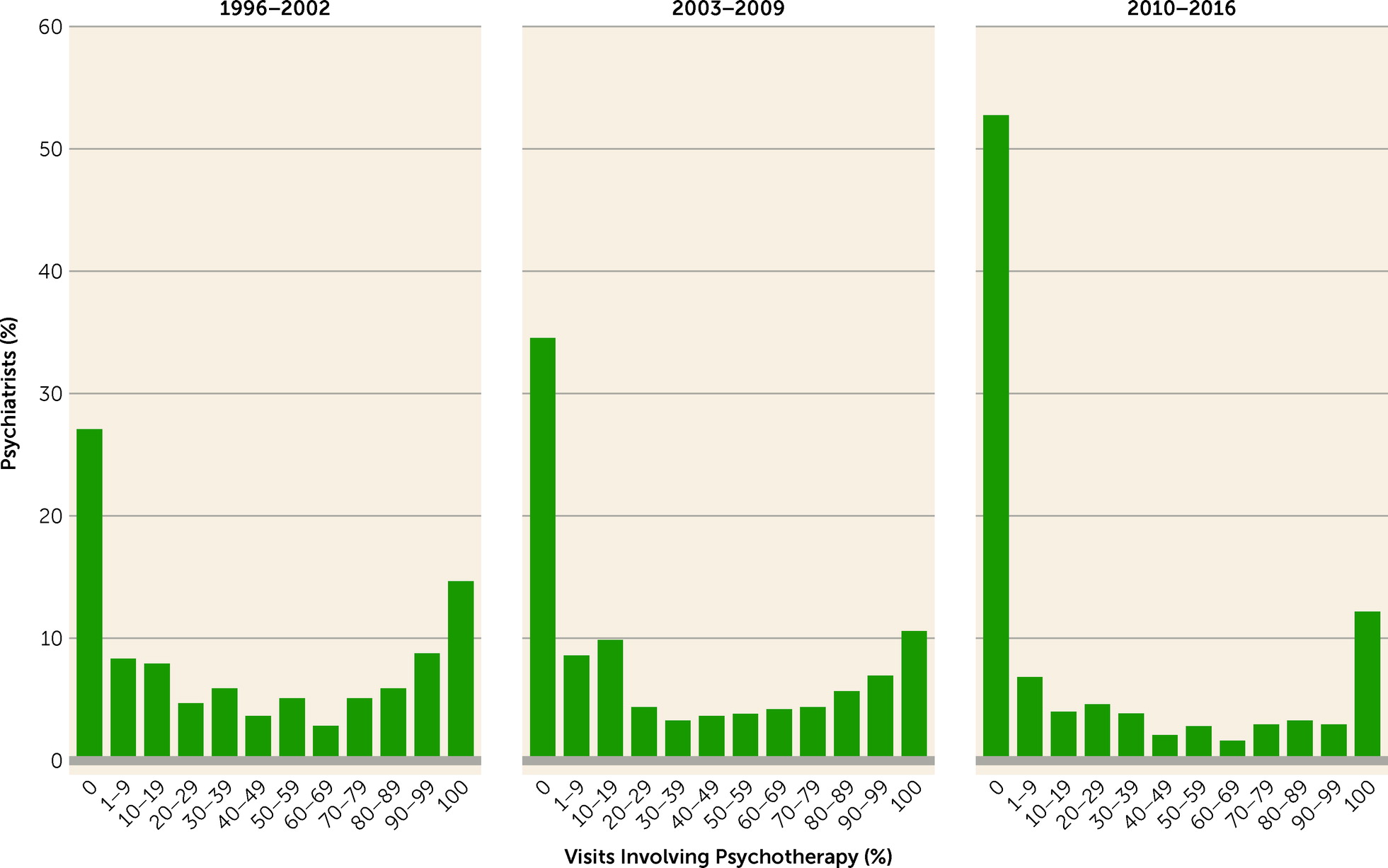
Across the study years, the percentage of psychiatrists providing no psychotherapy in any visit significantly increased (
Figure 2). Between 1996 and 2002, 133 of 491 (27%) sampled psychiatrists provided no psychotherapy; between 2003 and 2009, 189 of 547 (35%) provided no psychotherapy; and between 2010 and 2016, 355 of 673 (53%) provided no psychotherapy. Post hoc chi-square comparisons revealed all pairwise differences to be significant (p<0.001; comparison from 1996–2002 to 2003–2009, p<0.05). By contrast, no significant change was observed in the percentage of psychiatrists providing psychotherapy in all patient visits (1996–2002, 15%; 2003–2009, 11%; and 2010–2016, 12%). Alternative partitioning and provider-level weighting yielded similar results (see Figure S2 in the
online supplement).
Among psychiatrists who practiced psychotherapy in some patient visits, provision significantly decreased as well (risk difference=−0.7%, 95% CI=−1.1, −0.3, p=0.002). For this subgroup, psychotherapy was involved in 44% of visits between 1996 and 2002, 41% between 2003 and 2009, and 34% between 2010 and 2016.
Significant differences in caseload composition were observed between psychiatrists who offered psychotherapy in all visits, some visits, or no visits. Psychiatrists offering no psychotherapy had larger proportions of visits with patients diagnosed with schizophrenia or bipolar disorder (p<0.001). For psychiatrists offering psychotherapy in all visits, caseloads less frequently involved patients with major depression (p=0.04) and more often involved patients with dysthymic disorder (p<0.001), OCD (p=0.005), PTSD (p=0.005), social phobia (p=0.002), other anxiety disorders (p=0.002), and personality disorders (p<0.001). No difference was detected in the proportion of visits with patients with psychiatric comorbidities. These findings remained stable through the study period, and no temporal interactions were detected (see Table S6 in the
online supplement).
A multivariate multinomial logistic regression revealed that with time, visits to psychiatrists who provided psychotherapy in all visits or to those who never provided psychotherapy became more likely, compared with visits to those who occasionally offered psychotherapy (
Table 3). Adjusting for other covariates, treatment by psychiatrists who provided psychotherapy in all visits was associated with patients over age 25, as well as with diagnoses of dysthymic disorder, generalized anxiety disorder, other anxiety disorders, and personality disorders. It was also negatively linked with Medicaid or other, nonspecified payment sources, with non-solo clinic settings, with antidepressant or sedative-hypnotic prescription, and with location in the South. Treatment by psychiatrists offering no psychotherapy at all was associated with location in the South, a non-freestanding clinic setting, and a diagnosis of panic disorder or other mood disorders. It was also negatively associated with patient identification as non-White and non-Hispanic, with a diagnosis of dysthymic disorder, OCD, or personality disorder, and with self-pay.
Adding to the multivariate model (
Table 2) psychiatrist provision of psychotherapy in all visits, in some visits, or in no visits, the effects reported above largely persisted in magnitude and significance. The association with self-pay, however, diminished from an adjusted risk difference of 16.1% (95% CI=11.8, 20.4, p<0.001) to 7.2% (95% CI=2.8, 11.5, p<0.001) (see Table S7 in the
online supplement). This link between patient self-pay and access to psychiatrists who favor psychotherapy highlights the centrality of payment in psychotherapy provision.
Psychotropic Prescription and Integrated Combination Care
During the study period, psychotropics were prescribed in 86% of visits. Whereas nonprescription tripled (in the multivariate model) or quadrupled (in the bivariate model) the odds of involving psychotherapy, 73% of psychotherapy visits involved medications. Of nonpsychotherapy visits, 60% involved antidepressants, and of psychotherapy visits, 52% involved antidepressants (p<0.001). Prescription rates for nonpsychotherapy and psychotherapy visits, respectively, were 28% and 14% (p<0.001) for antipsychotics, 15% and 11% (p<0.001) for mood stabilizers, and 33% and 27% (p<0.001) for sedative-hypnotics. Psychiatrists providing psychotherapy in all visits prescribed medications in 65% of the visits. Between 1996 and 2002, prescription occurred in 66% of psychotherapy visits and in 88% of other visits. Between 2003 and 2009, the percentages rose to 79% (p<0.001) and 93% (p<0.001), respectively, and between 2010 and 2016, they remained stable at 75% (p=0.26) and 92% (p=0.56), respectively. Psychiatrist visits where both pharmacotherapy and psychotherapy were provided declined from 25.4% of visits in 1996–1997 to 13.1% in 2015–2016 (risk difference=−0.6%, 95% CI=−0.8, −0.3, p<0.001).
Frequency of Patient Visits
Since 2007, NAMCS introduced exact counts of patients’ prior visits within the past 12 months (capped at 99 visits). The mean number of visits during the past 12 months among patients receiving psychotherapy was 27.2 (SD=1.6), which was larger (p<0.001) than that of other patients (mean=8.3 [SD=0.3]). Of sampled visits, 2% were by patients with 99 or more annual visits. Of these, 82% involved psychotherapy. Data available since 2014 demonstrate the association between psychotherapy and earlier return appointments: less than 1 week in 23% of psychotherapy visits, compared with 1% of other visits (p<0.001), and 2 months or more in 3% of psychotherapy visits, compared with 33% of other visits (p<0.001). A middle category of return appointments, ranging from 1 week to 2 months between appointments, accounted for 60% of psychotherapy visits and 69% of other visits (p<0.001). No difference was detected in visits where no specific return appointments were scheduled.
DISCUSSION
The downward trend in psychiatrist provision of psychotherapy in outpatient settings in the years 1996–2016 persisted and did not abate. While a small group of psychiatrists (11%−15%) continued to provide psychotherapy in all patient visits, in the 2010s, about half of psychiatrists did not provide psychotherapy at all, and those who provided psychotherapy in some patient visits came to do so more and more rarely. The decline in psychotherapy provision by U.S. psychiatrists may be related to changing economic pressures, as well as to the specialization in prescription of new psychotropic medications.
Although psychotherapy provision declined across almost all clinical groups, patients with severe diagnoses, such as major depressive disorder, bipolar disorder, panic disorder, and schizophrenia, were typically the least likely to receive psychotherapy from their psychiatrists. Differences in the availability of effective pharmacological treatments may help to explain this variation. For example, while for personality disorders, the diagnosis with the highest psychotherapy provision, no medications have indications approved by the U.S. Food and Drug Administration (FDA), for schizophrenia, the diagnosis with the lowest psychotherapy provision, psychiatrists have a range of effective antipsychotic medication options (
9). The association between lower income, education, and other socioeconomic status indicators and some severe mental disorders (
10) may further explain these findings through links between payment source and psychotherapy provision.
During the study period, psychiatrist provision of psychotherapy became more segregated, and declines were especially marked in nonmetropolitan areas, in the South and Midwest regions, and among patients covered by public insurance, including Medicaid. Older, White patients residing in metropolitan areas in the Northeast or West with private insurance or who were self-paying experienced more limited change. These findings harken back to a long tradition of research demonstrating associations between social class and treatment type, with higher-status sociodemographic groups likelier to receive psychotherapy (
11).
Market Forces
Previous research has shown how outpatient reimbursement rates incentivize multiple shorter medication management visits over psychotherapy (
12,
13). Data collected in both 2002 and 2014 estimated a 41% hourly reimbursement gap disfavoring psychotherapy (
14,
15). This, together with insurers’ preference for service provision by lower-reimbursed nonphysician providers when possible (
6), is likely pertinent to the association between payment source and psychotherapy provision. In the present study, self-pay had the strongest association with psychotherapy provision among all sociodemographic, geographic, and financial characteristics examined and, additionally, a significant negative relationship with treatment by psychiatrists not providing psychotherapy at all.
Between 2003 and 2013, the number of practicing psychiatrists declined, exacerbating access constraints in the face of growing demand (
16). Such shortages, disproportionately occurring in rural areas, were associated with treatment using psychopharmacotherapy alone (
17). Despite the increase in mental health care insurance coverage brought about by the Affordable Care Act and the Mental Health Parity and Addiction Equity Act, psychiatrist participation in public insurance programs decreased, and the proportion of psychiatrists only treating self-paying patients increased (
6,
18,
19). The sociodemographic and geographic contours of psychiatrist shortages (
16), which are more acute in lower-income and lower-education localities, in the South and Midwest, and in nonmetropolitan areas, align with those of the downward trend in psychotherapy provision.
Despite many patients’ preference for psychotherapy over medication, most extensively studied in depression and anxiety disorders (
20), a market in which fee structures disincentivize psychiatrists from practicing psychotherapy and in which demand overwhelms supply likely drives some psychiatrists to focus on services that nonphysician professionals are typically unauthorized to provide (
21).
Clinical Considerations
Psychiatrists in the expanding group that offered no psychotherapy typically had more visits involving the most severe diagnoses such as schizophrenia and bipolar disorder. Psychiatrists who provided psychotherapy in all visits had fewer visits involving diagnoses of major depression and more involving dysthymic disorder, personality disorders, OCD, PTSD, social phobia, and other anxiety disorders. Indeed, specific psychotherapies for OCD (
22) and PTSD (
23) are considered first-line treatments. Caseload differences remained stable and did not change throughout the study period.
The study period was also marked by considerable expansions in the number and range of psychotropic medications approved by the FDA in each major class (
24). With the exception of antidepressant prescription, which remained stable, prescription rates for antipsychotics, mood stabilizers, and sedative-hypnotics significantly increased during the study period. After adjusting for other covariates, antidepressants, antipsychotics, and sedative-hypnotics were each negatively associated with psychotherapy provision. The changes in psychotherapy and psychopharmacology provision by psychiatrists coincided with increasing public acceptance of neurobiological attributions of common psychiatric disorders, public endorsement of psychopharmacotherapy use (
25), and rising direct-to-consumer marketing of psychotropic medications (
26).
Psychiatrists who provided psychotherapy in all visits utilized psychotropics less frequently, with prescribing reported in 66% of visits between 2010 and 2016, compared with in 91% of visits reported among psychiatrists who did not provide psychotherapy in all visits (p<0.001). As demonstrated in a previous study, more prevalent use of pharmacotherapy explained much of the decline in the provision of psychotherapy between 1996 and 2005 (
5). Yet, extending the analysis to 2016 revealed that the decline persisted independently of prescription and through the 2010s, when psychiatrists’ prescription rates plateaued. Indeed, pharmacotherapy has largely become the rule in outpatient psychiatry, with psychotherapy typically indicating combination therapy rather than nonprescription (
27).
In outpatient settings for much of the 20th century, psychotherapy was the defining outpatient treatment for a wide range of mental disorders. Since the 1980s, however, the psychiatric profession has shifted toward a more biomedical model of patient care (
28). The ACGME regards psychotherapy as a core competency and requires residents to develop broad psychotherapy skills (
3), yet, often as a result of resource considerations, limited psychotherapy training in many residency programs does not adequately reflect this perspective (
29,
30). Although our study cannot decompose findings regarding the decline in psychotherapy into those due to cohort turnover and those due to individual providers’ changing practices, the decline in psychotherapy practice among psychiatrists offering it occasionally and the rising share of those practicing no psychotherapy at all suggest that both factors may be operative.
Implications
APA’s most recent evidence-based practice guidelines recommend that psychotherapy be provided to patients across diagnoses such as schizophrenia, major depressive disorder, and bipolar disorder, and indeed, combination treatments involving both psychotherapy and pharmacotherapy show superior efficacy for treatment of major depressive disorder, panic disorder, and OCD (
31). State-of-the-art individualized care often requires a combination of treatment modalities for many disorders.
However, not enough is known regarding the challenges and benefits of split (multiple providers) and integrated (single provider) combination care (
32). Despite accreditation requirements for competency in both models, their clinical effects have yet to be sufficiently examined (
33). While increases occurred in the proportion of patients with serious psychological distress receiving psychotherapy from any provider (
34), since 2010, approximately half of psychiatrists no longer practiced any psychotherapy at all. With the exception of older, White, self-paying patients in metropolitan areas in the Northeast and West, access to psychotherapeutic treatments provided by psychiatrists became increasingly scarce. We found that only a small and diminishing percentage of patients received nonsplit combination treatment and that psychiatrists not practicing psychotherapy typically had caseloads involving more severe diagnoses. This may challenge psychiatrists’ unique potential to integrate neurobiological and psychosocial elements of clinical care, a trend whose implications are thus far insufficiently studied.
Limitations
There are several limitations to this study. First, NAMCS codes repeat patient visits as though they are unique, creating a gap between visit and patient counts. Because patients receiving psychotherapy have more annual visits and schedule earlier returns, the actual percentage of psychotherapy patients is likely lower than that of psychotherapy visits. Second, NAMCS response rates are modest, and they declined during the study period. Yet, weighting reduces selection bias (
8), and the uncertainty associated with sample size is reflected in relatively large confidence intervals. Third, the NAMCS definition of psychotherapy does not differentiate between different modalities of psychotherapy, nor does it capture other verbal interventions, which are important to patient-centered care (
35). Refining the definition to visits longer than 30 minutes likely excluded some encounters that included brief psychotherapy. Fourth, these results do not capture changes in psychiatric practice since 2016, psychotherapy visits with nonpsychiatrist health care professionals, visits outside of office-based medical care, or telehealth visits, which have significantly increased during the COVID-19 pandemic (
36). Finally, NAMCS does not provide physician-level weights before 2005; to allow for pre-2005 comparisons, provider-level analyses were unweighted.
CONCLUSIONS
Although psychotherapy provision to U.S. adult patients is stable or rising overall (
34), in part as a result of increases in the allied behavioral health workforce (
37), pharmacotherapy advances and market pressures may have contributed to the continuing decline in psychiatrists’ practice of psychotherapy. Psychiatrist psychotherapy provision rates decreased by more than 50% between 1996 and 2016, and starting in the 2010s, about half of psychiatrists no longer practiced any psychotherapy at all. Psychiatrists not practicing psychotherapy typically saw patients with more severe diagnoses, and while declines affected nearly all patient populations, they were most marked among patients diagnosed with social phobia, dysthymic disorder, and personality disorders. Integrated combination care, in which both psychotherapy and pharmacotherapy are provided by the same practitioner, is most often associated with patient self-pay and is gradually declining. These trends pose a challenge to psychiatrists’ unique role as integrators of biological and psychological dimensions of care, with important implications for the profession and for the delivery of U.S. mental health care as a whole.
Lastly, the COVID-19 pandemic has made mental health care issues even more salient and pressing, with significant increases reported in anxiety and depression symptoms, psychopharmacotherapy use, and psychotherapy use, as well as in the unmet demand for psychotherapy (
38). Although social distancing measures have resulted in a rapid increase in mental health care delivery via telehealth methods, improving some access constraints (
39), these adaptations are unlikely to have reversed the long-term trends analyzed here, and increasing demand for treatment may have even accelerated them.