In 2002 (
1), Bud Craig re-energized scientific interest in interoception (i.e., the processing of sensations coming from inside the body), focusing on the insular cortex and its role in integrating body states, emotion, and awareness (
2). Perceptual accuracy of bodily sensations in the insula was subsequently associated with emotional experience (
3), and insular processing dysfunctions were identified in individuals with anxiety (
4) and depression (
5). More recently, computational approaches (
6) have been used to conceptually and mathematically parse how dysfunction in interoceptive processing leads to mental health problems. For example, within the framework of “interoceptive inference,” descending cortical model predictions are hypothesized to provide top-down inputs to help regulate internal bodily states and thereby adapt the body to the outside world’s demands (
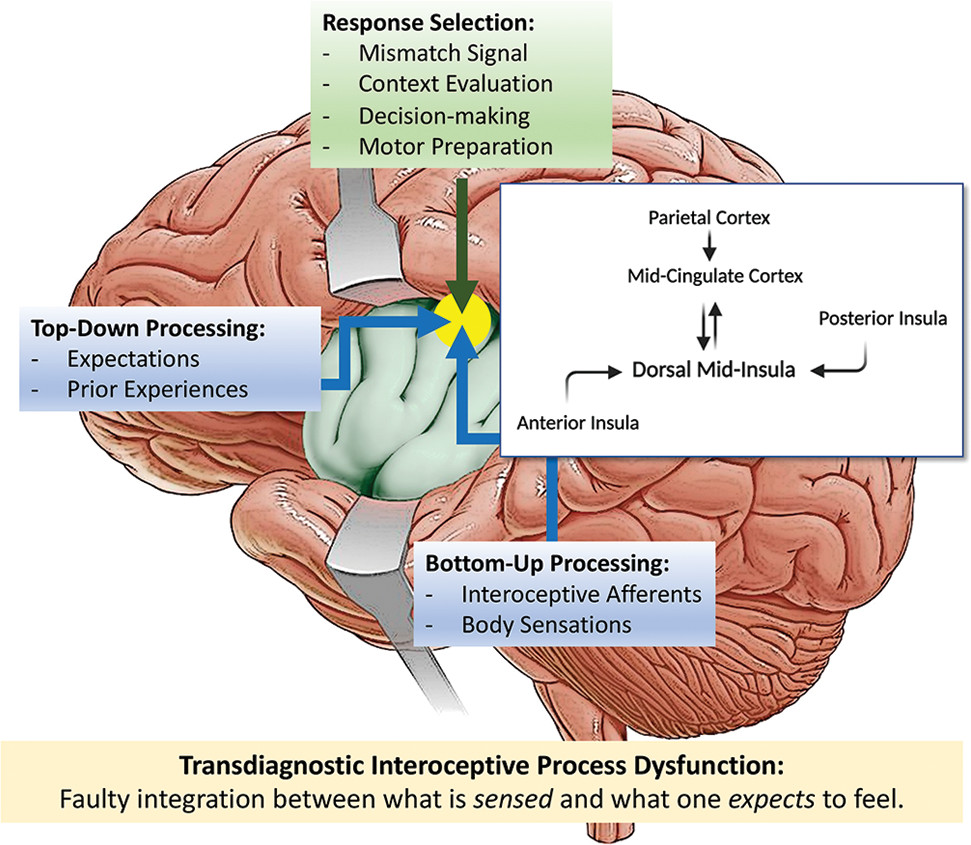
7). The central tenet is that both feeling and action emerges from a tension between what is perceived (at conscious and nonconscious levels) and what is expected via a so-called “interoceptive prediction error” (i.e., the difference between what the brain expects the body signals to be and what the actual body signal afferents are) (
8). The inability to resolve this discrepancy is increasingly recognized as an essential factor contributing to anxiety, mood, eating, substance use, and somatic symptom disorders (
9). In parallel, our anatomical knowledge of the insular cortex has expanded significantly (
10). The mid-insular cortex is uniquely positioned at the interface between ascending sensory information from the posterior insular cortex and descending cognitive or affective information from the anterior insular cortex. It projects primarily to the mid-cingulate cortex (
11), an area important for action selection under motivated conditions such as pain or reward.
The study by Nord and colleagues (
12), in this issue of the
Journal, used a preregistered meta-analytic approach of 33 functional neuroimaging studies of interoception based on 626 individuals with various psychiatric disorders, ranging from mood or anxiety disorders to schizophrenia and bipolar disorder, and 610 healthy comparison participants and asked three questions. First, is there a common “locus of disruption” in the brain underlying interoceptive processing in this group of individuals? Second, is there an overlap between interoceptive processing disruption and affective circuitry as defined by prior meta-analyses? Third, is there an overlap between the interoceptive processing disruption and the neural systems affected by antidepressant treatment across behavioral and pharmacological interventions? The authors identified the left dorsal mid-insula as the common “locus of disruption” (
Figure 1) and emphasized the transdiagnostic importance of this region of the limbic system in interoceptive psychopathology. Several regions with sensory capacities that are not often considered “interoceptive” yielded some signal, although at a statistically uncorrected threshold. These areas included the caudate, cerebellum, dorsolateral prefrontal cortex, and precentral gyrus and could be targets of exploration for their role in interoceptive processing and its dysfunction. However, there was no overlap with either the common brain structures involved in affective circuitry or those that change with antidepressant treatment. The authors speculate that the hybrid cytoarchitecture of the mid-insula (i.e., between the six-layered iso-cortex and three- to four-layered allo-cortex) makes this a candidate for interoceptive prediction-error encoding in individuals with psychiatric disorders. This process is not necessarily aligned with some of the other affective dysfunctions and may currently not be a primary intervention target.
This meta-analysis advances the field in several ways. First, it focuses on an anatomical part of the insula that has not yet been widely appreciated. Although the anterior insula had been reported as among the central anatomical structures involved in structural (
13) and functional (
14) abnormalities in psychiatric disorders, the mid-insula has not yet been widely recognized for its major role in integrating interoceptive processing with motivated behavior. Second, the analysis revealed that there is a need to reconceptualize mid-insula dysfunction in terms of the underlying processes but also in terms of modulating it as a treatment target. It is now better understood that the most crucial connection of the mid-insular cortex is to the mid-cingulate cortex (
11), which puts it at the heart of feedback-mediated decision-making processes. The mid-cingulate region is associated with cognitive control, decision making, fear, and pain, and it is central to cognitive and affective integration (
15). This integration process begins with the sensing of interoceptive (e.g., breathing) and exteroceptive sensory afferents (e.g., audio-visual cues), which provide an instant comparison between what is expected and what is being sensed to generate a very early set-shift signal. For example, shallow frequent breathing in a dark alleyway might provoke an individual to engage in fight/flight behavior upon hearing a sudden noise. If the noise turned out to be a cat and not an assailant, the associated error signal could modify memory, expectations, and the motor plan via an error-driven feedback mechanism, which involves integrating body-relevant information with the selection of action-outcome behaviors. However, disrupted integration of body-relevant information with action-outcome behavior selection would not simply map onto affective processing per se or to interventions targeted at altering affective processing, as shown by this study. Our group has recently proposed that interoceptive psychopathology can arise in two ways (
16): first, individuals may have abnormally strong expectations of the situations that elicit internal bodily change (i.e., hyperprecise priors). For example, an anxious individual encountering a cat instead of an assailant in a dark alley at night might not adjust their behavior or emotional experience due to the overwhelming conviction that a sudden sound together with shallow breathing indicates ensuing assault. Second, individuals may have great difficulty adjusting these expectations when the environment changes (i.e., context rigidity). Upon emerging into a brightly lit open space, the anxious individual may continue feeling threatened due to the maintenance of the same model (shallow breathing and sudden noises signal impending assault) despite the new context. This model of psychopathology assumes that for optimizing bodily functioning, the nervous system needs to develop an accurate model of the world. In that regard, the meta-analytic finding of disrupted mid-insular cortex processing in various psychiatric disorders could be viewed as evidence for a reduced ability to match the model to how the body is feeling or vice versa, at least at the level of the brain.
Several problems need to be solved to make this finding actionable for mental health practitioners. First, longitudinal studies will need to examine whether the mid-insular “locus of disruption” is a preexisting condition that facilitates the emergence of a psychiatric disorder or whether it is a consequence of mental health problems. One could envision that inadequate integration of body-relevant signals into decision making, and motivated behaviors, could result in a greater risk of specific psychiatric disorders. For example, not experiencing or attending to body sensations when engaging in “risky” behaviors, such as drug-taking, might predispose individuals to expose themselves further to risky situations associated with psychiatric disorder onset (e.g., repeated drug use). On the other hand, the occurrence of a psychiatric disorder may shift an individual’s motivated engagement with his or her surroundings in ways that produce a dysfunctional integration of those body-relevant signals that facilitate decision making. Second, could a mid-insular locus of disruption be modified by interventions that restore adequate function? Nord and colleagues argue that the mid-insula cluster is spatially distinct from both general affect circuitry and brain regions that have been implicated in evidence-based psychological and pharmacological treatments for affective conditions. Thus, would this require novel approaches that specifically attempt to regulate the mid-insula? Future studies may need to employ focused neuromodulation or real-time functional MRI neurofeedback to determine the modifiability of this area and evaluate whether this anatomically identified processing disruption can be a treatment target. Third, more refined approaches will be necessary to precisely delineate the nature of the dysfunction that is mediated by this circuitry. The authors are clear that this meta-analytic approach does not provide a mechanistic accounting of the physiological functioning of the identified neural tissues. By aggregating studies across different sensory functions (e.g., nociceptive stimulation, inspiratory loaded breathing stimulation, resting heartbeat attention, sensual touch stimulation, etc.), this study cannot determine the functional role of the mid-insula (or any other cortical/subcortical regions) in orchestrating specific aspects of interoception, such as nonconscious versus conscious processing, stimulus intensity decoding, or metacognitive insight.
Nord and colleagues focus on an important area of psychiatry that is generating interest but one that has been understudied. There is emerging interest in interoceptive neuroscience (
17), an interdisciplinary space replete with essential discoveries in both the basic and clinical spheres. Computational approaches (
18), based on the notion that interoceptive processing is vital for maintaining homeostasis by continually making predictions about future body states and adjusting behavior accordingly, may provide a transformative basis for refining our understanding of the affected processes in psychiatric disorders. Collectively, such approaches may ultimately lead to a new language and precise clinical tools that help us to better define what happens when you don’t feel right inside.