In case-control studies, cannabis users exhibit subtle cognitive deficits and structural brain differences (
1,
2). These findings come largely from studies of adolescents and young adults (
3,
4). It is unclear whether the subtle cognitive and brain differences observed in young cannabis users might be larger in midlife and older adult cannabis users with longer histories of use (
5). This issue is timely because cannabis use is increasing among baby boomers (born 1946–1964), a group who used cannabis at historically high rates as young adults (
6) and who now use cannabis at historically high rates as midlife and older adults (
7). This issue is important because mild cognitive deficits and greater hippocampal atrophy in midlife are risk factors for later dementia (
8,
9).
We identified four longitudinal studies and seven cross-sectional studies that reported on cannabis users in midlife or older adulthood (
3,
10–
19) (see Table S1 in the
online supplement). Limitations include use of crude or retrospective measures of cannabis exposure and a lack of neuroimaging data. Further, the studies did not address four questions of policy significance. First, are all midlife and older adult cannabis users at risk? Older adults in the United States are increasingly using cannabis (
7), but only 10%−15% of users are cannabis dependent (
20). Distinguishing problem and non–problem users is important, because non–problem users may not differ from nonusers. Second, are cognitive deficits and brain differences among cannabis users minor compared with those observed for alcohol or tobacco users, as some proponents of cannabis legalization claim (
21)? Third, do differences among cannabis users persist after cessation? If so, these differences could increase risk for dementia. Fourth, do brain differences among long-term cannabis users underlie cognitive deficits? Brain differences, if observed, are inconsistently related to cognitive deficits in adolescent and young adult cannabis users. Research is needed in midlife and older adult cannabis users.
We addressed these questions by assessing cannabis use, cognitive function, and hippocampal volume in a population-representative cohort followed prospectively from birth to age 45. We compared long-term cannabis users against five groups: 1) lifelong cannabis nonusers (to replicate the control group most often reported in the case-control literature); 2) midlife recreational cannabis users (to ascertain whether cognitive deficits and structural brain differences are apparent in non–problem users—the majority of cannabis users); 3) long-term tobacco users and 4) long-term alcohol users (to serve as benchmark comparisons for any cannabis findings and to help disentangle potential cannabis effects from tobacco and alcohol effects); and 5) cannabis quitters (to ascertain whether differences are apparent after cessation).
Discussion
This prospective study followed a population-representative birth cohort for 45 years, generating a unique evidence base for evaluating whether long-term cannabis users show cognitive deficits and smaller hippocampal volume in midlife. The longitudinal design enabled a comparison of a person’s midlife cognitive abilities to their childhood cognitive abilities before cannabis initiation. The study also enabled a test of the role of hippocampal gray matter volume in mediating associations between long-term cannabis use and cognitive deficits. Six findings stand out.
First, long-term cannabis users exhibited IQ decline and poorer learning and processing speed in midlife relative to their childhood IQ. People who knew them well described them as having memory and attention problems. These associations were not explained by prospectively assessed persistent tobacco, alcohol, and other illicit drug dependence or by childhood socioeconomic status, low childhood self-control, and family substance dependence history. Associations were also not explained by recent cannabis use. Findings were consistent across two cannabis exposures (persistence of cannabis dependence, persistence of regular use) and in tests comparing long-term cannabis users to five comparison groups (cannabis nonusers, tobacco users, alcohol users, recreational cannabis users, and cannabis quitters). (Table S11 in the
online supplement summarizes findings across tests of dose-response associations and group comparisons.) This suggests that cannabis-related IQ decline, poorer learning and processing speed, and informant-reported memory and attention problems are not artifacts of analytic approach or of measured confounders, but rather are more likely to be consequences of long-term use. Cognitive childhood-to-adulthood changes such as those we observed have been shown to predict steeper cognitive decline from ages 70 to 82, and to do so better than adult cognitive level (
39).
Second, long-term cannabis users showed significantly larger IQ decline, poorer learning and memory, and poorer processing speed than long-term tobacco or alcohol users. Thus, some cognitive deficits were more pronounced for long-term cannabis users than for long-term tobacco or alcohol users, contrary to some claims (
21,
40).
Third, cognitive functioning among midlife recreational cannabis users was similar to representative cohort norms. This suggests that infrequent, non–problem recreational cannabis use in midlife is unlikely to compromise cognitive functioning. Our results highlight the importance of not conflating long-term and recreational cannabis users in future studies.
Fourth, cannabis quitters showed subtle cognitive deficits that may explain inconsistent findings on the benefits of cessation (
11,
14,
41–
45).
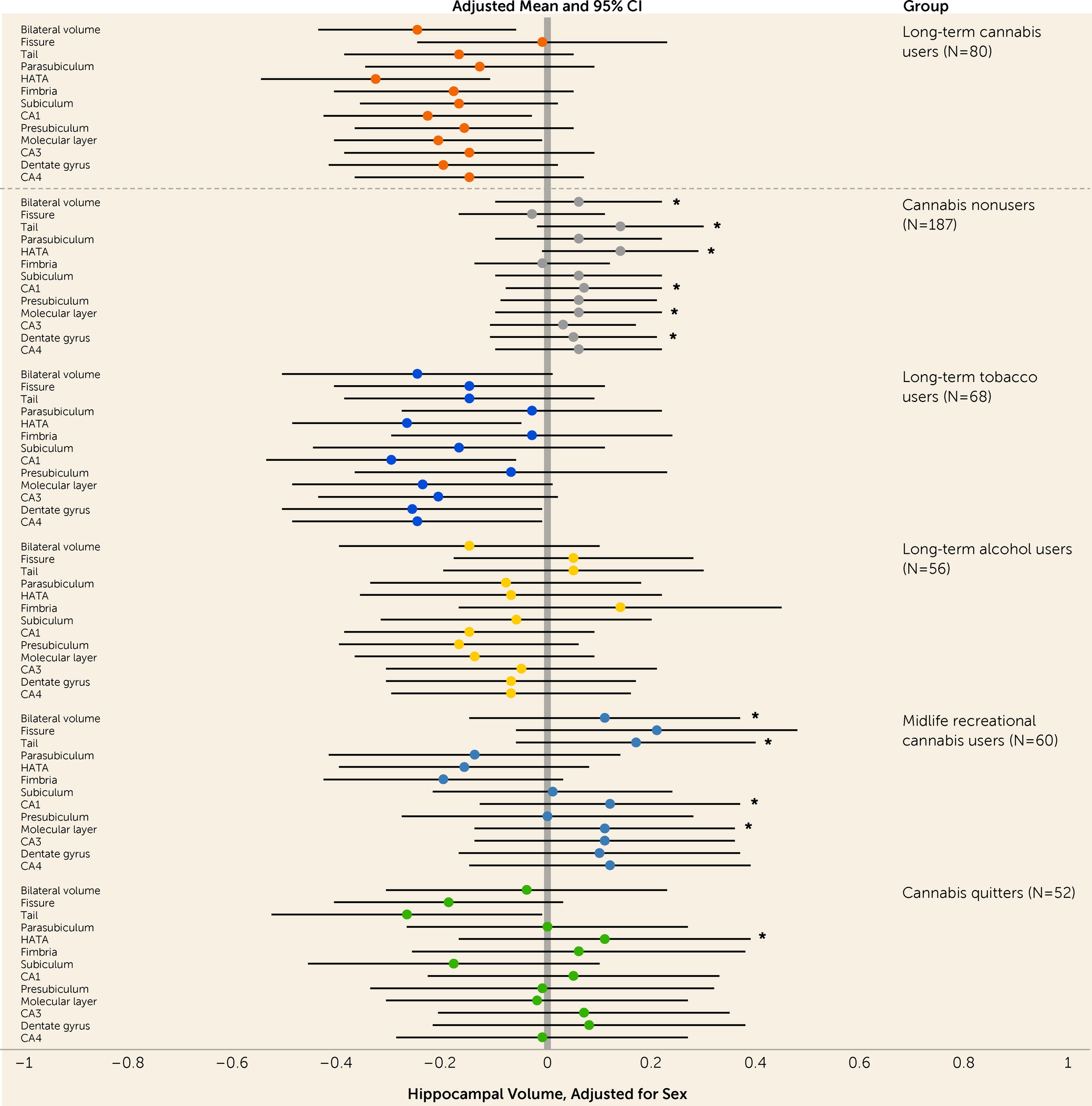
Fifth, long-term cannabis users showed smaller bilateral volume in total hippocampus and five of 12 structurally and functionally distinct subregions compared with nonusers, consistent with case-control studies (
2).
Sixth, although persistence of cannabis use showed dose-response associations with cognitive deficits and, to a lesser extent, smaller hippocampal volume in the representative sample, smaller hippocampal volume did not statistically mediate associations between persistence of cannabis use and cognitive deficits. Smaller hippocampal volume has been suggested as a possible mediator of cannabis-related cognitive deficits (
24), because the hippocampus is rich in type 1 cannabinoid (CB1) receptors and is involved in learning and memory. However, smaller hippocampal volume may be a reductionistic explanation for cannabis-related cognitive deficits. For example, in addition to the hippocampus, other CB1-rich brain regions, including those involved in reward and motivation, may play a role (
2). Further, neurobiological mechanisms likely extend beyond gray matter volume differences to include differences in structural and functional connectivity (
46). Finally, social mechanisms could also play a role.
Our findings conflict with those of some studies (including one by us) that compared the cognitive functioning of twins who were discordant for cannabis use and found little evidence of cannabis-related cognitive deficits (
47–
50). Discordant twin comparisons represent a compelling approach to controlling for shared genetics and family background. However, a limitation is that the size of the differences between twins in cannabis use and in cognitive functioning is much smaller than between unrelated individuals. Hence, it is unclear whether associations that are attenuated in twin-difference comparisons, relative to comparisons between unrelated individuals, are an indication of true confounding or are an artifact of reduced statistical power.
In the present study, we tackled confounding by incorporating the most notable confounding variables identified in the literature, including childhood socioeconomic status, low self-control, low childhood IQ, family substance dependence history, and persistent dependence on other substances, using unusually strong measures derived from multiple waves and data sources. These obvious confounders, considered together, could not account for many of the observed associations. We also reported E-values, with larger E-values indicating that considerable unmeasured confounding would be needed to explain associations. E-values ranged from 1.33 to 1.56. These E-values represent the risk ratios needed after adjustment for measured confounders, raising the bar for unmeasured confounding to play a role.
This study has several limitations. First, cannabis use was self-reported. Underreporting for fear of admitting to illegal drug use is unlikely because participants were interviewed repeatedly over a lifetime and learned to trust the confidentiality guarantee. Second, some group sizes were small, raising concerns about low statistical power. These concerns were minimized through powerful tests of dose-response associations and through transparent reporting of effect sizes in a representative cohort. Third, long-term cannabis users also use tobacco, alcohol, and other illicit drugs. Disentangling cannabis effects from other substances is challenging. We did not limit analyses to cannabis-only users because they are unrepresentative of cannabis users (
51). Instead, we used two complementary approaches: 1) we reported no midlife cognitive deficits for long-term tobacco and alcohol users, groups who showed polysubstance use, like long-term cannabis users, but were free from cannabis, and 2) we controlled for persistent dependence on tobacco, alcohol, and other illicit drugs in analyses of dose-response associations and found that a number of associations were robust to covariate control. Collectively, the findings suggest that use of other substances cannot fully account for the cognitive deficits observed in long-term cannabis users.
Fourth, we focused on hippocampal volume as a key MRI outcome based on theory and previous research (
2). We are preparing a separate report with results of exploratory analyses of associations between long-term cannabis use and comprehensive MRI measures of global and regional gray and white matter. Fifth, the results are based on a single birth cohort who began using cannabis in the 1980s or 1990s. The concentration of THC, the psychoactive constituent of cannabis, has risen in recent years (
52). Therefore, if THC exposure underlies associations, we may have underestimated effect sizes in contemporary users. Finally, observational studies cannot conclusively demonstrate causality.
This study has notable implications. First, long-term cannabis use is robustly associated with cognitive deficits in midlife. These may be consequential given that mild cognitive deficits in midlife are a risk factor for dementia (
8). The deficits we observed are comparable to midlife cognitive deficits of individuals who developed dementia in the Atherosclerosis Risk in Communities Study (
8). Older adults who developed dementia showed midlife cognitive deficits that ranged from 0.32 to 0.53 standard deviations below the cohort mean on tests of memory, processing speed, and word fluency. Second, research is needed to ascertain whether long-term cannabis users show elevated rates of dementia in later life. This is important given the huge burden of dementia, and it is timely given the confluence of two trends: the growth of the aging population, and the record high rates of cannabis use among today’s older adults.