To the editor: Psilocybin has reemerged as a promising treatment for depression (
1). Currently, it is assumed that psilocybin’s therapeutic effects require a psychedelic “trip” that is mediated via serotonin 2A (5-HT
2A) receptor activation (
1). However, recent preclinical animal models demonstrated antidepressant-like behavioral effects and synaptic actions of psilocybin independent of 5-HT
2A receptor activation, suggesting that altered perception may not be necessary for therapeutic benefits (
2). We report here the first case of an adult with treatment-resistant depression (TRD) who was administered psilocybin after premedicating with a potent 5-HT
2A receptor antagonist, namely, trazodone.
“Mr. A” is a 45-year-old man with a long history of TRD failing to respond to several medications (i.e., sertraline, levomilnacipran, bupropion, mirtazapine, desvenlafaxine, duloxetine, venlafaxine, aripiprazole, vortioxetine, vilazodone, cannabis oil, trazodone, intranasal esketamine, and intravenous ketamine) and multiple years of evidence-based psychotherapies. He was enrolled in an ongoing trial (
3) evaluating the antidepressant effects of 25 mg oral psilocybin (open label with all participants receiving psilocybin) combined with brief supportive psychotherapy. He reported discontinuing all psychotropic medications 2 months prior to entering the trial. The patient provided written consent for this case report publication in addition to the consent provided for trial participation.
The patient underwent a psilocybin session and reported feeling no psychoactive effects. Throughout the 8-hour dosing session no psychedelic effects were reported by the participant or observed by the therapists. Subjective and objective scales detected no psychoactive effects, and no psychotomimetic or dissociative effects were detected during or after the dosing session. Both the participant and the therapists were surprised, and the participant reported feeling “disappointed” that no psychedelic effects were observed. After two integration sessions in the following week, he did not receive any further therapy throughout the 6-month observational period, as per the trial protocol.
At the 6-week follow-up visit, Mr. A disclosed that he continued to take trazodone 200 mg each night for sleep leading up to the dosing session, despite being told to stop this medication 30 days prior to his dosing session. Given that Mr. A’s last dose of trazodone was taken within 12 hours of psilocybin administration, serum levels would likely be sufficient to still occupy 5-HT
2A receptors by >90% (
4,
5), almost entirely blocking psilocybin from binding this target receptor during the dosing session.
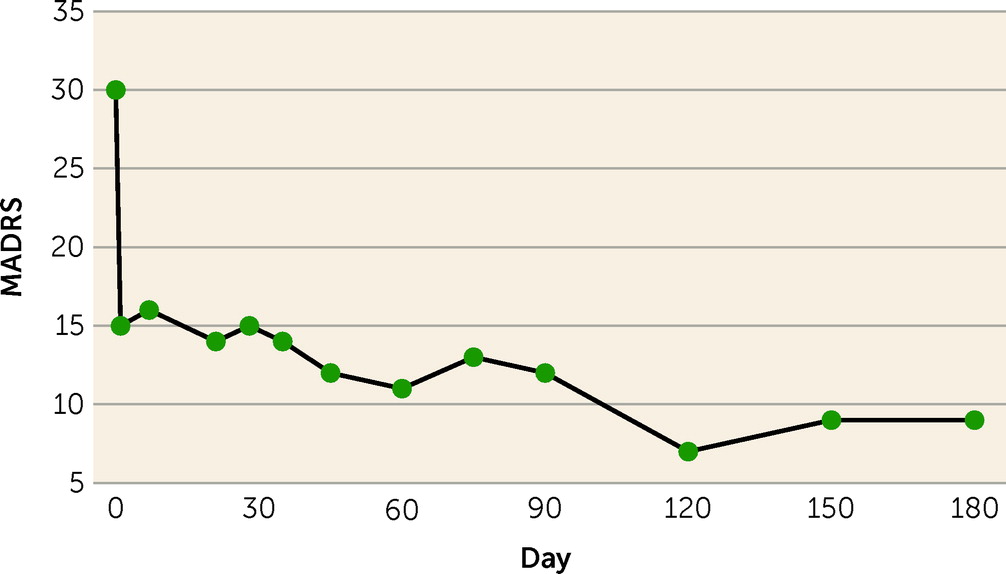
Despite the absence of psilocybin’s psychedelic effects, Mr. A experienced rapid, robust, and sustained antidepressant effects, reporting that this was the first time he had experienced true, full remission of his depression in over 8 years. Clinician-rated depressive symptoms, as measured by the Montgomery-Åsberg Depression Rating Scale (MADRS), corresponded well with the subjective global impression, decreasing from a MADRS score of 30 at baseline to a score of 15 the day after the psilocybin dosing session. This reduction was maintained, with MADRS scores ranging from 7 to 12 throughout the 6-month observational period (
Figure 1).
This case suggests that the mechanism of antidepressant action of psilocybin may be independent of 5-HT2A receptor activation and psychedelic effects. However, a single case report must be interpreted cautiously, and prospective clinical trials are needed to determine the potential 5-HT2A–independent antidepressant effects of psilocybin, with major implications for scalability and acceptability.