A reporter once allegedly asked the infamous bank robber, Willie Sutton, why he robbed banks. Sutton’s response was “Because that’s where the money is” (
1).
Using postmortem human brain to elucidate the molecular biology of brain disease is a strategy consistent with Sutton’s Law. The work of Ehringer and Hornykiewicz, which found decreased dopamine in the striatum of postmortem brains of patients with Parkinson’s disease (
2), was a resounding demonstration of the wisdom of this strategy. It paved the way for the use of
l-dopa, the metabolic precursor of dopamine, in the treatment of Parkinson’s disease (
3). As dramatic as these findings were for neurology, it had a significant impact on the early postmortem brain studies of schizophrenia, which focused heavily on monoamines and their receptors (
4–
6). While the dramatic success of this approach for Parkinson’s disease has not been matched as yet in psychiatric disorders, postmortem brain studies of schizophrenia have pushed ahead with a number of novel hypotheses propelled by advances from the Human Genome Project (
7,
8) and the Psychiatric Genomics Consortium (
9). While studies related to risk variants for schizophrenia have involved hundreds of postmortem brains (
10,
11), smaller, cellular-level studies have complemented this approach, as referenced in an article by Dienel et al. in this issue (
12) entitled “The Nature of Prefrontal Cortical GABA Neuron Alterations in Schizophrenia: Markedly Lower Somatostatin and Parvalbumin Gene Expression Without Missing Neurons.”
The article includes a scholarly review of highly interesting and relevant areas of research for schizophrenia. First, it reminds the reader of the import of the prefrontal cortex for the cognitive deficits that characterize schizophrenia. Second, it reviews the numerous postmortem brain studies that have led to this study of GABA neurons in the dorsolateral prefrontal cortex (DLPFC), including the definitive stereological study of the number of neurons in the prefrontal cortex of patients with schizophrenia, conducted by Bente Pakkenberg (
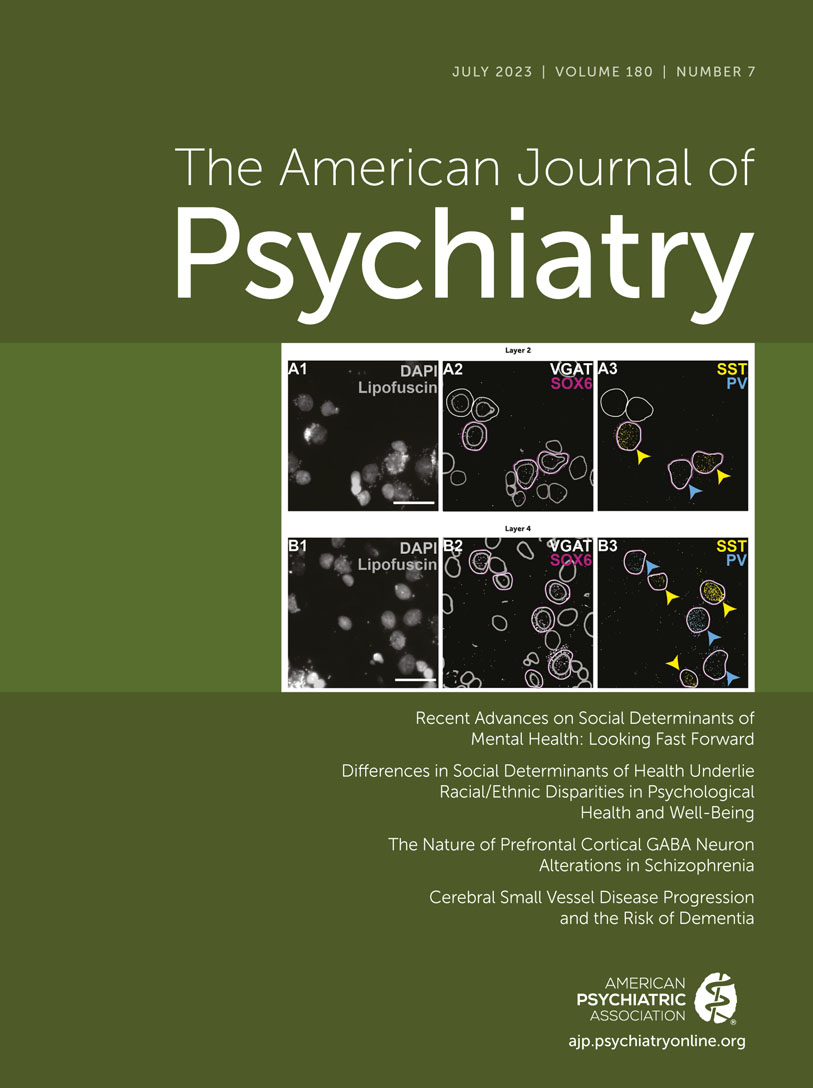
12). This latest study uses a novel multiplex fluorescent in situ hybridization technique to reveal that lower somatostatin and parvalbumin levels in layers 2 and 4 of the DLPFC are secondary to lower levels per neuron, not to decreased numbers of neurons. The study compares 30 patients with schizophrenia and 30 neurotypical control subjects, matched for sex, race, age, postmortem interval, body mass index, RNA integrity number (a measure of RNA quality), and tissue storage time. Although the samples were not matched for comorbid substance abuse (including nicotine) or manner of death (including suicide), analyses of these confounders in subgroups of the patients have suggested that they are not causative of the differences seen between patients and control subjects.
A second measure of RNA integrity in this study is pH, which differed significantly between the patients (mean pH, 6.5) and the control subjects (mean pH, 6.7). Although the authors characterize the 0.2 difference as “of uncertain biological significance,” it is a log measurement of acidity (about a 1.5-fold difference), and antipsychotics have been shown to decrease brain pH, which is associated with decreased RNA expression secondary to degradation (
13). Neither animal studies using antipsychotics nor studies using a group with bipolar disorder as an antipsychotic control adequately mitigate this postmortem confounder. The remedy lies in a methodological correction, which uses postmortem human brain degradation studies, referred to as qSVA (quantitative surrogate variable analysis), to control for this and other occult confounders (
14). Antemortem antipsychotic treatment is associated with numerous genes showing differential expression in postmortem human brain, as demonstrated most recently in a study involving the striatum (
15). We have also looked at this in DLPFC, where at least 2,000 genes are affected by antemortem antipsychotic treatment (
10). The data from the Dienel et al. study to some degree support this notion, insofar as Figures S6 and S7 in the article’s online supplement show a trend for an antipsychotic drug effect. The number of antipsychotic-negative patients was small (N=3), however, and probably none were antipsychotic naive (
12). It will be interesting to see how emerging large-scale single-nuclei studies support these findings. In this regard, preliminary data from a recent single-nuclei study of DLPFC in schizophrenia did not show differential expression of either parvalbumin or somatostatin in GABA neurons (
16). To be certain, the lower pH is a potential confounder only for the original finding of decreased somatostatin and parvalbumin, while the most important finding in this study is that there is no loss of GABA neurons in cortical layers 2 and 4 of the DLPFC of brains of patients with schizophrenia.
These considerations notwithstanding, it would be fair for the reader to ask, “Why does this matter?” The normal number of neurons in the DLPFC of brains of patients with schizophrenia is an argument against the notion that these reductions in somatostatin and parvalbumin in the cortical GABA neurons are related to the death of neurons and/or abnormal migration, hypotheses reviewed by Dienel et al. to elucidate the neuropathology of schizophrenia (
12). Moreover, the authors contend that this makes the prospect for treatment of these abnormalities that much more likely, not unlike the advances seen in the treatment of Parkinson’s disease. This is certainly a reasonable conclusion from this study, but other questions remain only partially addressed, particularly whether the effects are related to prior treatment.
If the lower levels of somatostatin and parvalbumin in the DLPFC of patients with schizophrenia are not related to a loss of neurons and/or abnormal migration or epiphenomena of chronic illness, what are they caused by? Is it genes, or environment, or both? This study focuses on the excitatory input to GABA neurons in DLPFC. A number of molecular candidates are discussed, including ErbB4 and
N-methyl-
d-aspartate receptors (NMDARs), both of which could be related to hypothesized decreased excitatory input to GABA neurons. One way to test these hypotheses is to look for relationships between the expression of ErbB4 and/or NMDARs or genetic variants known to affect expression of these genes in the same specimens used for this study. It also would be of interest to examine genetic variants identified by the Psychiatric Genomics Consortium that are known to increase risk for schizophrenia (
9). This is certainly not expensive, and it might shed some light on what, if any, of the genetic risk variants for schizophrenia are related to the interesting and important observations made in this study.