The ketamine tiger remains untamed. Sixty years ago, the first human experiments with ketamine revealed an anesthetic drug with a remarkably favorable cardiopulmonary profile but odd dissociative features (
1). Ketamine then quickly gained popularity for its utility as a perioperative analgesic. In 2000, ketamine reincarnated into the field of psychiatry as the prototype rapid-acting antidepressant (
2). Now, in this issue of the
Journal, Hess et al. (
3) sidestep a simmering debate about whether ketamine’s psychoactive effects merit inclusion with “classical” psychedelics (e.g., psilocybin and LSD) and show that ketamine can produce prosocial effects in both rats and humans that are much closer to an altogether different psychopharmacological category, that of entactogens, best known by the exemplar MDMA (3,4-methylenedioxymethamphetamine). MDMA, also historically called an “empathogen,” produces feelings of closeness and an increased sense of empathy, and allows access to traumatic memories without triggering an aversive response, the latter responsible for the “entactogen” label, meaning “touching within” (
4). Ketamine, classical psychedelics, and entactogens have a few things in common: they are powerfully psychoactive, they act rapidly across an array of psychiatric disorders, and their effects appear to be durable, long outlasting the acute drug experience. What they do not share is a primary molecular target (e.g., a receptor) or (for most of these compounds) a high degree of pharmacological specificity. So, despite our best efforts to classify ketamine into receptor-oriented categories (
5,
6), experimental data once again force us to question whether a molecular target–based taxonomy, well suited for cardiovascular medications and novel antibiotics, meaningfully captures the effects and clinical potential of ketamine, let alone other emerging therapeutics for mental health.
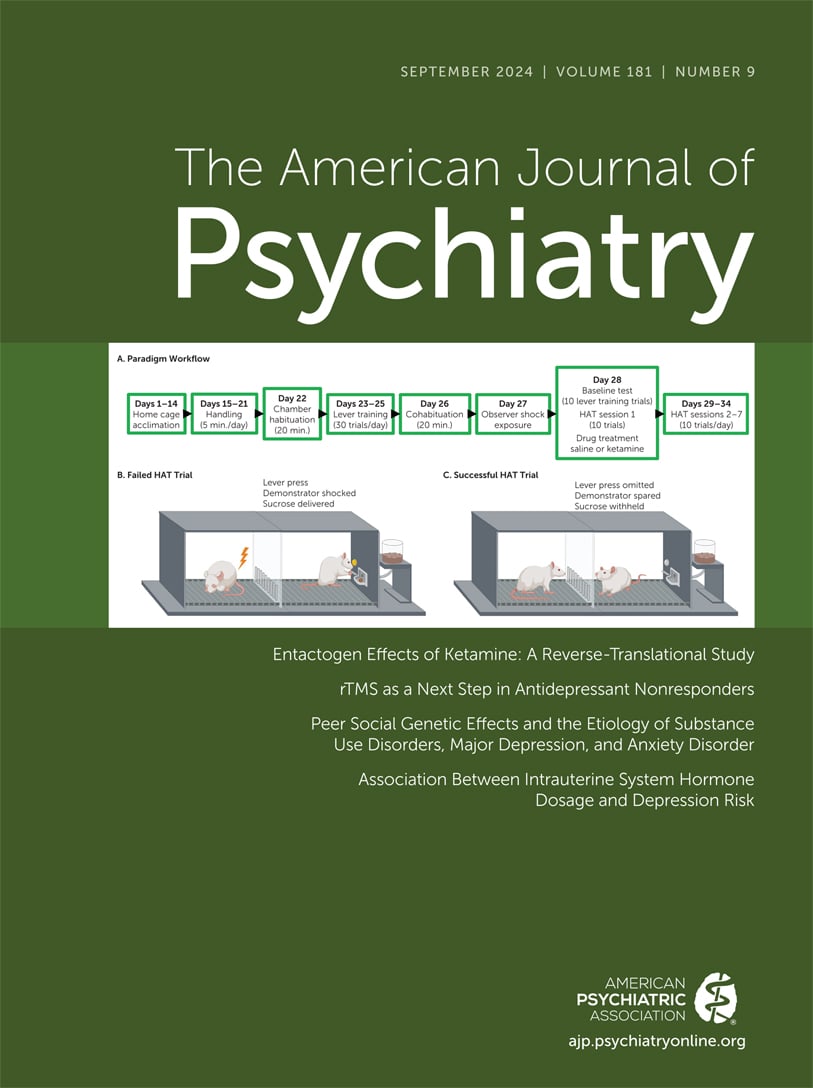
The study begins with a familiar experiment: patients with depression were treated with a single infusion of racemic ketamine. However, in addition to standard depression rating scales, the authors focused on improvements in ratings on questionnaire items reflecting reduced pleasure associated with social situations, an often underappreciated dimension of depression. Theorizing that these responses may reflect an underlying improvement in empathy, meaning one’s ability to intuit the internal affective state of another, the authors then developed a behavioral task to model the potential prosocial effects of ketamine in rats. “Observer” rats, who had previously experienced shocks, learned that pressing a lever does two things: it nets the observer a sugar pellet and it delivers a shock to an adjacent compartment housing a “demonstrator” rat. Remarkably, a single, roughly human-equivalent antidepressant dose of ketamine given to observer rats was followed by an abrupt and sustained reduction in lever pressing, compared to behavior following a control vehicle injection. The reduced lever pressing could be explained in a few ways. First, shocking the demonstrator imposes a new cost to the observer’s lever press: the observer’s sensory experience of a rat being shocked next door could be a deterrent to reward seeking, akin to hearing a noisy neighbor bang on the wall every time you turn up the music. A second possibility is that the observer, knowing how a shock feels, intuits the distressed internal state of the demonstrator; omitting a lever press could alleviate the observer’s own empathic distress. Reframed in terms of helping behavior, sparing the demonstrator by omitting a lever press could provide a natural reward to the observer, reducing the need or desire for a sucrose reward. A third possibility, that ketamine reduced the intrinsic value of sugar reward, is essentially ruled out by the investigators based on the time rats spent in proximity to the lever, consistent with a substantial literature testing ketamine and sucrose reward.
The translational platform used in this work is truly innovative, and it is a beautiful example of how complementary experiments across species can potentially fill in the gaps of interpretation. As the authors indicate, there is more work to be done to solidify the claim that humans and rats show increased
empathy after ketamine and to elucidate the mechanisms of this effect, particularly the extent to which these effects and mechanisms are equivalent to those induced by the prototypical entactogen, MDMA (
7).
Ketamine’s place within the psychoactive pharmacopeia is perpetually controversial, perhaps because it exposes the fault lines in a premise of modern psychopharmacology, namely, that a drug response, be it a higher heart rate or hallucinations, occurs through the action at individual receptors. Ketamine’s hemodynamic, respiratory, anesthetic, analgesic, psychedelic, and entactogenic effects do not cleanly map onto the multiplicity of ketamine’s molecular targets, including
N-methyl-
d-aspartate (NMDA) receptors, mu and kappa opioid receptors, and hyperpolarization-activated and cyclic nucleotide–gated cation channels, among others (
6).
A comparison between ketamine and classical psychedelics pointedly illustrates this disconnect. In contrast to ketamine, classical psychedelics like LSD (and psilocybin) have a profound psychoactive effect that is completely blocked by a relatively selective antagonist for the 5-HT
2A receptor (
8), which may also account for their therapeutic effects. Although ketamine acts as an anesthetic at high doses, subanesthetic doses (<1 mg/kg i.v.) produce clinical, phenomenological, neurophysiological, and functional effects on consciousness that are shared with classical psychedelics (
Table 1). Ketamine and LSD have shared phenomenology (
9): although it is true that disembodiment is typically more salient during exposure to psychedelic doses of ketamine, dissociation has also been reported with classical psychedelics, whose subjective effects are not identical to each other. Importantly, the term “dissociative” was coined in the 1960s to highlight ketamine’s stark differences from classical anesthetics, which do not lead to dissociation because they induce unconsciousness rather than disconnected consciousness; the dissociative aspects of the ketamine experience share more in common with psychedelics than anesthetics. Moving from the phenomenological to the large-scale brain networks from which experience likely emerges, ketamine shows many similarities to classical psychedelics. Ketamine enhances neurophysiological signal diversity, as measured by the Lempel-Ziv algorithm (
10,
11), leads to a similar reorganization of functional brain networks (i.e., decreased within-network connectivity and enhanced between-network connectivity) (
12), and expands brain state repertoire (
13).
Considering the evidence of shared traits of phenomenology, enhanced neurophysiologic complexity, expanded brain state repertoire, neuroplasticity, and antidepressant effects, it is remarkable that ketamine is not considered a psychedelic drug. By contrast, other drugs with a much wider divergence of pharmacological properties—antihypertensives, for example—are still considered to be part of the same class because of their common physiologic or therapeutic effects. That the molecular targets for the phenomenological and therapeutic effects of psychedelics, and especially entactogens, have yet to be fully clarified is another reason why drug classification should not be based exclusively on the receptor level. Rather than an exclusive perspective, it is our view that a comprehensive approach that is inclusive of multiple relevant parameters describing the activity and effects of promising psychiatric drugs like ketamine, MDMA, and psilocybin will be more informative and yield useful flexibility as the field evolves. It is certainly possible that additional discoveries will further highlight a significant role for molecular targets outside of monoamine transporters, NMDA, and 5-HT2A receptors in the subjective and therapeutic effects of entactogens, dissociatives, and classical psychedelics, respectively.
The thought-provoking work reported by Hess and colleagues highlights the necessity for a more flexible, multidimensional framework that might better accommodate further mechanistic discoveries. On the similarly thorny problem of classifying psychiatric disease itself, exciting progress is in motion using empirically defined symptom clusters and imaging-based biotypes (e.g.,
14). A similar dimensional analysis for psychoactive drug effects could yield surprising similarities, like the one reported by Hess et al. Mining these similarities for convergence at the level of network physiology, for example, rather than pharmacology, could provide us with promising targets for brain stimulation, or more useful animal models that do not rely on difficult-to-interpret behavioral responses. The recent enthusiasm for incorporating powerfully psychoactive substances into the treatment of psychiatric disorders is likely to yield dozens of novel drugs that appear to act across a spectrum of illnesses—we now have the tools to reorient drug development away from receptor specificity and toward the broader scale of neurobiological effects.