Understanding the neurobiological underpinnings of schizophrenia remains a daunting challenge—what is happening in our highest-order cortical circuits to lead to such distortions in abstract thinking? Symptoms of thought disorder are highly correlated with reduced functioning of the dorsolateral prefrontal cortex (DLPFC), a recently evolved brain region that subserves working memory, abstract reasoning, and executive functions and that exists only in primates (
1). A major clue has been known for almost three decades: patients with schizophrenia have reduced numbers of spines and dendrites on the pyramidal cells in deep layer III of the DLPFC (
2–
4). Deep layer III expands greatly in primate evolution and contains the recurrent excitatory microcircuits that interconnect on dendritic spines to generate the mental representations that are foundational to working memory and abstract thought (
1). These dendritic alterations in schizophrenia are highly specific to region, cell type, and lamina, as they are not seen in DLPFC layers V or VI, or even in superficial layer III, and they are not seen in the primary visual cortex (
2–
4). The neuropathological data are consonant with the more gross-level in vivo brain imaging of individuals at risk for schizophrenia, which shows a wave of gray matter loss during adolescence in subjects at risk as symptoms emerge (
5) and a loss of synapses early in the course of disease (
6). Altogether, these data have suggested excessive, erroneous pruning of neuronal connections, with early and pronounced loss in the DLPFC but progressing to envelop multiple association cortices (
5). What are these cells that lose so many spines and connections?
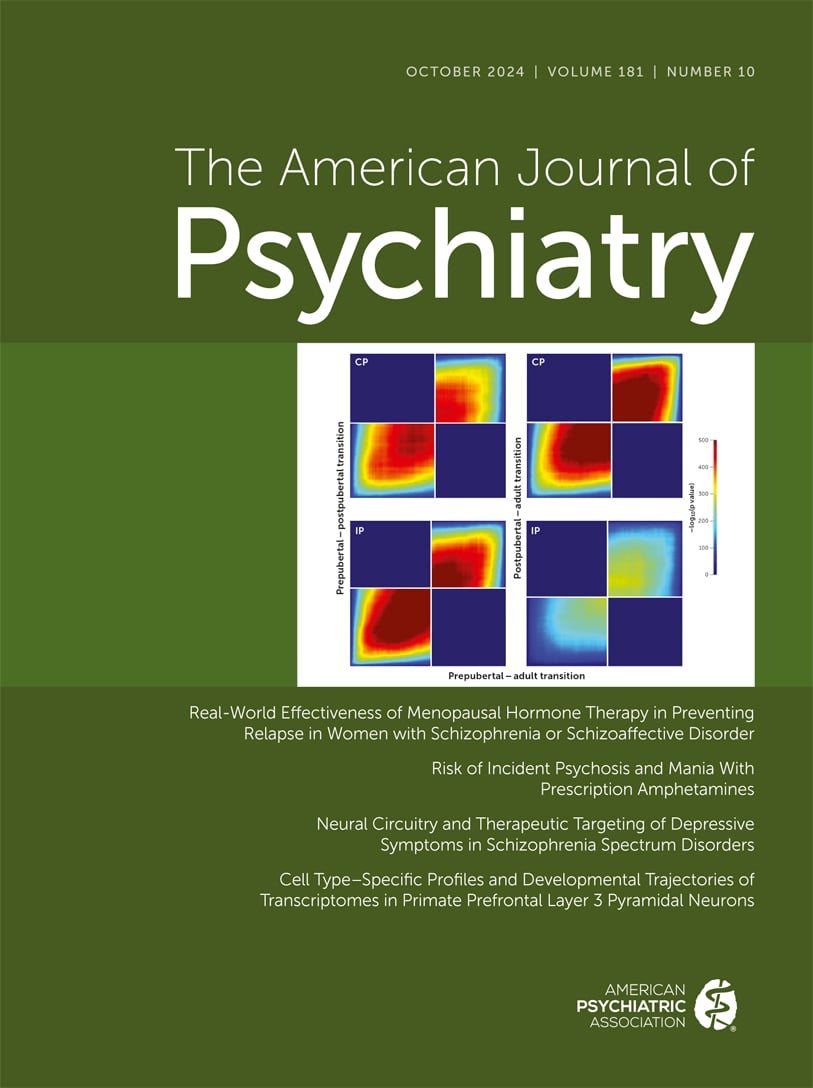
What is different about the CP cells compared to the IP cells transcriptionally? Arion et al. found that the CP cells could be characterized by a number of differences from the IP cells; for example, they had low levels of
SCN1B, which encodes a subunit of a voltage-gated sodium channel, whereas the IP cells had high levels of
SCN1B. Most intriguingly, Arion et al. show that the CP cells express much higher levels of
ADCYAP1, which encodes the “master stress peptide,” pituitary adenylate cyclase-activating polypeptide (PACAP). PACAP is highly expressed in circuits that orchestrate the stress response, and it has a critical role in initiating stress actions (
8). As described below, chronic stress causes loss of spine and dendrites from prefrontal cortex (PFC) pyramidal cells (
9), and thus an enriched “stress transcriptome” would be of particular interest when trying to understand why a specific layer of pyramidal cells is so vulnerable to spine loss in schizophrenia. Furthermore, PACAP and its receptors have genetic links to schizophrenia (
10). Thus, it is especially interesting that CP pyramidal cells have uniquely high levels of this transcript in the primate DLPFC.
Stress, Schizophrenia, and the DLPFC
Stress exposure has long been known to be an aggravating factor in the descent into illness, including the alterations that underlie thought disorder in schizophrenia (
1). In rodents, chronic stress causes loss of dendrites and spines from pyramidal cells in the medial PFC and is correlated with impaired cognition, and in humans is associated with reduced PFC gray matter (
9). In patients, the wave of gray matter loss at the onset of schizophrenia is related to stress and inflammation (
5), suggesting that these factors play a role in the structural changes that drive pathology. Thus, understanding how stress impairs PFC function and leads to dendritic spine loss may provide important clues about the etiology of the illness.
We have shown that uncontrollable stress rapidly impairs DLPFC function, switching control of behavior to more primitive circuits—for example, the amygdala—via high levels of dopamine and norepinephrine release in the DLPFC (
1). High levels of dopamine and norepinephrine stimulate dopamine D
1 receptors (D1R), β1-adrenoceptors (β1-AR), and alpha-1 adrenergic receptors (α1-AR) on layer III dendritic spines that drive feedforward cAMP-calcium signaling, which in turn opens nearby potassium channels to rapidly weaken synaptic efficacy and reduce PFC neuronal firing (
1). For example, recent research shows that high levels of norepinephrine activate β1-AR on dendritic spines, which drives PKA opening of nearby Cav
1.2 L-type calcium channels, which in turn opens SK potassium channels to reduce firing and impair working memory (
11). This process may be dysregulated by inflammation, prolonging detrimental actions (
1).
In parallel studies, transcriptomic analyses of bulk-tissue macaque and human DLPFC found that superficial (
CUX2-expressing) pyramidal cells express high levels of calcium-related signaling molecules that are also linked to genetic risk for schizophrenia and other mental illnesses (
11). These pyramidal cells have high levels of
CALB1, encoding the calcium binding protein, calbindin, indicative of high calcium usage; high levels of
GRIN2B encoding the NMDAR-GluN2B subunits that flux high levels of calcium and are essential to DLPFC neurotransmission; and high levels of
CACNA1C, encoding the L-type voltage-gated calcium channel Cav
1.2 (
11). Genetic alterations in
CACNA1C are a common risk factor for mental illness, including gain-of-function mutations related to schizophrenia (
12). Interestingly, these same superficial pyramidal cells also have exceptionally high expression of
CHP1, which encodes an endogenous inhibitor of the phosphatase calcineurin, and calcineurin inhibitors can induce psychosis (
13). However, it is not known which of these superficial pyramidal cells is the subgroup identified by Arion et al. as the CP cells that are malleable in adolescence. Although Arion et al. performed laser capture microdissection of layer III pyramidal cells of young animals (3.2–4.7 years), and our study employed more general single-nucleus RNA sequencing of older animals (6.6–8.2 years), might we try to bridge across studies by identifying a subgroup of macaque DLPFC
CUX2 (superficial layer) pyramidal cells with exceptionally high
ADCYAP1 (PACAP), and very low
SCN1B?
“Molecular Fingerprint” of CP and CUX2B Pyramidal Cells
Our analyses identified three subgroups of CUX2 (superficial layer) pyramidal cells: CUX2A, CUX2B, and CUX2C (
11). Of these, subgroup CUX2B expresses the highest
ADCYAP1 (PACAP) and the lowest
SCN1B, suggesting that at least some of the CUX2B subgroup may be some of the CP cells that project across the corpus callosum (
Table 1). While a rigorous bridge across studies would require quantitative comparisons of a very large number of genes, a focus on a few transcripts related to DLPFC neurotransmission and stress indicates interesting characteristics of the CUX2B cells. Thus, in addition to their very high expression of
ADCYAP1, they also have the highest levels of
CALB1, indicative of high calcium use, and
GRIN2B, which encodes NMDAR-GluN2B, needed for neurotransmission. This elevated level of calcium may be needed to sustain recurrent excitatory firing across the hemispheres. Perhaps most relevant to neuronal vulnerability, CUX2B pyramidal cells express the highest levels of
KCNN3, which encode the SK3 potassium channels that weaken connectivity and
reduce neuronal firing with high levels of calcium (
Table 1).
The CUX2B subgroup also has higher levels of stress-related signaling molecules (
Table 1), including
ADRB1, which encodes the β1-adrenoceptor (β1-AR) that drives cAMP-PKA and Cav
1.2 signaling to reduce firing during stress (
11);
ADCY1, which encodes adenyl cyclase 1 (AC1), the major synthetic enzyme for cAMP;
PRKACB, which encodes a PKA catalytic subunit; and much higher levels of
AKAP5, which anchors PKA, β-AR, and Cav
1.2 together in the plasma membrane to drive calcium currents (
14). Conversely, CUX2B pyramidal cells have lower levels of the phosphodiesterases that catabolize cAMP (
Table 1; lower
PDE4A,
PDE4B, and
DISC1, which anchors PDE4s to the calcium-storing smooth endoplasmic reticulum). An earlier study by Arion et al. (
15), of just the 3-year-old animals, found similar results, with CP cells enriched in cAMP-calcium signaling, including the PKA subunit
PRKACB, and the PKA anchoring protein AKAP5, suggesting that at least a substantial subset of CUX2B cells are the CP neurons. Interestingly, the CUX2B cell group also expresses the highest levels of
DRD1, which encodes the dopamine D
1 receptor known to mediate the stress response (
16). It is noteworthy that the dopamine innervation of macaque DLPFC layer III is increased in adolescence (
17), which may increase the stress response in these D1R-enriched pyramidal cells. Patients in the early stages of schizophrenia have increased expression of D1R in the DLPFC (
18), suggesting that an even larger stress response may occur in patients at this early stage.
The very high expression of potassium channels in layer III spines, and especially the very high expression of SK3 channels in the CUX2B (putative CP) pyramidal cells, may be a fundamental factor in why these cells may “overprune” dendritic spines. While very high levels of cAMP-calcium signaling can strengthen connections in many neurons—for example, in the hippocampus—the very high expression of KCNN3 (SK potassium channels) in the CUX2B subgroup switches cAMP-calcium signals from strengthening to weakening connectivity, which may drive spine loss when sustained for long periods of time.
Arion et al. speculate that PACAP may be involved in driving spine loss, as it can increase RAC1 and TIAM1 signaling to alter the actin skeleton and cause spine collapse, signaling pathways that are altered in layer III DLPFC pyramidal cells in patients with schizophrenia (
19). The CUX2B cells have higher levels of
TIAM1 and
RAC1 compared to other CUX2 (superficial) pyramidal cells (
Table 1), consistent with this hypothesis. Rac1 alteration of the actin cytoskeleton depends on activating PKC
α (
20), and in rodents PKC inhibition prevents stress-induced spine loss in medial PFC and working memory impairment (
21). In this regard, it is noteworthy that all atypical antipsychotic and antimanic medications inhibit PKC (
22), for example, by blocking 5-HT
2A and α1-A receptors, or through more direct effects on IP3R-related calcium signaling. Thus, these agents may have some of their therapeutic actions by protecting PFC dendritic spines from toxic stress signaling.
These new data from macaque DLPFC suggest that the CP pyramidal cells, which develop later than their neighbors, may have a “stress-enriched” molecular fingerprint that makes them most vulnerable to atrophy, including the higher expression of
ADCYAP1 (PACAP). It is noteworthy that PACAP acts at three receptors that increase cAMP signaling: PAC1 (
ADCYAP1R1), VPAC1 (
VIPR1), and VPAC2 (
VIPR2) receptors. VPAC2 is of special interest, as duplication of its gene,
VIPR2, is a rare risk factor of very large effect for schizophrenia (
23), suggesting that elevated stress signaling in DLPFC may be particularly impactful for mental disorders.
Transcriptomic signatures provide a bridge across studies and species, where additional tract tracing experiments in macaque begin to illuminate the molecular and connectional properties of the cells most vulnerable in schizophrenia, and how they may vary across developmental stages and may be differentially affected by stress, inflammation, and genetic alterations over the lifespan. The discovery by Arion et al. that CP cells are the latest to mature, during a developmental period when schizophrenia onset is most common, suggests that these cells may be a particular target of pathology, with a molecular fingerprint that renders them especially vulnerable to stress.