Case Vignette
Danielle Rawlings is a 25-year old female who was referred to you by her primary care physician for help with addressing issues of depressed mood, after being unable to tolerate treatment with two trials of antidepressant medication
She reported to you that she has been having trouble with her mood for much of the past year. “It started with feeling soooo negative and pessimistic. I couldn’t enjoy anything––not my job, not spending time with my friends, not sex with my boyfriend–– nothing.” She described that, in addition to pessimism and anhedonia, she also had been finding it difficult to get going in the morning and that she often slept 10 hours yet still felt exhausted. “My roommates learned to not even look at me until I’d had my first cup of coffee.”
Danielle described that she had gone to see her primary care physician about 10 months ago to try an antidepressant. “When I was in college, I had a bout of depression after my loser ex-boyfriend cheated on me and we broke up. I tried therapy with one of the intern psychologists at the Student Health Center. It didn’t help much, but probably because she spent a lot of time talking about herself and her problems. Their doc saw me for, like, 10 minutes and gave me a prescription for some generic Prozac. I tried it for a week, but I got all anxious and nervous and nauseated and gave up. I started doing some yoga, and that helped me pull out of it.”
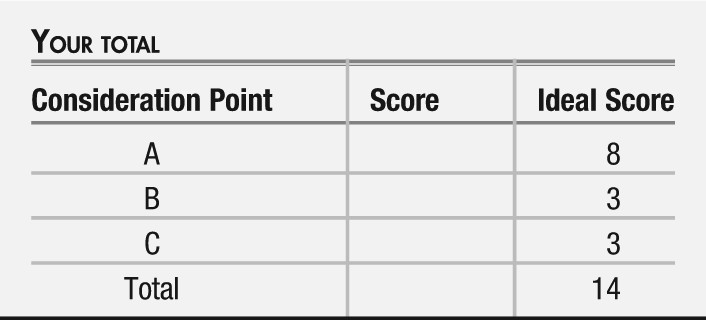
Consideration Point A
At this point in the patient’s history, your differential diagnosis includes
| A.1_____ | Unipolar, major depressive disorder |
| A.2_____ | Hypersomnia not elsewhere classified |
| A.3_____ | Bipolar II depression |
| A.4_____ | Substance-induced disorder |
| A.5_____ | Obstructive sleep apnea |
Vignette Continues
You probed for more details of her current episode, and in addition to depressed mood, anhedonia, hypersomnia, and fatigue, she endorsed feeling hungry “all the time... craving comfort food,” with a 10 pound weight gain over the past year. She also felt worthless and guilty about being unable to “snap out of it.” She denied thoughts of suicide.
As you inquired more about her history, she denied any prior periods with obsessive thoughts or compulsive behaviors, hallucinatory experiences, or delusional thoughts. However, she endorsed that 2 years ago she had one occasion when she slept only 2 hours a night for 4 days while working on a big project for a course in her major, noting “I was ‘in the zone,’ with my creativity flowing and plenty of energy.” At that time, she was told by classmates “girl, you are on fire with creative ideas” and once the project was turned in, she impulsively dragged her boyfriend at the time to go on a trip to the mountains “for a weekend of pleasure to make up for my week of hell.” She reported that her thoughts came easily at that time, but were not “racing.” She had a similar bout about 14 months ago that lasted for 4 days in the wake of flying home from a trip to Hawaii, where she had been a bridesmaid. Both episodes had resolved spontaneously. She estimated that the second episode occurred about 2 weeks before her current depressed period began.
As you inquired about her early life history, you learned she had a fairly unremarkable childhood as the eldest of three sisters who grew up in an intact family of origin. Her dad was “a novelist who sometimes drank a little too much, but he was happy when he overdid it;” she denied that he ever was verbally or physically violent or sexually inappropriate with the patient or her siblings. She was a good student in high school and graduated from college with a BA degree in art and architecture. Currently, she worked doing graphic artwork for a web design company. She lived in a townhouse with two female roommates who had been good friends in college.
The patient reported never smoking tobacco or consuming alcohol to excess, but occasionally using marijuana while in college. She reported “I don’t smoke any weed now because it makes my mood worse. Plus, I don’t need the munchies.” She denies the use of other drugs of abuse, and notes that she will have a glass of wine with friends on the weekends but not during the week.
In reviewing her medical history, the patient denied having major medical conditions. When you evaluated her, she reported taking no routine prescription medications other than oral contraceptive pills.
You already had her complete a self-rated 30-item Inventory of Depressive Symptomatology (
1) before coming to see you, and she had scored 31, comparable to a score of 17 on the 17-item Hamilton Depression Rating Scale (
2), indicative of moderate symptom severity (
3).
On examination, she was slender, pleasant, and cooperative with the interview, casually attired in shades of gray and black, with a nose ring and hair dyed jet-black with a few strands of pink. Moderate psychomotor slowing was noted. Eye contact was good. Speech was of slightly slowed rate and monotonous prosody, but of normal volume. Affect was fatigued. Mood was endorsed as “sometimes it all just seems so bleak.” Thought process was generally linear and coherent but slightly sluggish. Thought content was without hallucinations, delusions, or current suicidal or homicidal intent. Cognitively she was awake, alert, and oriented to self, place, date, and circumstances. Memory registration was intact with 3/3 stimuli, and recall after delay was 3/3 items. She recalled the prior five United States presidents without difficulty. Her similarities were abstract (apple/orange = “delicious fruit”; watch/ruler = “for measuring things”). Her insight was good in that she recognized she needed to receive professional help. Judgment currently was good in that she was open to considering all options for treatment. Neurologically, her gait stride length, arm swing, turning, and rapidly alternating movements were all normal. You detected no focal neurological deficits.
Consideration Point B
At this point, your differential diagnosis includes
| B.1_____ | Unipolar, major depressive disorder |
| B.2_____ | Hypersomnia not elsewhere classified |
| B.3_____ | Bipolar II depression |
| B.4_____ | Substance-induced disorder |
| B.5_____ | Obstructive sleep apnea |
Vignette Concludes
After a discussion of the options for treatment, the patient accepted quetiapine monotherapy, titrating up to 300 mg/d over 4 weeks. You asked her to leave you a voicemail message after 1 week, in order to let you know how things were going, either good or bad; she did so, and reported that she felt a little more tired the first 2 days than before starting the medication, but that had corrected. After 4 weeks of this regimen, she returned for a follow-up visit and reported that she was feeling markedly better—less pessimistic, more energetic, and “more like my well self.” After 6 weeks, she emailed you that she felt “really positive and solid, not moody or flighty at all.” At a follow-up visit after 8 weeks of quetiapine monotherapy, she reported that she was “pretty much a 10 out of 10” in terms of her recovery. Her self-rated IDS-30 score was 4, which is in the remission range.