Case Vignette
Megan Washington is a 22-year-old female who was referred to you by her primary care physician for help with treating depressed mood and behavioral impulsivity that have exceeded his capacity to help.
“I need help with my depressions,” the patient said as she first met you. She reported to you that she had been having trouble with her mood ever since she was a sophomore in high school. “Growing up was tough. My parents split up when I was in seventh grade. My dad’s new girlfriend was a total bitch to me, and my stepdad was not much better. I got back at my dad’s girlfriend by trashing her precious rose garden, and at my stepdad by leaving his tools outdoors to rust! I got into Aleister Crowley, Robert Anton Wilson, and a lot of other esoteric stuff as an escape. My grades were not bad, even though I cut class a lot, smoked weed a lot, and drank a bit too much ... mostly swiping it from my mom’s stash. I was just trying to numb the awfulness of it all ... trying to make some sense of all the pain. I tried Vitamin K once, at a concert, but ended up with a bad k-hole experience, and never went back there again.” She clarified that there were relatively few days that she did not smoke at least a joint of marijuana from age 15 to age 20, that she used ketamine once (with an adverse reaction), and never used other substances of abuse. She reported that, at present, she smokes perhaps one or two joints in a week, and will drink only on the weekends (typically two to four drinks on Friday and on Saturday) with friends.
“All the adults in my life then were so controlling—‘don’t wear that outfit,’ ‘don’t hang out with him,’ ‘you’re staying out too late’—and were so lame, as if I’d ever want to grow up and be like them, those losers. My problems were really all their fault.” She described angry arguments with her parents and their new partners, and how she would break their rules for when to be home or for finishing her schoolwork. She managed to graduate from high school and has been a student at a community college while also working part-time as a barista at a coffee place near campus.
She endorsed that she now felt sad more days than not, that very little made her mood brighten, and that she had low energy despite tending to sleep more than 10 hours a day.
Consideration Point A
At this point in the patient’s history, your differential diagnosis includes
A.1——Unipolar major depressive disorder
A.2——Depression as a part of bipolar disorder
A.3——Attention deficit hyperactivity disorder
A.4——Substance-induced mood disorder
Vignette Continues
You probed for more details of her current episode, and in addition to depressed mood, anhedonia, hypersomnia, and fatigue, she endorsed a 10-pound weight gain over the past year and feeling worthless and guilty about “wasting her life.” She endorsed frequent thoughts of what would happen if she were to end her life—if she were to relieve her suffering by death, is there a heaven? would she reach an enlightened state and transcend the physical plane?—but no plans or attempts to end her life.
As you inquired more about her history, she denied any prior periods with obsessive thoughts or compulsive behaviors. She did endorse that two years ago she had an experience in late springtime when she had just met a man online “and it was heavenly.” She described that she had been feeling “extra sexy” for a few days before she met him online and then decided to meet in person. She described that “I thought he was like my soul mate or something,” and that she was awake for most of the next week, having “wild animal” unprotected sexual intercourse with him “and with another guy we met in a bar.” She said “all the world was alive, vibrating with energy, as if Mother Gaia were having an orgasm, too.” She spent more money than was usual for her, but this did not do lasting damage to her financial health. “After about 10 days, the guy just up and vanished. I came home, and he and his backpack were gone, and I’ve not heard from him since.” She affirmed that she had not used any substances other than marijuana and alcohol during that time, “and only about one or two beers a day. I didn’t want to get stoned then, because I was already high on life.” She reported that her mood plummeted after that for a couple of weeks, but that, with the help of some friends, she was able to get through it and back to her more typical state of mild sadness.
She noted that, in high school, she had had some periods of feeling “speedy, creative, pretty, and kinda on the verge of laughing a lot” but that these had lasted only three or four days at a time, and she has simply dismissed them as being “a few better days against the bleak background of my reality.”
In reviewing her medical history, the patient denied having major medical conditions. When you evaluated her, she reported taking no routine prescription medications other than oral contraceptive pills.
You had already had her complete a self-rated 9-item Patient Health Questionnaire (PHQ-9) (
1) before coming to see you, and she had scored 17, indicative of moderate severity.
On examination, she was pleasant and cooperative with the interview, casually attired in saffron-colored yoga pants and a lime-green tank top, with multiple pierced earrings in each ear. Mild psychomotor slowing was noted. Eye contact was adequate. Speech was of slightly slowed rate, and monotonous prosody, but of normal volume. Affect was fatigued. Mood was endorsed as “today is not as bad as most days, but still pretty bad.” Thought process was generally linear and coherent. Thought content was without hallucinations, delusions, or current suicidal or homicidal intent. Cognitively she was awake, alert, and oriented to self, place, date, and circumstances. Memory registration was intact with 3/3 stimuli, and recall after delay was 2/3 items. She recalled the prior six U.S. Presidents without difficulty. Her similarities were abstract (apple/orange = “fruit;” hammer/screwdriver = “tools for building things”). Insight was good, in that she recognized she could benefit from professional help. Judgment currently was good, in that she was open to considering all options for treatment. Neurologically, her gait, arm swing, turning, stride length, and rapidly alternating movements were all normal. You detected no focal neurological deficits.
Consideration Point B
At this point, your differential diagnosis includes
B.1——Unipolar major depressive disorder
B.2——Depression as a part of bipolar disorder
B.3——Attention deficit hyperactivity disorder
B.4——Substance-induced mood disorder
Vignette Continues
You shared your diagnostic impressions with the patient, and she agreed that “I’ve been moody for a long time, much more than my friends. It’s hard to accept that this is an illness, rather than just a rough patch. But I want to feel better, and what I’m doing now isn’t working for me.”
She told you that she had tried fluoxetine at age 16, but it made her feel agitated so she stopped after a week. Her pediatrician had given her paroxetine, but that, too, had made her feel more uncomfortable than better, and so she had stopped it after a week as well. She talked with a counselor at her high school, and that had helped her curb what she called her “bad-ass behavior” and gave her some support so that suicide did not look as attractive, but that had not returned her to feeling “good.”
She was open to hearing your recommendations for treatment.
Consideration Point C
Given all the details of the case, your next therapeutic step(s) is/are
C.1——Retry fluoxetine monotherapy but at a low dose
C.2——Trial of escitalopram plus bupropion
C.3——Trial of lamotrigine as monotherapy
C.4——Electroconvulsive therapy
Vignette Concludes
After discussion of the options for treatment, the patient accepted lamotrigine and began a gradual titration schedule, starting at 25 mg a day of Iamotrigine XR and titrating to reach a target of 200 mg per day at week seven. She reported as early as week three that she felt a bit “brighter,” and more “at peace with my inner demons.” You saw her in the office at week four, confirmed that she was having no rashes or other side effects, and continued her titration on schedule.
At a follow-up visit after eight weeks of lamotrigine monotherapy, she reported that she was feeling “more stable, more real than I have in years.” Her self-rated PHQ-9 score was 2, in the remission range.
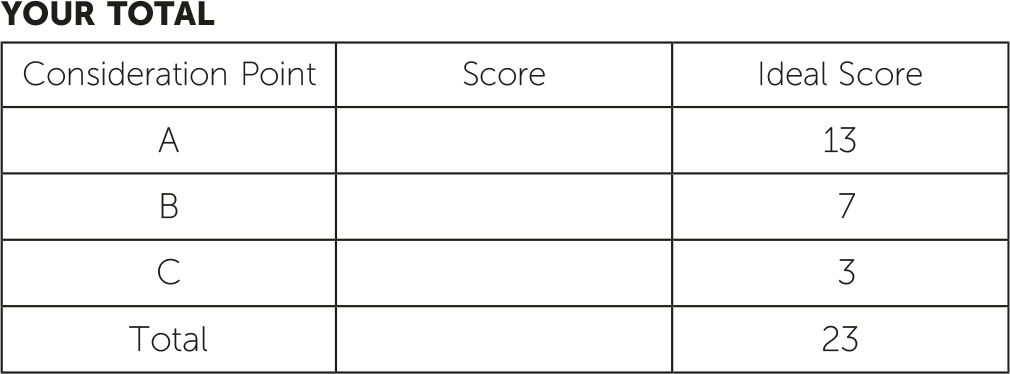
Answers: Scoring, Relative Weights, and Comments
Consideration Point A
A.1——
(+3) Unipolar, major depressive disorder. The patient endorsed several of the DSM-5 criteria for major depressive disorder (
2), and you are struck by her symptom cluster with so-called reverse neurovegetative symptoms.
A.2——
(+3) Depression as part of bipolar disorder. Her depressive episode could be part of unipolar or bipolar mood disorder (
2).
A.3——
(+1) Attention deficit hyperactivity disorder. While she may have had some issues as a child with poor grades, and some impulsive behaviors, the bulk of the information is more supportive of other conditions (
2).
A.4——
(+3) Substance-induced mood disorder. She gives a history of marijuana and alcohol use, with at last one use of ketamine, associated with past mood disturbances (
2).
A.5——
(+3) Conduct disorder. The behaviors the patient describes have several historical elements that are consistent with the presence of CD (
2).
Consideration Point B
B.1——
(−2) Unipolar, major depressive disorder. The patient has given you evidence of hypomanic events and one probable manic episode, and treating her as if she had unipolar depression is not consistent with best practices (
3–
5).
B.2——
(+3) Depression as part of bipolar disorder. Her depressive episode is described as the predominant state with occasional hypomanic and manic episodes (
3–
5).
B.3——
(0) Attention deficit hyperactivity disorder. The patient’s history is marked mostly by mood complaints, rather than cognitive challenges, and the use of psychostimulant monotherapy to address attention deficit hyperactivity disorder would not be consistent with best practices for bipolar disorder (
4,
5).
B.4——
(+1) Substance-induced mood disorder. The patient reports that her use of marijuana is at a low level, as is her use of alcohol (
2).
B.5——
(+3) Conduct disorder. The patient’s history contains many elements for this diagnosis—destroying property, stealing, breaking parents’ rules, school truancy—but it is probably best thought of as a comorbidity to the primary diagnosis (
2).
Consideration Point C
C.1—
(−1) Retry fluoxetine monotherapy but at a low dose. According to the STEP-BD study and other research, selective serotonin reuptake inhibitor monotherapy does not appear to be the treatment of choice for bipolar depression (cf. reference
6).
C.2——
(−2) Trial of escitalopram plus bupropion. While this combination may be quite helpful for unipolar depression (
7), it has not been shown to be an evidence-based practice in bipolar depression.
C.3——
(+3) Trial of lamotrigine as monotherapy. This treatment approach is supported by double-blind randomized clinical trial data (cf. reference
8), and the U.S. Food and Drug Administration has allowed an indication for this drug for this condition.
C.4—
(−2) Electroconvulsive therapy. While ECT is an evidence-based practice for the treatment of depression, it is not the usual next step in the treatment algorithm for a patient like this, with bipolar depression that has not been adequately treated with pharmacotherapy (
9).