Body Dysmorphic Disorder: Clinical Aspects and Relationship to Obsessive-Compulsive Disorder
Abstract
| The core features of BDD are distressing or impairing preoccupation with nonexistent or slight defects or flaws in appearance; the preoccupation triggers excessive repetitive behaviors that attempt to check, fix, hide, or obtain reassurance about the perceived bodily deformities (e.g., mirror checking, comparing with others, excessive grooming, reassurance seeking, and skin picking). |
|---|
| BDD is about as common as OCD, with a current prevalence of approximately 2% of the population. |
| BDD affects nearly as many men as women. |
| Many patients with BDD express suicidal ideation, and the rates of suicide attempts and completed suicide appear markedly elevated. |
| Individuals with BDD may be reluctant to spontaneously reveal their appearance concerns to psychiatrists and other mental health clinicians; thus, BDD may be misdiagnosed as major depressive disorder, social anxiety disorder, OCD, agoraphobia, and other disorders. Patients should be specifically asked about BDD symptoms. |
| The recommended first-line medication for BDD is an SRI, even if appearance beliefs are delusional in nature. |
| SRI doses and trial durations are similar to those used for OCD; higher doses and a longer treatment trial than those typically used for depression and most other disorders are recommended. |
| Antipsychotics may be helpful in addition to an SRI but are not recommended as monotherapy for patients with any level of insight (including delusional BDD). |
| Cognitive-behavioral therapy that is specifically tailored to BDD is the psychosocial treatment of choice. Simply treating BDD as if it were OCD is not recommended. Because the treatment can be complex and challenging, use of a BDD-specific treatment manual is recommended. |
Definition and Core Clinical Features of BDD
Diagnostic Criteria for BDD in DSM-5
Criterion A.
Criterion B.
| Behavior | Percentage |
|---|---|
| Comparing disliked body parts with the same areas on others (e.g., in person, online, on television) | 88 |
| Checking disliked body areas in mirrors or other reflecting surfaces | 87 |
| Grooming (e.g., applying makeup; cutting, styling, shaving, or removing head hair, facial hair, or body hair) | 59 |
| Seeking reassurance about the perceived defects or questioning others about how they look (e.g., “Can’t you see this on my face?”) | 54 |
| Touching the disliked areas to check their appearance | 52 |
| Changing clothes (e.g., to camouflage disliked areas or find an outfit that distracts others from the “defects”) | 46 |
| Dieting (e.g., to make a “wide” face narrower) | 39 |
| Skin picking to improve perceived skin flaws | 38 |
| Tanning (e.g., to darken “pale” skin) | 25 |
| Excessive exercising | 21 |
| Excessive weight lifting | 18 |
Criteria C and D.
BDD Specifiers in DSM-5: Muscle Dysmorphia, Insight, and Panic Attacks
Muscle dysmorphia.
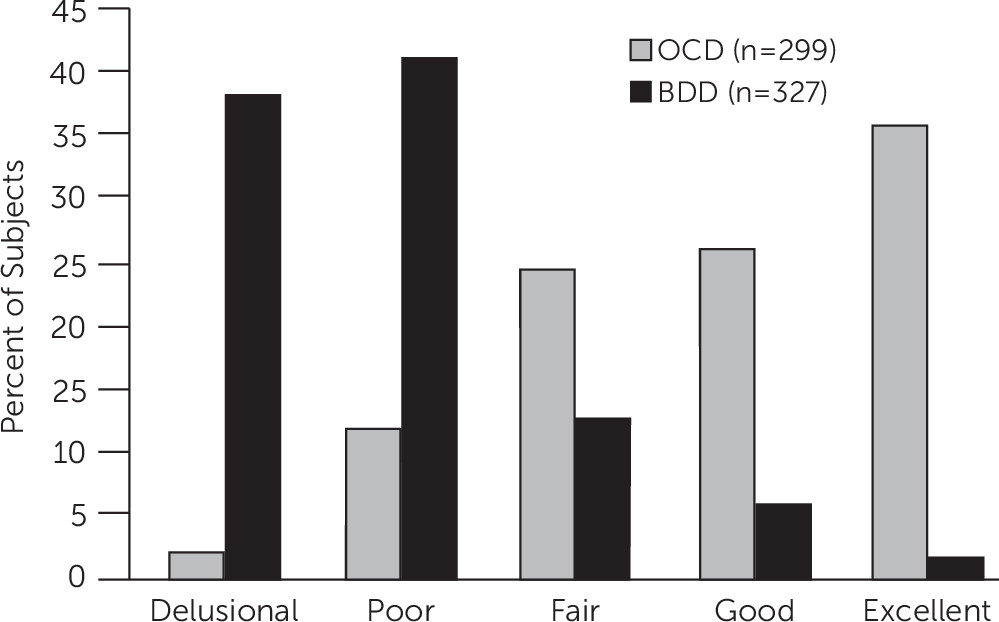
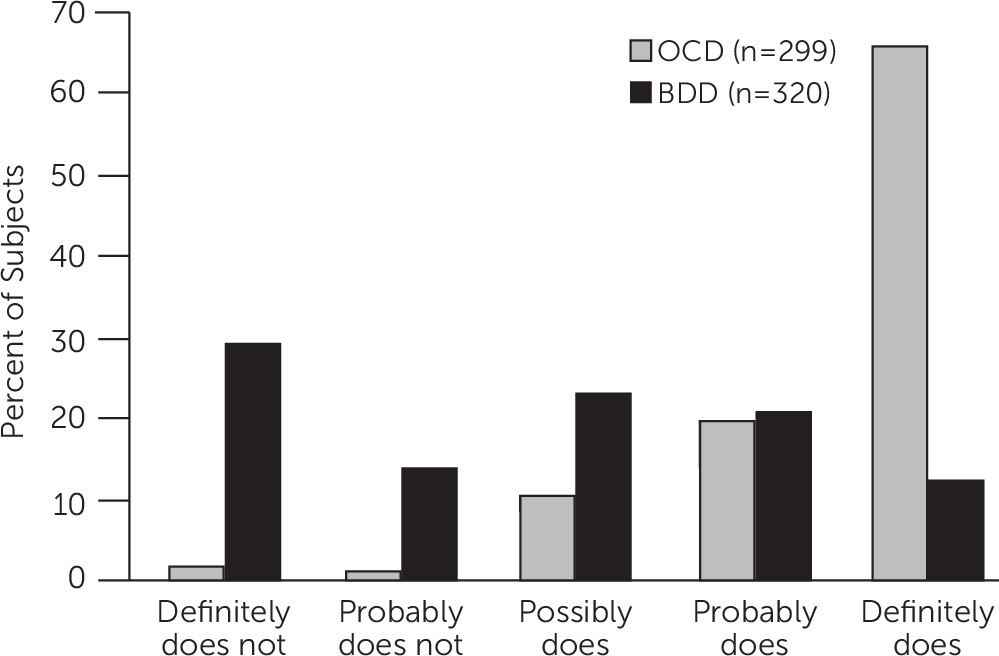
Insight.
Panic attacks.
Key Associated Features
Epidemiology
Age at Onset and Course of Illness
BDD in Youth
Impairment in Psychosocial Functioning
Suicidality
Gender-Related Aspects of BDD
Comorbidity
A Patient With BDD
Emerging Clues About BDD’s Etiology and Pathophysiology
Genetic Factors
Neurobiological Factors
Information Processing Biases
Psychological and Social/Environmental Factors
Evolutionary Perspective
BDD’s Relationship to OCD: Similarities and Differences
| Similarities | Differences |
|---|---|
| Unwanted, distressing obsessions/preoccupations | Different focus of obsessions, core beliefs, and compulsions |
| Distressing repetitive behaviors (compulsions) that aim to reduce anxiety or distress and are functionally linked to obsessions/preoccupations | Poorer insight and more referential thinking in BDD (and more frequent paranoid personality disorder) |
| Similar BDD–YBOCS/Y-BOCS scores for individual items | More frequent comorbid major depressive disorder and comorbid substance use disorders in BDD |
| Most demographic features | More frequent suicidality in BDD |
| Often severe functional impairment and markedly poor quality of life (even poorer in BDD?) | More childhood emotional and sexual abuse in BDD? |
| High levels of perfectionism; high neuroticism, low extraversion | Differences in translational studies (e.g., different structural MRI findings; greater frequency of threatening interpretations of ambiguous social and appearance-related information in BDD) |
| Course of illness (often chronic) | Differences in CBT: In BDD, more complex and often longer treatment, with greater focus on cognitive techniques, and behavioral experiments; inclusion of perceptual retraining, habit reversal for skin picking and hair plucking/pulling, approaches for cosmetic surgery; greater need to address depressive symptoms |
| Familiality | More intensive strategies (e.g., motivational interviewing) needed to engage and retain patients with BDD in treatment |
| Overlapping genetic vulnerability? | |
| Abnormalities in frontostriatal systems, including hyperactivity on fMRI in the orbitofrontal cortex and head of the caudate | |
| Relatively high doses of SRIs as first-line pharmacotherapy |
How to Assess Patients for BDD
| DSM-5 Criterion | Questions |
|---|---|
| A: Preoccupation with perceived defects or flaws in appearance that are not observable or appear only slight to others | “Are you very worried about your appearance in any way?” or “Are you unhappy with how you look?” |
| “Can you tell me about your concern?” or “What don’t you like about how you look?” | |
| “How much time would you estimate that you spend each day thinking about your appearance, if you add up all the time you spend?” or “Do these concerns preoccupy you?” | |
| B: Repetitive behaviors in response to appearance concerns | “Is there anything you feel an urge to do over and over again in response to your appearance concerns?” Give examples of repetitive behaviors |
| C: Clinically significant distress or impairment in functioning | “How much distress do these concerns cause you?” Ask about anxiety, social anxiety, depression, feelings of panic, and suicidal thinking |
| “Do these concerns interfere with your life or cause problems for you in any way?” Ask about effects on work, school, other aspects of role functioning (e.g., caring for children), relationships, intimacy, family and social activities, household tasks, and other types of interference | |
| D: Concerns not better explained by an eating disorder | Ask diagnostic questions for anorexia nervosa, bulimia nervosa, and binge eating disorder |
| Muscle dysmorphia specifier | “Are you preoccupied with the idea that your body build is too small or that you’re not muscular enough?” |
| Insight specifier | Elicit a global belief about all of the perceived defect(s): “What word would you use to describe how bad your (fill in disliked areas) look?” Optional: “Some people use words like unattractive, ugly, deformed, or hideous.” The global belief must be inaccurate. Do not use beliefs that are true, such as “I don't look perfect” or “I want to look better.” |
| “How convinced are you that these body areas look (fill in patient’s global descriptor)?” |
How to Differentiate BDD From Disorders With Which It Is Often Confused
OCD
Excoriation (Skin-Picking) Disorder
Trichotillomania (Hair-Pulling Disorder)
Major Depressive Disorder
Social Anxiety Disorder (Social Phobia)
Agoraphobia
Generalized Anxiety Disorder
Eating Disorders
Psychotic Disorders
Gender Dysphoria
Olfactory reference syndrome
Clearly noticeable physical defects
Treating BDD
Treatment Challenges and How to Address Them
Surgical, Dermatologic, Dental, and Other Cosmetic Treatment
Pharmacotherapy
SRI efficacy.
SRI dosing.
SRI trial duration.
SRI switching and augmentation.
Non-SRI monotherapy.
Cognitive-Behavioral Therapy
Components of CBT for BDD
Foundation for treatment.
Cognitive restructuring.
Relapse prevention.
Combined Pharmacotherapy and CBT
Approaches for Treatment-Refractory BDD
Future Directions
Acknowledgments
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).