Advances in Mobile Mental Health: Opportunities and Implications for the Spectrum of E-Mental Health Services
Abstract
Introduction
| Level | Source/entry | Initiator goals/aims | Pros | Cons/liabilities | Comments/suggestions |
|---|---|---|---|---|---|
| 1 | Website information | Obtain health information and read ‘in-time’ or follow-up on physician’s verbal instructions | Get information, understand how to approach a problem and triage problem | Quality of information varies Inaccurate patient self-diagnosis | Better if referred to a site by clinician who made appropriate diagnosis |
| 2 | Support/chat groups or “communities” | Gain support, answers, tips and perspective | Get a sense as to what are others doing for treatment and to cope; feel part of a group | The patients may or may not be similar; quality of information varies | Support in group format is nice for some |
| 3 | SM | Person/patient/caregiver: additional option for interaction; clinician: skeptical unless known commodity | Feeling understood, heard; more ‘in-time’ | Not HIPAA compliant, no time for this for most clinicians, significant boundary issues ( e.g., self-disclosure, invading patient privacy) | Clinician should ask what platforms patient uses, but not promise to participate or track, triage acute issues to phone or in-person |
| 4 | Self-directed assessment by using screening tools with feedback | Person/patient: good habits, reflection tips; caregiver: reflection tips, tools to assess loved ones; clinician: refer patients to tips on clinical care | Customized to learning preference/style; make progress outside of a clinic; reduced clinician time demand | Not all problems can be self- assessed; some illnesses affect insight; quality of assessment varies | Good for motivated persons and even better if referred by clinician who has checked it out |
| 5 | Formal educational materials | Person/patient: education; caregiver: education, supports, and advice; clinician: CME | In-depth and evidence-based education; document progress in learning | Less interaction with instructors compared to in-person; may not fit all learning styles | Tend to be higher quality, but may cost money to obtain |
| 6 | Self-care decision-making options by one-time assessment by a professional | Person/patient/caregiver: additional options; clinician: skepticism unless known commodity | Customized preference/style; empowered; increased self-efficacy | What if the path of steps is not clear: should I do A or B? | Using members of an interdisciplinary team in a stepped care approach is better; linked to clinician |
| 7 | Email/text | Person/patient: common and fabric of life; apps ‘log’ experience and give data to clinician; clinician: used and incorporated into EHR | Patient gets quick advice, details on routine matters; convenient easier for teen patients: prefer texts to calls? | Occasional use for acute issues; HIPAA compliance issues if not secure; patient may expect future response | Better if email is within EHR; HIPAA compliant; things taken out of context; and miscommunication |
| 8 | Mobile health, psych apps, sensors and other technologies | Access, mobility, and low cost option. apps ‘log’ experience and give data to clinician; clinician: better integrated, longitudinal assessment | Convenient improved cueing of patients (i.e., to appointments); good narrative by ecological collection of data) | HIPAA issues for compliance may be more complex; patient may expect future response; data integration issues are complex | Better if integrated within HER; can systems to monitor respond ‘in time’? Private and public data may not be integrated |
| 9 | Synchronous, traditional or TMH care | Person/patient: it really works and is much more convenient; clinician: if patients like it, it is a good option | There is no shortcut to synchronous decision-making (patient-clinician; primary care-psychiatry) | It always has to be scheduled (and paid for) | A great option; not always needed due to lesser, easier options |
| 10 | De facto hybrid care (synchronous and asynchronous technology) to technology-based integrated care | Person/patient: I connect in-person and via technology; clinician: a team leader in a true system of care | A multi-modal approach for patients, clinicians and programs is a start; progressive healthcare systems are doing this | Linkage with interdisciplinary staff helps discussion, prioritization and planning | Not always available, but eventually folks will shift if healthcare financing shifts; paradigm shift is needed. |
mHealth, mobile MH and MH/psychiatric apps
An Overview of mHealth
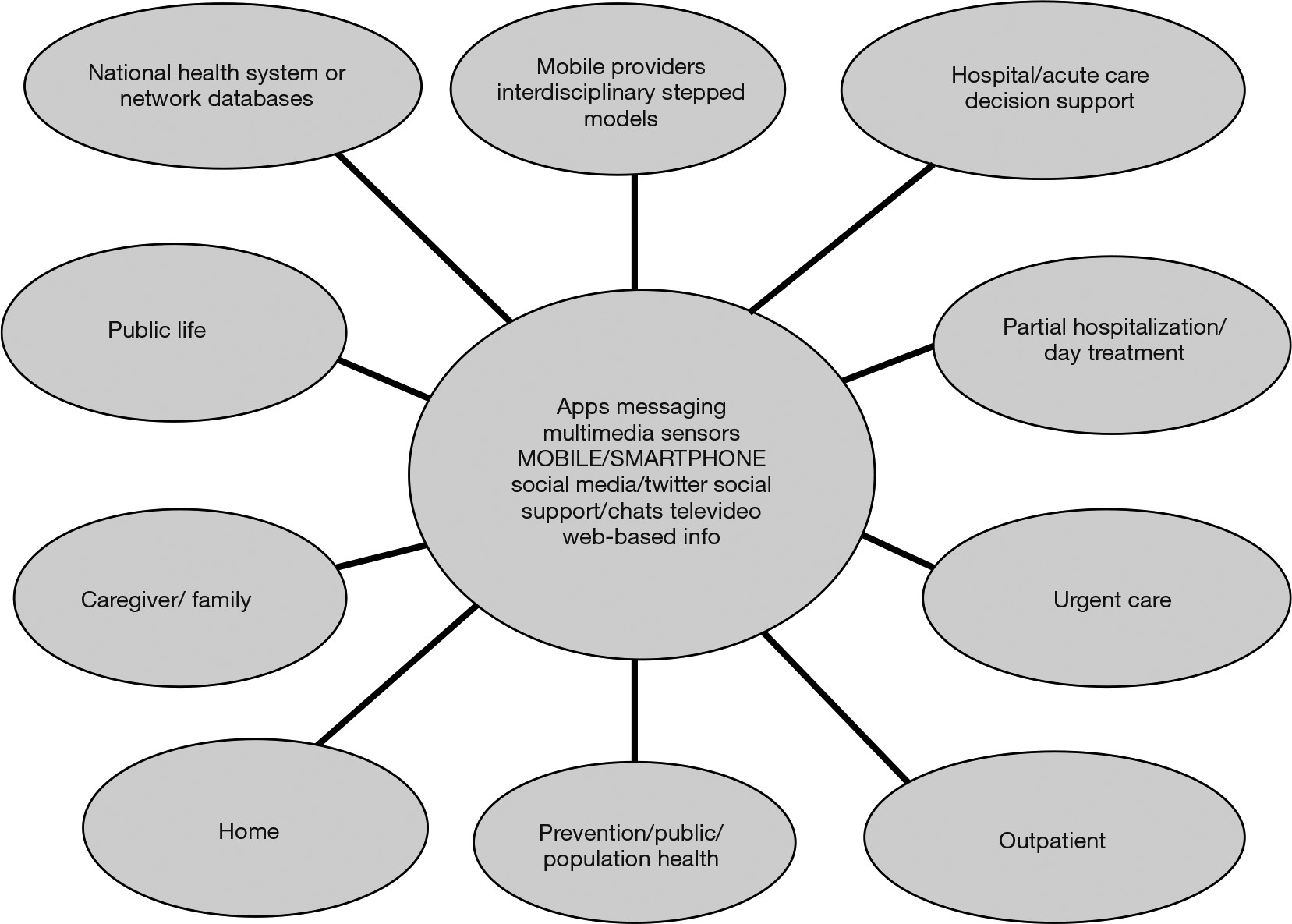
mMH and MH/Psych Apps
Internet and other technology-based options for patients, caregivers and clinicians
Support Groups and Participation in a “Community”
Structured Information and Tools for Self-Directed Habit, Lifestyle or Illness Changes
Informal Advice from Health Professionals Without Guidance
Traditional Clinician-Assisted Decisions, Telepsychiatric Care and Other Evidence-Based Options
Clinical care, training/education, system administration: approaches and preliminary guidelines
Technology Integrated into Clinical Practice
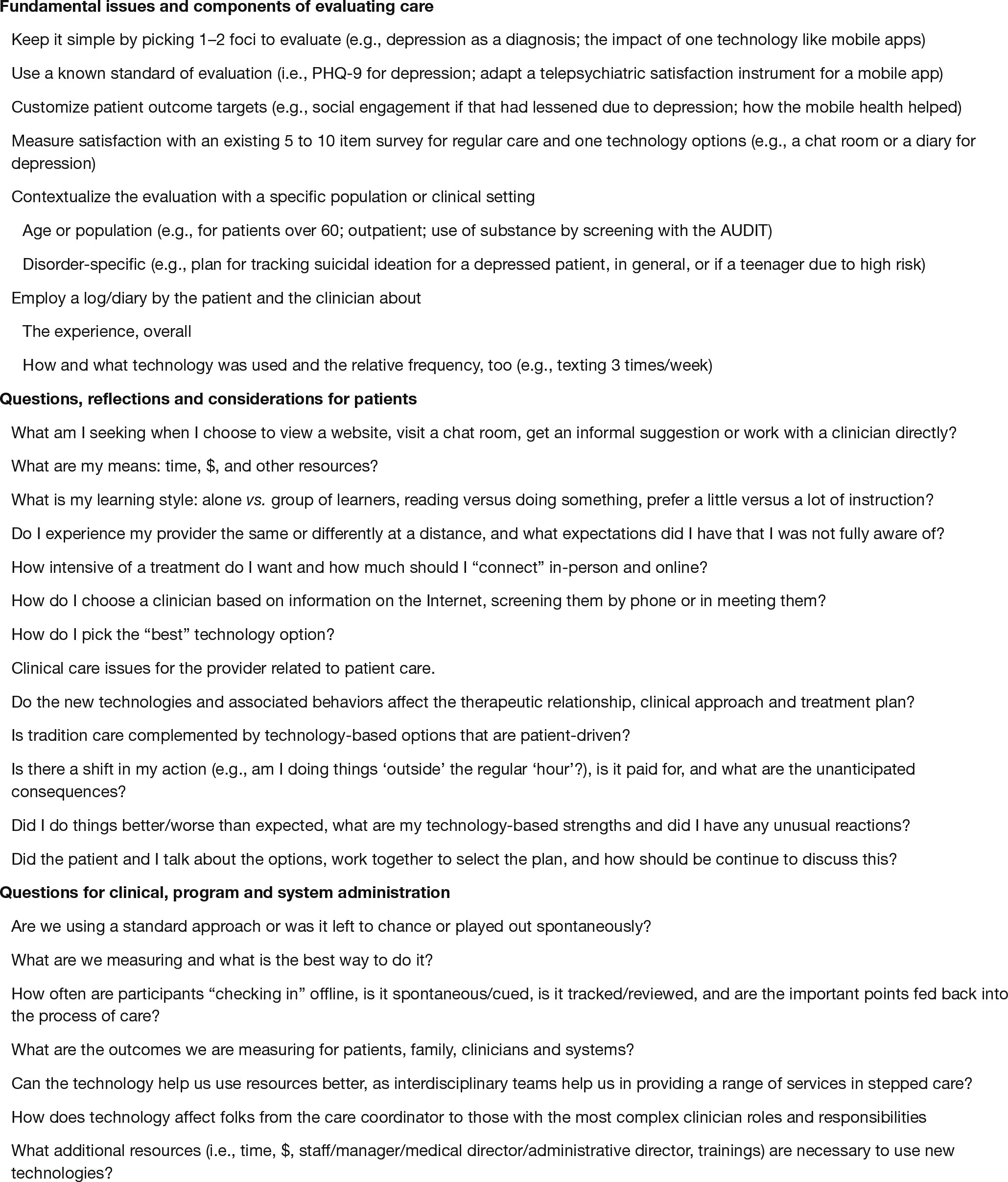
Training and Education
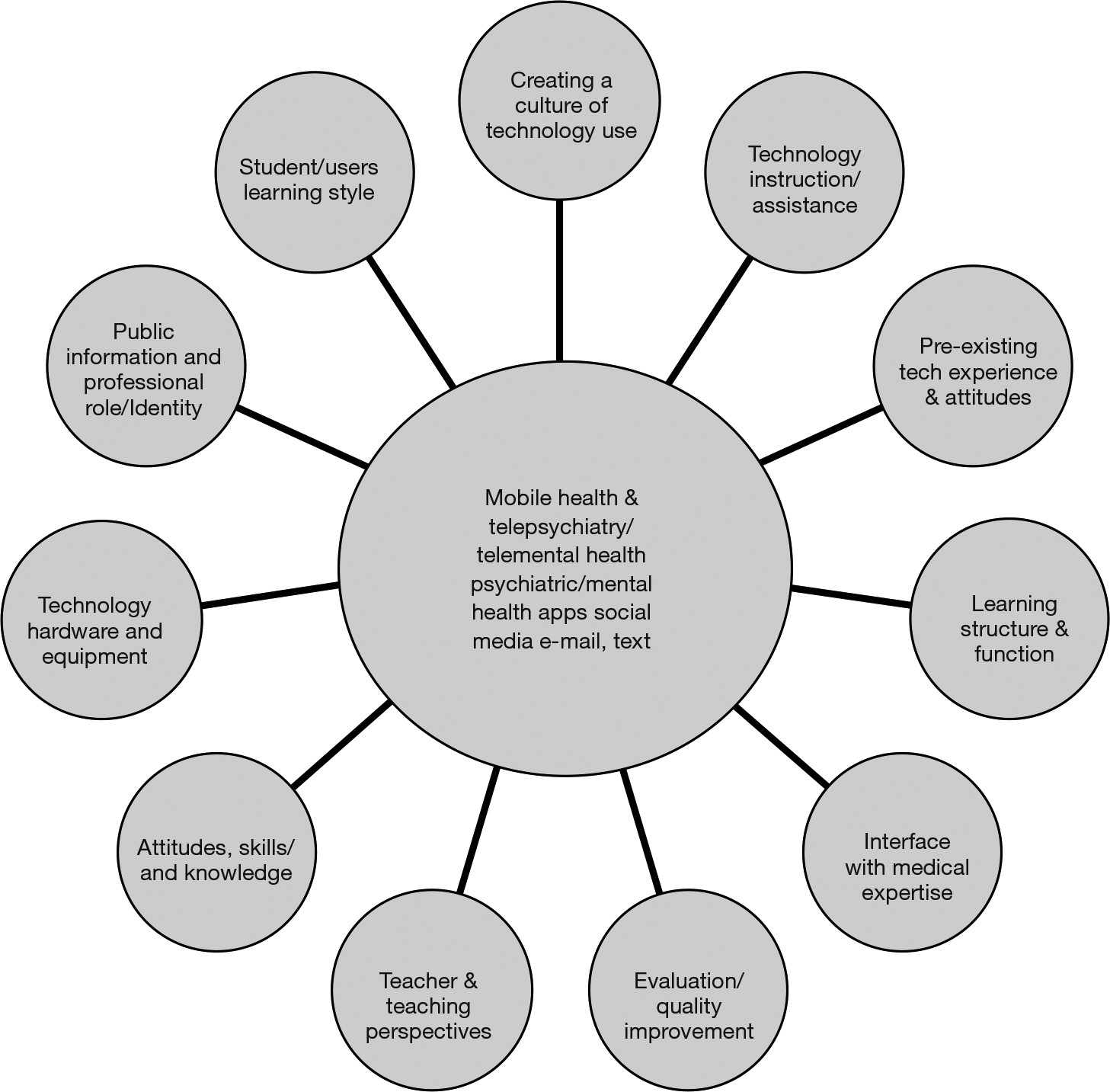
Developing an Administrative Approach
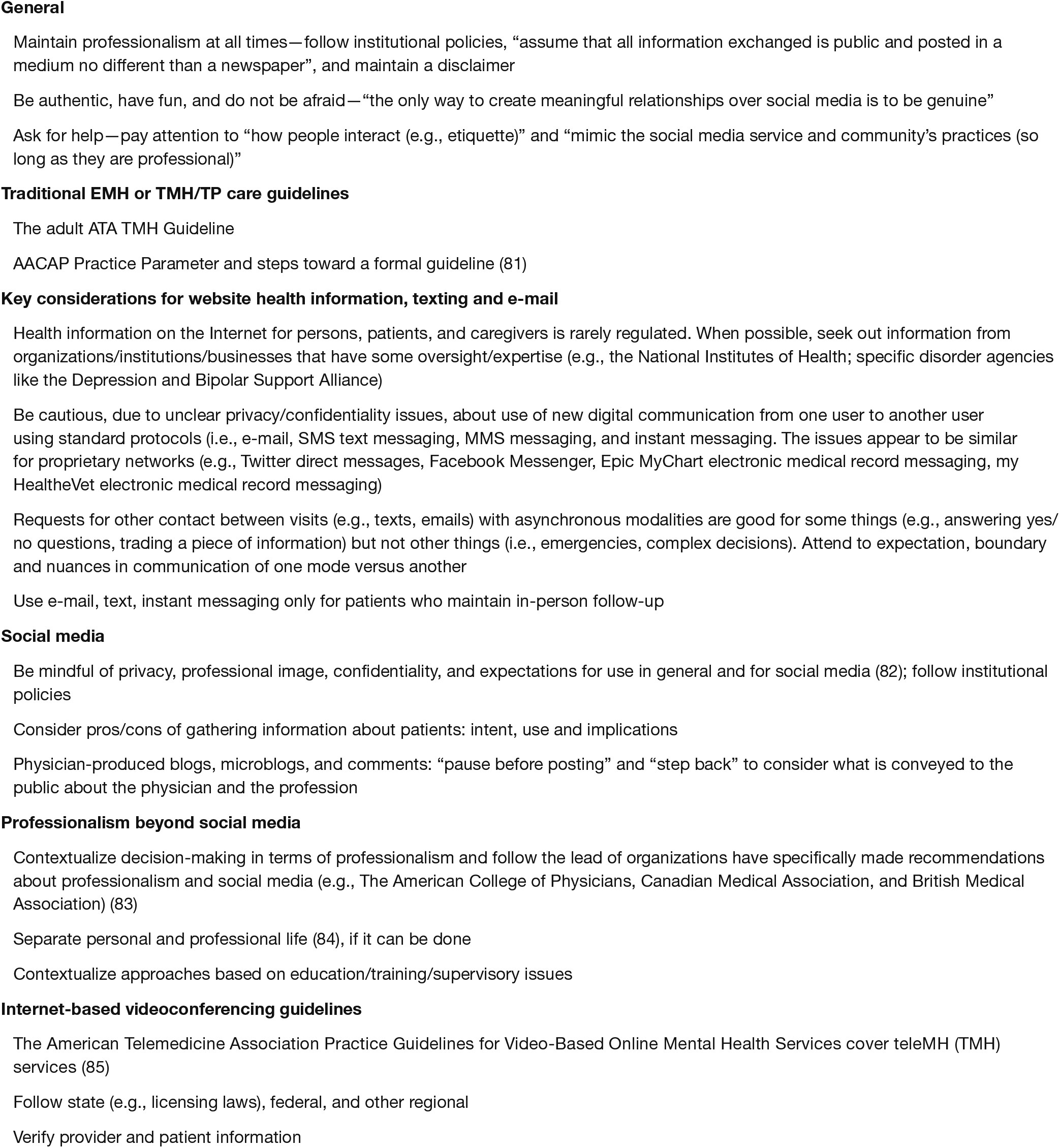
Guidelines
Discussion
Conclusions
REFERENCES
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).