The biopsychosocial model has served as a structure, primarily for clinical formulations of individual patients, for several decades, and evidence and support for this approach have increased over time. During the growing focus and research advances on the biological underpinnings of mental illnesses in recent decades, there has been broad awareness of the simultaneous relevance of biological, psychological, and social factors to the onset and course of mental (and physical) illnesses. However, psychiatry has given less attention to the social factors at the societal, rather than just the individual, level and how those population-level, societal factors play a role in the epidemiology of behavioral health conditions.
To advance the prevention of chronic health conditions, such as hypertension, diabetes, chronic obstructive pulmonary disease, and congestive heart failure, and many other illnesses, the fields of medicine and public health have increasingly homed in on social risk factors and adverse health behaviors at the individual level and the social determinants of health at the societal level. The World Health Organization (
2,
3) defines the social determinants of health as the conditions in which people “are born, grow, live, work, and age” and notes that these determinants are shaped by the multilevel distribution of money, power, and resources. Such conditions include access to and quality of education for children and employment for adults, the distribution of wealth and other forms of opportunity within society, and characteristics of housing and other built structures, to name just a few. Understanding health as influenced by these societal conditions places the responsibility of health and health equity firmly within the realms of politics, policies, and governance and encourages lawmakers to consider the health impacts of all policies (
2).
Despite long-standing recognition by psychiatrists and other mental health professionals of the important effects of individual-level social factors on mental illnesses and substance use disorders, our field has focused less on social factors that are best understood, and addressed, at the societal level. The social determinants of mental health, which are largely the same as the social determinants of chronic physical health conditions, are addressable through policy and programs, environmental change, and both collective and individual decisions within society. In this article, we provide an overview of the social determinants of mental health, discuss why they deserve special emphasis, and provide recommendations for how psychiatrists and other mental health clinicians can incorporate this perspective into their work both within and outside of clinical settings.
Conceptualizing the Social Determinants of Mental Health
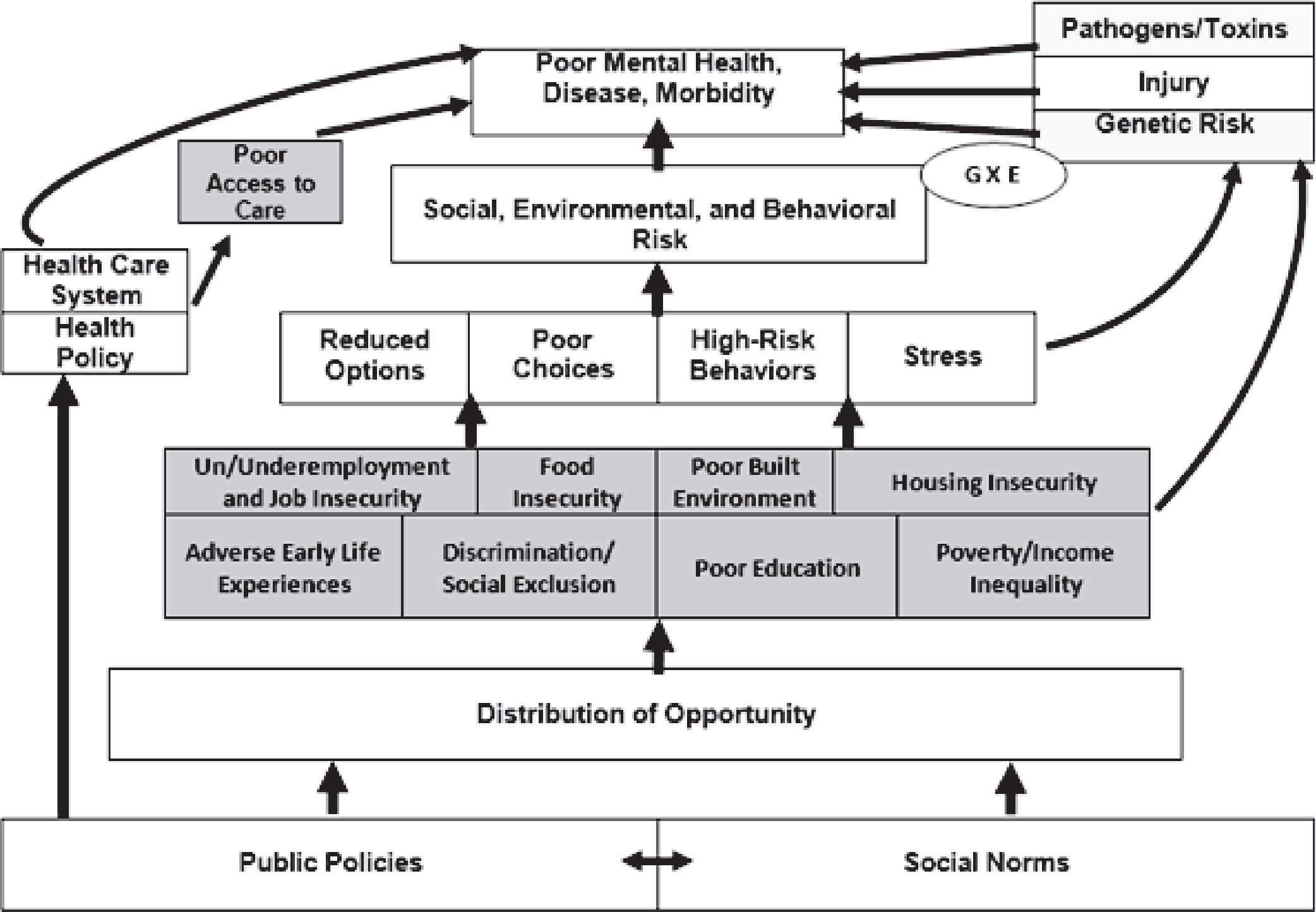
Our conceptualization of the social determinants of mental health—presented in greater detail elsewhere (
4)—is shown in
Figure 1, which attempts to dissect the driving forces behind social, environmental, and behavioral risk factors for poor physical and mental health, as well as disease and morbidity. It should be noted that our model is focused on conditions in the United States, although the social determinants of health clearly have ubiquitous (although varying) effects across countries. It could be argued that our model pertains to an individualistic, urban, Western view of the world. Furthermore, we intentionally focus on socioenvironmental determinants primarily at the level of society, rather than the family. We nonetheless acknowledge that even in the Western world (and perhaps especially in the so-called “collectivist” countries of Asia), beneficial or adverse features stemming from within the family also play a central role in mental health and risk for mental illnesses. As such, some of the factors considered and interventions suggested in this article are specific to the United States. The effects and interventions to address the social determinants could be very different in other cultural or ethnic settings and between urban and rural settings within the same country.
With those disclaimers about our conceptualization aside, the nine social factors and societal conditions in the shaded portion of
Figure 1 are what we deem to be some of the main “core” social determinants of mental health (racial discrimination and social exclusion; adverse early life experiences; poor education; unemployment, underemployment, and job insecurity; poverty, income inequality, and neighborhood deprivation; poor access to sufficient healthy food; poor housing quality and housing instability; adverse features of the built environment; and poor access to health care). These nine core social determinants shown in
Figure 1 serve as a starting point, partly because they have been recognized in relation to diverse chronic physical health conditions. Yet there are other social determinants of mental health that could be articulated, including inadequate or unequal access to transportation (
5); exposure to violence, conflict, and war in childhood or adulthood (
6); mass incarceration and poor relations between law enforcement and communities (
7); environmental air, water, or land pollution (
8); climate change (
9); sexism and other forms of non–race-based discrimination; and adverse or unsupportive features of the workplace.
In this architecture of risk, the social determinants of health predispose individuals and populations to poor physical and mental health, increased risk for many physical and mental illnesses, and poorer course/outcomes of such illnesses when they occur. As shown in
Figure 1, at the individual level, being affected by one or more social determinants can lead to poor choices and adverse health behaviors (in large part owing to reduced options), which in turn leads to known risk factors (e.g., poor diet, substance misuse) for poor physical and mental health and ultimately to increased morbidity and earlier mortality. In addition to poor choices and adverse health behaviors, exposure to adverse social conditions undoubtedly leads to stress and known psychological and physiological stress responses concerning allostatic load (
10), hypothalamic-pituitary-adrenal axis activation (
11), and inflammation (
12), all of which increase the risk for a number of mental illnesses. This aspect of our model (proximal risk factors) is congruent with the widely adopted biopsychosocial model for understanding circumstances and disorders of individual patients.
Our conceptualization also suggests that illness etiologies that are thought of as “biological” determinants can be prominently influenced by social and environmental factors. For example, exposure to toxins and pathogens and the likelihood of injury are often related to adverse community and societal factors. Furthermore, genetic determinants can be prominently influenced by social and environmental factors through at least two mechanisms—gene-by-environment interactions (
13) and epigenetic modifications (
14). Ongoing research into these genetic mechanisms will further highlight the importance of understanding the diverse ways in which the social determinants of mental health affect risk, including genetic risk.
In addition to understanding some of the ways in which the social determinants of mental health lead to poor mental health, increased risk for mental illnesses and substance use disorders, and poorer course and outcomes of behavioral health conditions when they are present, clinicians and citizens at large should also be interested in the deeper factors that set the stage for the diverse social determinants to exist within society. That is, although the biopsychosocial model shapes our understanding of individual patients, a model of social determinants of health also informs our understanding of risk and resilience—and gives directions for intervention—at the community and population level. As we conceptualize these deeper layers, the core social determinants of mental health can be understood as stemming directly from unequal distribution of opportunity. Although it may affect individual patients and may be considered in formulations and intervention planning based on the biopsychosocial model, this unequal distribution of opportunity is primarily a concern about society. As such, it is a social justice issue, rather than a clinical issue. Social justice means fair distribution of advantages and equal sharing of burdens while focusing on those most disadvantaged (
15).
In our model, the unequal distribution of opportunity—an inequity in resources, money, power, voice, and choices at the level of the structure of society (which then leads to effects at the level of the individual)—is driven both by public policies and social norms, which are two types of ubiquitous, pervasive, and persistent (and perhaps even difficult to recognize as pertinent to health) social contextual factors. Although income inequality is perhaps the best studied form of inequality (
16), the unequal distribution of opportunity is also apparent in terms of education, political power, and other aspects of civic life. We view the social determinants of health as coming about largely through inequalities (unequal distribution of opportunity). For example, food insecurity in the United States is not grounded in a shortage of food; rather, food insecurity is attributable to unequal distribution of and access to adequate, healthy food (
17).
Public policies are codes, rules, and legislation pertaining to education, employment, wages, food, housing, neighborhoods, and many other facets of society (
4). Examples of public policies that have diverse downstream effects on physical and mental health include the tuition costs for higher education within a state’s college system, federal minimum wage legislation, and city and county zoning ordinances. These public policies usually do not appear at first glance to be health policies, but they drive the social determinants of mental health, which in turn drive risk and ultimately mental health outcomes. Social norms, on the other hand, pertain to values, attitudes, impressions, and biases held by individuals in society and by the collective. Rather than being codified or officiated like public policies, social norms are largely learned and promulgated within groups. Instead of regulations, they are opinions and beliefs, including political ideologies as well as views on class, race/ethnicity, and gender, to name just a few. Together, public policies and social norms—which mutually reinforce and strengthen one another—are the driving forces behind unequal distribution of opportunity and, in turn, many of the social determinants of mental health.
Both public policies and social norms are structured such that they favor some individuals and groups over others, which sets the stage for the unequal distribution of opportunity noted above and thus the social determinants of mental health. Although clinical interventions clearly have a role in reducing risk for mental illnesses, the greatest population-based impact for preventing many chronic physical health conditions and a number of mental illnesses and substance use disorders would be achieved by optimizing public policies to make them more health promoting and by shifting social norms so that together we prioritize the health of all members of society.
In addition to the often “covert” role of public policies in influencing health, actual health policies are obviously also important to consider. Health policies shape the structure and function of the health care system, which clearly has an impact on individual and population health (
4). Poor access to health care (which we conceptualize as one of the core social determinants of mental health) has an important role in shaping health and disease.
Our conceptualization suggests that risk for poor mental health and mental illnesses can be most broadly and effectively minimized by working at the deepest levels. As we conceptualize nongenetic (socioenvironmental) causation, public policies and social norms drive unequal distribution of opportunity (inequality), which drives the diverse social determinants of mental health, which in turn create stress and constrict options, which leads to poor choices and risky behaviors (
4). Although we must intervene at all levels, the deeper we go, the greater the overall impact for the population.
Thus, the social determinants of health are upstream, fundamental causes of disease and disparities/inequities in disease (
18) that would continue to exist even if more proximal risk factors and causes of disease were addressed (
19). If risk factors such as an unhealthy diet and unsafe living conditions are considered the precursors of disease, then the environmental and contextual factors that precede or shape these risk factors (e.g., food insecurity or inadequate enforcement of housing regulations) can be considered the causes of the causes. These social determinants can be understood through the lens of social justice, and they can be mitigated through advocacy, political will, and policy interventions (
20,
21).
Two Examples of the Social Determinants of Mental Health
To illustrate the clinical and policy relevance of the social determinants of mental health, we provide two examples—income inequality and poor education.
With regard to income inequality, a robust body of research supports the association between income inequality and poor physical health outcomes. As reported in a meta-analysis of studies with multilevel data across countries, there is an association between income inequality and premature mortality, even after analyses control for socioeconomic status, age, and sex (
22). Similarly, there is a correlation between income distribution of countries and the average life expectancy of their citizens (
23). In the United States, research has uncovered an association between state-level income inequality and mortality rates (
24). Infant mortality rates are also linked to higher levels of income inequality, particularly in metropolitan areas of the United States (
25).
Income inequality is also a social determinant of mental health in terms of (a) leading to poorer mental health, (b) increasing risk for and incidence of mental illnesses and substance use disorders, and (c) worsening course/outcomes among people affected by mental illnesses or substance use disorders. For example, county-level analyses have shown an association between income inequality and depression prevalence in older adults (
26). Using the Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System, one study found a positive correlation between state income inequality and depression prevalence (
27). Income inequality is also associated with substance use disorders and substance-related outcomes; for example, a New York City–based study showed that the risk of death from a drug overdose was significantly higher in neighborhoods with greater income inequality (
28). Other work has shown an association between income inequality and schizophrenia in the most economically deprived wards in South London (
29).
In addition to associations with specific mental illnesses, income inequality is also associated with poor overall mental well-being. A recent ecological study observed an association between income inequality and more mentally unhealthy days, even after controlling for poverty and per capita income (
30). Income inequality is also associated with a lower index of child well-being scores (
31). In addition, some researchers have found poorer mental health among lower-income women in highly unequal societies (
32).
Addressing the effect of income inequality on mental health requires individual-level interventions, some of which can be delivered in the clinical setting, as well as societal-level interventions centering on policy. At the clinical level, providers should consider assessing income status in all patients, and providers should research the level of income inequality in the counties and states in which they practice. Providers can work to improve linkages for individuals in poverty to appropriate social services, and they can work with patients to address other social determinants of mental health that contribute to poverty and income inequality, including unemployment, low education, and discrimination.
Clinical-level interventions, although important and relevant to patients at an individual level, will not lead to lasting changes in the population and will not effectively address the impact of income inequality on mental health and substance use disorders. To effectively begin to take action on income inequality as a social determinant of mental health, as well as a social justice issue, interventions need to be carried out upstream, at the policy level. Federal programs that focus on reducing the poverty level in the United States, including Medicare, Medicaid, Social Security, and the Earned Income and Child and Dependent Care tax credits, ultimately lead to less income inequality in society (
33). Unfortunately, much recent political debate and action has been focused on cutting these federal programs rather than expanding them. To truly address the increase in risk for mental illnesses and substance use disorders associated with high levels of income inequality, providers must advocate for programs and policies that reduce poverty and support greater economic equality in our society.
Like income inequality, poor education is also associated with poorer physical and mental health outcomes. Higher-quality education, and greater educational attainment, have been repeatedly and consistently associated with better social outcomes (e.g., lower likelihood of criminal justice involvement, better social networks). Poor education is linked to adverse health behaviors (e.g., smoking, unhealthy diet, sedentary lifestyle or limited physical activity, and substance misuse) that set the stage for greater risk (e.g., higher body mass index) for chronic physical illnesses (e.g., diabetes, cardiovascular disease) (
34). Thus, inadequate educational attainment, and especially school dropout, should be considered a public health problem (
35). Furthermore, greater educational attainment is predictive of lower death rates and later death.
Using data from diverse prior studies, Galea et al. (
36) estimated the numbers of deaths in the United States that were attributable to six social factors. In 2000, approximately 245,000 deaths were attributable to low education (defined as less than a high school education, relative to a high school diploma equivalent or greater). Furthermore, Galea et al. (
36) estimated that 176,000 deaths were attributable to racial segregation, 162,000 to low social support, 133,000 to poverty, 119,000 to income inequality, and 39,000 to area-level poverty. Such mortality estimates are comparable to those from the leading disease-related causes (e.g., the number of deaths attributable to low education was comparable to the number due to acute myocardial infarction). Although obtaining a high school education is strongly tied to lifelong health, college completion is associated with higher social and economic achievement and increased quality-adjusted life expectancy (
37). The bidirectional effect of mental health and educational attainment should also be recognized; mental health is predictive of college success, and identifying and addressing the mental health needs of college students is therefore crucial (
38,
39).
As in our example of income inequality, poor education is also a social determinant of mental health in terms of leading to poorer mental health, increasing risk for mental illnesses and substance use disorders, and worsening course/outcomes of individuals affected by such disorders (
40). Addressing the adverse impact of poor education on mental health, and its influence on risk for and poorer course/outcomes of mental illnesses and substance use disorders, requires individual-level interventions that can be partly delivered in the clinical setting, as well as societal-level interventions centering on policy.
In the clinical setting, pediatricians and other primary care physicians obviously have a role in screening for educational barriers or problems, but psychiatrists and other mental health professionals also have a role. Clinicians can assess educational attainment, educational quality, and other aspects of education (e.g., history of bullying, disciplinary actions, extracurricular involvement) of all patients. Among those still getting their education (especially children and adolescents), this will be an ongoing process, and any opportunities for improvements should be identified. Youths whose educational success appears to be impaired by attention problems or learning difficulties should be referred for evaluation by a neuropsychologist, who can conduct testing and use results to obtain suitable accommodations and supports when necessary to assist these students in excelling and completing school. As another example, among mental health professionals working with persons with serious mental illnesses, supported education can be implemented. Supported education has been shown to improve the likelihood of graduation, assist in the development of interpersonal and work-related skills, and lead to a higher likelihood of employment (
41,
42).
Beyond the clinical setting, improving educational outcomes is obviously best accomplished in the educational sector, as well as other sectors, because parental income, housing quality, neighborhood environment, and other factors undoubtedly influence students’ likelihood of excelling. Some programs have been extensively studied. For example, children who receive high-quality early childhood education are known to experience mental health benefits beyond the commonly emphasized educational benefits. The High/Scope Perry Preschool model is one of the best studied, with positive findings in domains that affect mental health, such as earnings and criminal justice involvement, as distantly as age 40 years (
43). Other programs, such as the federally supported Head Start program, provide educational services, as well as social, health, and nutritional services for children from socially disadvantaged settings.
In addition to the level of education attained, quality of education is also crucial and is underpinned by many factors, including training, pay, and support of teachers; adequacy of academic resources; student-to-teacher ratios; the quality of arts, sports, and social programs in schools; and characteristics of the neighborhood in which the school is located. Poor educational quality and persisting educational inequalities are social justice issues, and policies that improve educational quality (and educational equality) will have beneficial effects on lifelong health. There are many ongoing policy decisions at the federal, state, and local levels that affect diverse aspects of educational access, attainment, quality, and equality. Mental health professionals can have a voice in policy decisions and in doing so can emphasize the major impact of education on social outcomes and both physical and mental health.
The Role of Psychiatrists and Other Mental Health Professionals
To promote mental health at the population level and to reduce the risk of mental illnesses and substance use disorders, psychiatrists and other mental health professionals have a role in altering clinical interventions, implementing and evaluating programs, and advocating for policy change. Although we encourage psychiatrists and other mental health professionals to be more active in advocating for the changes in social norms and public policies that are needed to address the unequal distribution of opportunity (i.e., decrease inequality) associated with negative mental health outcomes, this advocacy obviously also extends to general physicians and other health professionals who want to improve the general medical health of their patients and their communities. This work will require new forms of training quite different from those of the medical model, and it will necessitate working in partnership with diverse disciplines. Expanding the concept of mental illnesses from the individual level to public health as a whole is central to the social determinants of mental health framework (
4). This is exemplified by the Health in All Policies framework and Health Impact Assessments and Mental Health Impact Assessments as part of policy or program planning (
44–
47).The public health approach, oriented largely around social justice, requires collaborating with civil rights advocates, early childhood educators, education and employment experts, urban planners, and many other professions in the public health arena and in the realm of policy and politics. In addition to having more public health–informed mental health professionals, we also need more mental health–informed public health professionals advocating for the needed changes in social norms and public policies that are equally important for both mental health and general health.
The social determinants of mental health represent modifiable factors that, if addressed, could lead to improvements in the mental health of our society and could even contribute to the prevention of mental illnesses and substance use disorders. Although these social determinants are categorized into discrete determinants for the purposes of our discussion, they interact with each other in complex ways and exert their effects variably across the lifespan. It is not accidental that these determinants work in concert to drive poor mental health and disparities; rather, it is the unfortunate result of decisions stemming from public policies and social norms that disadvantage some over others. Therefore, given the complexity of the social determinants of mental health, addressing them involves cultivating political will and changing policy.
There is a multitude of reasons why our field must work to address the social determinants of mental health. First and foremost, as indicated previously, it is a matter of social justice. Second, and related closely to social justice, is the fact that the social determinants are largely responsible for race-based and other forms of class-based health disparities and inequities; thus, addressing them will contribute to eliminating health inequities. Third, the social determinants of mental health provide clues about means of prevention at the population level, which is obviously important given the limited effectiveness of existing treatments for many mental illnesses and substance use disorders.
Like income inequality and poor education, the effects of many other social determinants of mental health can be altered through both individual-level interventions and programs and through policy change. Psychiatrists and other mental health professionals have roles in public and policy discourse on discrimination and social exclusion; adverse early life experiences; unemployment, underemployment, and job insecurity; poor access to sufficient healthy food; poor housing quality and housing instability; adverse features of the built environment; and poor access to health care. Social activism has traditionally been fairly common among psychiatrists, although we wonder whether our field’s social activism has diminished compared with that of the 1960s, 1970s, and 1980s, when the community mental health movement and the biopsychosocial model peaked in popularity and was an integral part of psychiatric training. If this trend indeed exists, it would be informative to gain an understanding of the reasons for it and the feasibility or means of reversing it. Psychiatrists have a responsibility to expand their focus to advocate for policies that address the social determinants of mental health. Through these “nonclinical” roles, mental health will be promoted, and the risk for mental illnesses and substance use disorders will be reduced.