It makes sense to want to feel good about oneself. Decades of research suggest that high self-esteem—one’s evaluation of how good, competent, attractive, influential, and socially regarded one is (
1–
4)—portends positive mental health outcomes (
5–
7). However, it is possible to have too much of a good thing. A grandiose sense of self-importance, entitlement, and need for admiration can produce considerable intrapersonal and interpersonal difficulties, culminating into a diagnosis of narcissistic personality disorder (NPD) (
8,
9), an impairing condition that affects 1%–6% of the U.S. population (
10,
11). What distinguishes healthy self-esteem from narcissistic grandiosity? We begin by summarizing research on this question, arriving at the notion that self-esteem regulation is a transdiagnostic psychological process that becomes dysregulated in NPD. We then articulate a cognitive-behavioral formulation of narcissistic self-esteem dysregulation, showing how this dysregulation can be seen as interactions between beliefs, thoughts, feelings, and behaviors. This broadly applicable perspective offers hope for NPD treatment, as it renders self-esteem dysregulation amenable to intervention through cognitive-behavioral therapy (CBT), which has been found effective for several other psychiatric disorders. We then illustrate how key CBT techniques could be applied before concluding with a discussion of the implications of the model and future directions of research.
Narcissism and Its Treatment
Over decades of scholarship spanning psychoanalytic traditions, personality psychology, and clinical science, researchers have sought to characterize the psychological processes that drive pathological narcissism. Although numerous theoretical frameworks have been developed and continue to evolve, they share an understanding that maladaptive patterns of self-esteem regulation are central to pathological narcissism (
12). Data show that, unlike normative, healthy self-esteem, which is associated with positive outcomes (
5–
7), narcissistic self-esteem is fragile, because it is highly contingent on achievement-related successes and feedback from the social environment (
13–
15).
Narcissistic self-esteem is thus conceptualized as precariously elevated. When an individual with NPD is faced with an ego threat (e.g., real or imagined criticism, failure, or reduced social regard), unrealistically high self-expectations crumple into perceived inferiority (
16,
17). Individuals with NPD are, therefore, hypersensitive to ego threats, and when threatened, they respond with efforts to reduce concomitant distress and upregulate self-esteem (
17–
19). These regulation strategies include some of NPD’s most recognizable and maladaptive behaviors. Classic “grandiose” responses include being aggressive or devaluing toward others (
20,
21), fixating on grandiose fantasies (
22), or engaging in self-serving bias (
23). Classic “vulnerable” responses include alienating and isolating themselves (
24) by avoiding situations that may threaten self-esteem (
25), relentlessly criticizing themselves (
26–
28), or engaging in suicidal behaviors and fantasies (
29,
30). This vacillation between overly inflated and deflated self-appraisals, alongside efforts to regulate this unstable sense of self through grandiosity, flawlessness, and/or avoidance, are described in both early psychoanalytic theories of narcissism (
31), the contemporary Alternative DSM-5 Model for Personality Disorders (
8), and the personality disorder section of the
ICD-11 (
32–
34).
It is important to note that research is continually adding nuance to scientific perspectives on self-esteem in NPD (
35). Various frameworks differently emphasize shifts between distinct states of grandiosity (i.e., elevated self-esteem, arrogance, and entitlement) and vulnerability (i.e., shame, insecurity, and neuroticism). Scholars are working to clarify whether and how grandiosity may function to conceal ever-present vulnerability and whether fragile self-esteem is a driving force or an outcome of this process (
17,
18,
26,
36). Recent proposals also offer a more complex and dynamic view beyond shifting grandiosity and vulnerability (
35). In the midst of the field coming to a consensus regarding how to best conceptualize “narcissism,” we offer a cognitive-behavioral model proposing that symptoms of NPD are driven by narcissistic self-esteem dysregulation, which is characterized by fragile self-esteem (maintained by unrealistic beliefs about one’s importance, abilities, influence, or social regard) and habitual maladaptive behavioral strategies that prop up elevated self-esteem.
Despite the high prevalence of harmful outcomes of NPD, few psychotherapeutic treatments for NPD exist, and none have been empirically tested (
12,
37). Existing treatments for narcissistic processes are largely psychoanalytic (
38,
39). More recently, evidence-based psychotherapies for borderline personality disorder, a related but distinct diagnosis from NPD, have steadily been adapted for NPD. Transference-focused psychotherapy (
40), mentalization-based treatment (
41), good psychiatric management (
42), and dialectical behavior therapy (
43) have all adjusted protocols originally for borderline personality disorder to more directly address the unique aspects of NPD. However, none of these adapted therapies have been systematically tested, and developing accessible and pragmatic NPD treatments is critical (
44,
45). Given its effective application to a wide range of disorders, CBT stands as a clear choice for guiding the development of novel NPD interventions.
The CBT Model
CBT is a family of short-term, structured, and problem-focused psychotherapeutic treatments that primarily utilize cognitive (thought- and meaning-related) and behavioral (response- and action-related) interventions aimed at improving psychological functioning (
46,
47). The central theoretical model underlying CBT posits that thoughts, behaviors, and emotions dynamically influence and maintain one another. These processes ideally serve adaptive functions, such as helping individuals accomplish their goals, navigate their environment, and ultimately survive (
48). However, sometimes these cognitive-behavioral systems become dysregulated and produce symptoms of psychopathology. As we illustrate later, this is particularly the case when individuals believe that they cannot cope with situations that are actually tolerable and when they maintain these beliefs by habitually avoiding or escaping unwanted emotions aroused by situations that trigger these emotions (
49). CBT models have been tailored to treat specific disorders, such as major depressive disorder (
50,
51), posttraumatic stress disorder (PTSD) (
52,
53), and borderline personality disorder (
54). Transdiagnostic approaches such as the Unified Protocol (
49) and the Modular Approach to Treating Children (or MATCH) (
55), have also been developed to treat multiple disorders simultaneously or serially.
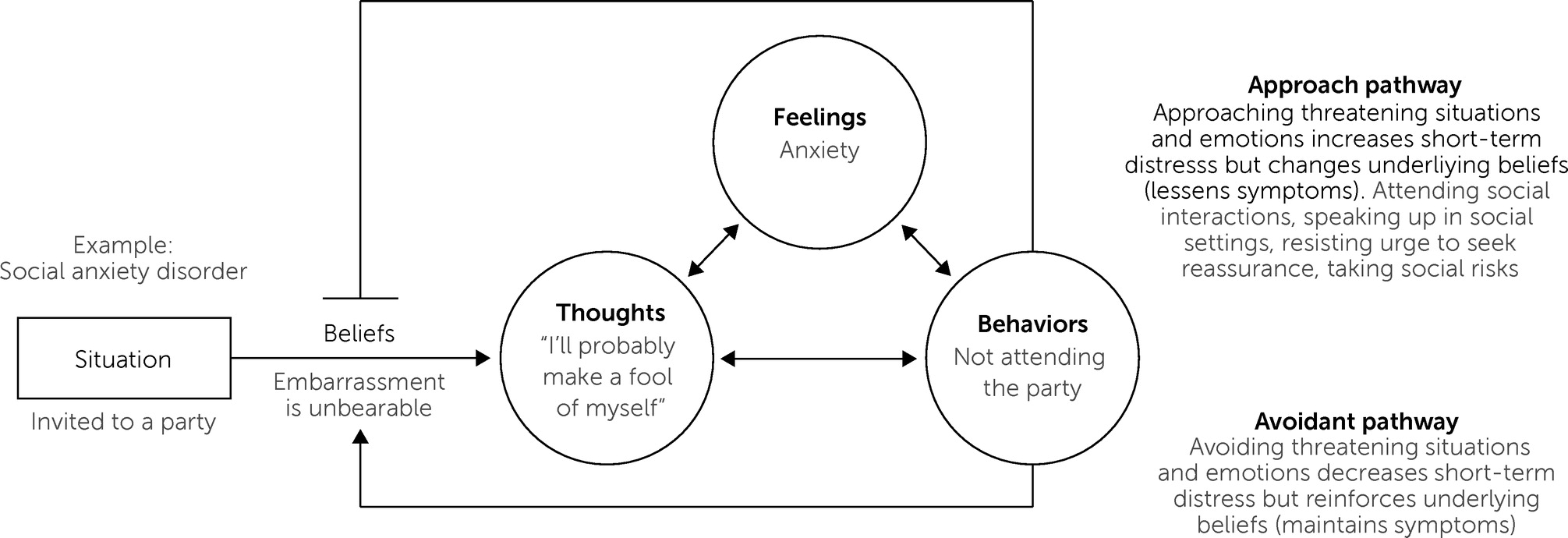
A transdiagnostic CBT model is presented in
Figure 1, which we illustrate using an example patient with social anxiety disorder. The patient’s highly distressing fears that they will embarrass themselves lead to chronic avoidance of social situations. CBT typically begins with psychoeducation, in which patients learn how emotions have adaptive functions (e.g., anxiety helps prepare for and avoid possible danger) and how they are are beneficial when calibrated to reality (i.e., aligned and proportionate to the facts of a given situation) (
56). Through both didactic discussion and self-monitoring homework exercises, patients learn about the CBT model of psychopathology. They learn to see their symptoms as recurring cycles of thoughts, feelings, and behaviors; how these cycles emerge in response to situations because of underlying belief systems; and how habitual cognitive and behavioral reactions to these situations only serve to reinforce these beliefs, thereby maintaining their problem.
For example, when a patient is invited to a party, the belief that “embarrassment is unbearable” becomes activated, leading to a negative automatic thought (e.g., “I’ll probably make a fool of myself”) and concomitant feelings (e.g., anxiety, elevated heart rate, or tension or tightness in the pit of their stomach). Although habitual strategies for regulating these feelings (e.g., avoiding the party) may immediately reduce distress, they only reinforce the maladaptive belief that embarrassment is unbearable by generating additional evidence that one must avoid social gatherings to be “safe” from embarrassment. Reinforcing this belief means that the same cycle of symptoms will arise in future social situations. During treatment, these behaviors will consequently be labeled as part of an “avoidant” pathway that is ultimately unhelpful to long-term well-being. The patient will be encouraged to replace these avoidant responses with skills that move them down an “approach” pathway. Although approaching social situations and embarrassment (e.g., attending parties or speaking in social settings) can generate distress, doing so gives patients evidence that can erode underlying maladaptive beliefs. For example, signing up for improvisation classes and learning that they can survive an hour in the spotlight can help patients form new beliefs that embarrassment is tolerable, thus freeing them from social anxiety. Note that although this example focuses on social anxiety disorder, these dynamics are also highly relevant to narcissistic dysregulation (discussed later).
There are many CBT techniques for shifting patients from avoidance to approach pathways and transforming their underlying beliefs. Two major classes of interventions include
cognitive and
behavioral skills. Cognitive interventions ultimately aim to increase the flexibility with which patients think about themselves, others, and the world (
57). Patients first learn about different layers of cognition, including their “automatic thoughts” (i.e., immediate, situation-specific interpretations that come to a person’s mind throughout the day), “intermediate beliefs” (i.e., general attitudes and assumptions that give rise to automatic thoughts such as, “If I don’t wash my hands, then I’ll get sick”), and “core beliefs” (i.e., the deep, long-standing, and rigid beliefs about oneself and the world that can be expressed in simple declarations like, “I’m unlovable”) (
58). Patients then learn cognitive techniques that they can use to challenge and change these layers of cognition. Using cognitive restructuring to summon evidence against one’s automatic thoughts and generate alternative interpretations can help improve mood and reduce symptoms (
59–
62). Cognitive interventions provide patients with the skills to change their thoughts and beliefs (indicated by a circle and an arrow, respectively, in
Figure 1).
Behavioral interventions challenge patients to directly change their behavior (indicated by a circle in
Figure 1), giving them evidence that interrupts their beliefs (indicated by an arrow in
Figure 1) and helps free them from the cycle of their symptoms. After patients develop an awareness of the behaviors they habitually use to avoid uncomfortable emotions, they then engage in “behavioral experiments,” “exposure exercises,” or “behavioral activation plans” in which they purposefully confront situations that they fear and avoid. These can be a wide variety of activities, including giving a speech in front of strangers, sending e-mails with typos in them, holding doorknobs that might have germs on them, planning positive events, or any other exercises that help them approach situations or sensations that they fear or avoid. A substantial body of research shows that behavioral exposures can drastically reduce a patient’s fear and avoidance of these situations, thereby improving their functioning (
63–
70). Theoretically, the patient begins to build new associations with these situations that foster the belief that they can cope (
71). Of key importance is that patients learn to resist avoidant (or “safety”) behaviors during exposures (e.g., taking lorazepam before every exposure or washing their hands immediately after the exposure), as this inhibits the patient’s learning that they can cope with feared situations or emotions without avoidance (
72). Some exposure exercises can be extremely distressing, meaning that providing a clear rationale for this approach and collaboratively working up to more difficult exposures are essential for the sustainability of this powerful and empirically proven intervention.
Meta-analyses show that treatments under the CBT umbrella improve symptoms and are often considered the gold-standard treatment for a wide range of psychiatric presentations (
73,
74). This list includes internalizing disorders, such as major depressive disorder (
66,
75), social anxiety disorder (
76), panic disorder (
67,
77), and PTSD (
78,
79); externalizing disorders, such as drug and alcohol use (
80), attention-deficit hyperactivity disorder (
81), and oppositional defiant disorder (
82); personality disorders, including borderline personality disorder (
83,
84) and personality disorders comorbid with other disorders such as PTSD (
85) or major depressive disorder (
86); suicidal thoughts and behaviors (
87); bipolar disorder (
88); and psychosis (
89,
90). The time has come to consider how CBT could be adapted for NPD and self-esteem dysregulation more broadly.
A CBT Formulation of Narcissistic Self-Esteem Dysregulation
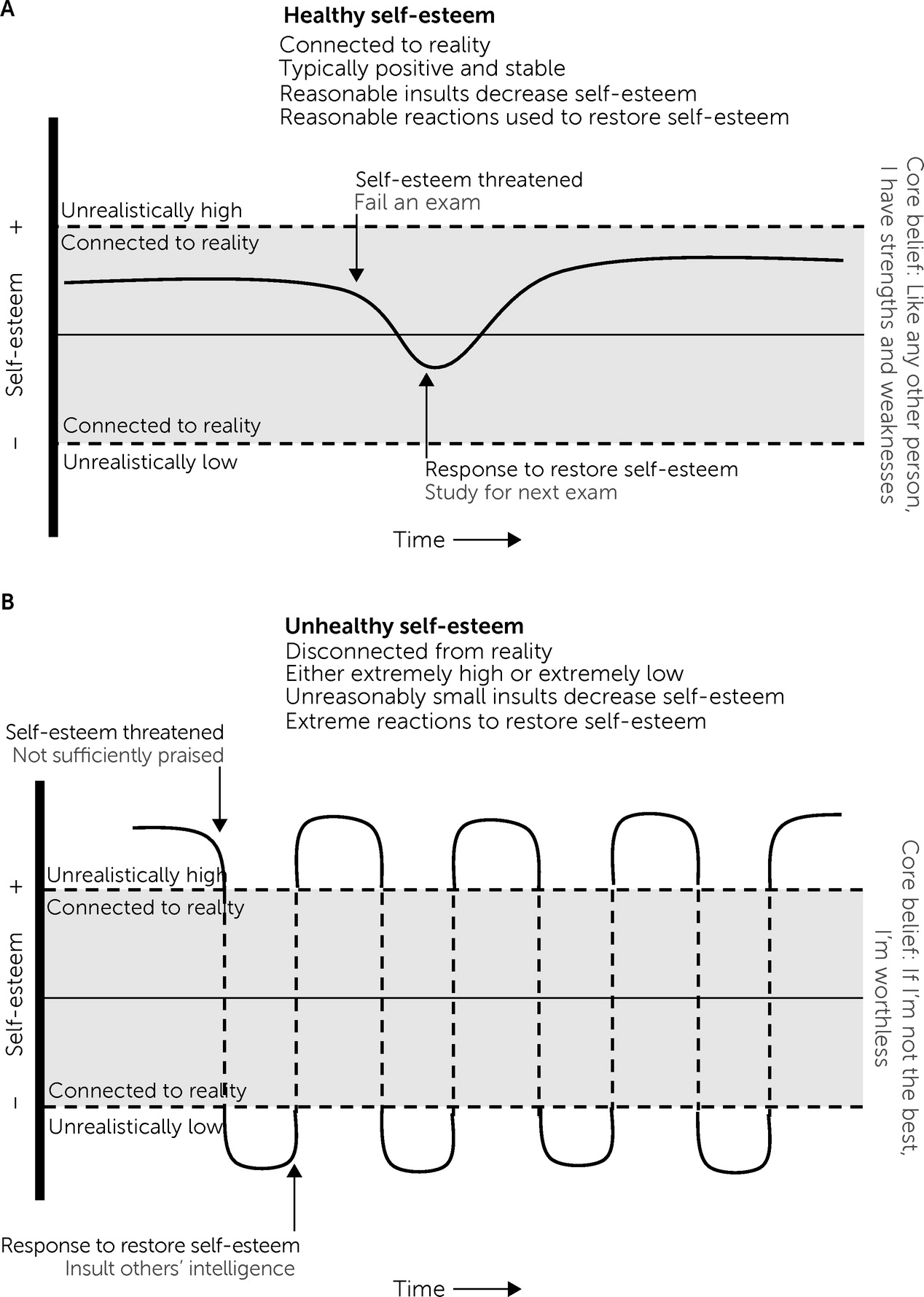
Generating a CBT approach to NPD requires identifying the key beliefs that generate dysregulation, the habitual avoidant behaviors that reinforce those beliefs, and a potential set of cognitive and behavioral interventions that could interrupt these habits and transform maladaptive beliefs to healthier versions. We outline these three steps in the present section, drawing on the principles and literature outlined in the previous sections. A conceptual model of healthy and unhealthy self-esteem dysregulation is illustrated in
Figure 2. Healthy individuals, overall, have relatively positive and stable self-esteem, which is consistently connected to reality (
Figure 2A). This means that one holds reasonable expectations of oneself and how one should be treated. Healthy self-esteem is still sensitive to environmental feedback, falling when there are threats to one’s self-esteem and rising when one’s abilities and standing are affirmed. Self-esteem threats involve challenges to one’s competence, influence, attractiveness, social regard, or overall “goodness” (e.g., when rejected, when receiving negative feedback, or when performing worse than others). Scholars agree that experiences in which one suffers decreased self-esteem generate negative emotions including shame, embarrassment, envy, anxiety, and anger (
13,
20,
91). These threats and concomitant emotions then activate efforts to “restore” self-esteem that both alleviate negative emotions aroused by the self-esteem threat and (when operating optimally) help the person grow their skills, social regard, and potential to contribute to society. In other words, self-esteem regulation is “the spice of life,” as it is a healthy and powerful promoter of both intrapersonal and interpersonal functioning (
12). Being able to maintain this healthy self-esteem regulation circuit requires maintaining reasonable expectations for oneself and choosing constructive means for restoring self-esteem. This healthy regulation thus flows from a set of core beliefs such as “like others, I have natural strengths and weaknesses,” “I can get better at things through hard work,” and “I have inherent value.”
However, this system can easily become dysregulated, leading to narcissistic symptoms (and, in extremes, NPD). This dysregulation can take many forms, but the key point of fragility lies at the interface of unrealistic expectations of oneself and destructive means for restoring self-esteem (for examples, see
Figure 2B and
Table 1). If a person believes that they are not valuable unless they attain extraordinarily high standards (e.g., “if I’m not the best, I’m worthless” or “I deserve praise for all that I do”), then even quotidian experiences will threaten one’s self-esteem. Insufficient acknowledgment, minor mishaps, or exposure to more accomplished others will all trigger cognitions and emotions reflecting an extreme dip in self-esteem in which one feels incompetent and valueless. Indeed, narcissism is associated with elevated negative affect in response to others’ dominance (
92). This distress can then trigger excessive behavioral reactions aimed at downregulating emotions, restoring self-esteem to unrealistically high standards (
19), for example, by bringing others “down a peg,” behaving pompously, or giving up. In our model, these behavioral reactions can vary across individuals, but all aim to restore self-esteem (see
Table 1 for examples). In fact, it is possible that the documented differences in “vulnerable” and “grandiose” subtypes of NPD (
93,
94) could be explained by different behavioral strategies that patients use to restore their self-esteem. For instance, a “vulnerable” narcissistic profile would emerge from responses that restore esteem by removing oneself from potential sources of ego threat (e.g., not engaging during class, not responding to friends, or seeking suicide). A “grandiose” presentation would emerge from behaviors that instead elevate one’s comparative standing over others (e.g., flaunting one’s successes, putting others down, or defying rules).
Special consideration should be given to the function of suicidal thoughts and behaviors (STB) in narcissistic dysregulation, particularly fantasizing about suicide or acting on suicidal urges (
30). As we have noted, narcissistic dysregulation can produce immense and frequent distress, which can generate a desire to downregulate and escape these painful feelings through death. Although such a desire to escape distress can motivate STB transdiagnostically (
95,
96), suicidal ideation and urges can serve additional functions in NPD, as suicide can seem like a pathway to quit a life in which one’s self-concept is irrevocably tarnished with no way to meet one’s idealized expectations (
97); gain ultimate control over one’s life by permanently ending it; restoring one’s standing relative to others by vengefully showing others that they were insufficient to help; or achieving a glorified version of one’s death (
30). Although these perceived benefits of dying by suicide might temporarily restore one’s sense of agency or relative standing to others, they also obviously bring immense pain to oneself and one’s community. As such, STB should be targeted early in treatment and understood within the aforementioned functional model.
To summarize this model, we propose that self-esteem regulation is a natural psychological process in human beings. People experience threats to their self-esteem, which generates aversive emotions that are regulated through learned behaviors that seek to restore self-esteem. This regulatory cycle is governed by (and, in turn, reinforces) underlying core beliefs about oneself and the world. Healthy self-esteem emerges when people have reasonable beliefs about oneself and use constructive responses to restore self-esteem. Unhealthy self-esteem emerges when people have unrealistic beliefs about themselves and others, leading to frequent self-esteem threats and immense, destructive attempts to restore self-esteem.
Furthermore, this dysregulated cycle can be understood through the lens of the CBT model described in
Figure 1. When someone with NPD is exposed to a situation that threatens their self-esteem, underlying beliefs become activated that produce distorted cognitions and intense emotions. Habitual behavioral responses can momentarily reduce negative emotions and restore self-esteem, but they only reinforce the maladaptive belief, recapitulating the cycle each time the individual’s self-esteem is threatened. Specific examples of this cycle are articulated in
Table 1. Behaviors indicative of classic narcissistic traits (e.g., need for admiration, fantasies of infinite success, suicidality, haughtiness, grandiose self-importance, and envy) can be understood through CBT components. Because of unrealistic underlying beliefs, any situations that threaten one’s sense of value, competence, power, and control germinate automatic thoughts organized around restoring a perceived sense of superiority. These thoughts provoke strong emotions, motivating internal and external behavioral reactions (e.g., escaping, lying, or aggressing) that may, indeed, restore a perceived sense of safety, perfection, or superiority but at the cost of healthy interpersonal functioning. Furthermore, these reactions only reinforce the underlying belief that perceived superiority is worth attaining at all costs. Although we chart only a few examples of narcissistic thought-feeling-behavior cycles, we use them to illustrate what we believe is a general process underlying dysregulated self-esteem.
The key benefit of analyzing narcissistic self-esteem dysregulation through this lens is that it opens this psychological process to modification through CBT techniques. Many relevant therapeutic skills fall under the umbrella of CBT, but we outline key potential approaches in the following text and in
Table 2. CBT typically begins with psychoeducation on the CBT model and how it connects to a patient’s current symptoms. As such, we argue that patients with NPD should be informed of the diagnosis and fully brought into the conversation regarding their clinical conceptualization (
42). After reviewing the models illustrated in
Figures 1 and
2, therapists can assign patients to use self-monitoring exercises to gain a greater awareness of what behaviors they might use to “restore” their self-esteem, which could be maladaptive in nature. Therapists and patients can then explore and identify the deeper assumptions and beliefs that underlie these ego sensitivities. The goal of this information-gathering stage is to build a working knowledge of how patients’ habitual cognitions and avoidant behaviors emerge from and reinforce their underlying beliefs. This serves as a foundation for learning cognitive and behavioral skills that can change these habitual responses and the beliefs that produce them.
Cognitive skills for narcissistic dysregulation would help patients habitually challenge automatic thoughts that generate distress and only reinforce underlying maladaptive beliefs. Automatic cognitions are likely to suffer from classic “cognitive distortions” through which thoughts and interpretations neglect parts of reality (
58). For example, cognitions might habitually deny the positive aspects of situations (e.g., thinking “I’m a failure” when patients receive both praise and critical feedback) or taking responsibility for an outcome even when all things are multiply determined (e.g., thinking “no one else is doing anything to make this project succeed” when collaborating on a project). Patients can then learn strategies for being more skeptical about these automatic thoughts and perhaps restructure them. For example, patients can learn to attend to the evidence that they still have value even when they are imperfect or that group projects benefit from shared effort and control. In these ways, habitual restructuring can help soothe negative affect in the face of self-esteem threats and regulate the patient’s behavioral attempts to restore self-esteem.
There are also several behavioral skills that could help stabilize narcissistic dysregulation. These interventions would focus on helping patients
approach distressing situations, cognitions, and emotions that they typically avoid in order to learn that they can tolerate these experiences without the need for their habitual destructive reactions. This facilitates a corrective experience in which patients learn new beliefs that the situations that they typically avoid are actually tolerable. When treating narcissistic dysregulation, the goal of behavioral exposures would be to help patients approach situations that threaten self-esteem (which they typically avoid) and choose healthier behaviors to restore self-esteem rather than their typical strategies. Gaining mastery through more effective coping generates more durable self-esteem. For instance, someone with the belief that they must always be seen as the most intelligent person could practice allowing their coworker to take the lead on a project and resist urges to correct them or withdraw from the project. As is well known in exposure-based interventions, this practice can increase distress and requires clear rationale setting and collaboration to help the patient approach and learn from these exposures. One strategy would be to first identify and remove habitual avoidant behaviors in patients’ daily lives (even if they are not related to self-esteem), providing the patient with practice in habituating to strong emotions and engendering confidence in behavioral skills. The ultimate goal is for patients to develop increased willingness to approach situations they typically avoid and healthier skills for managing the emotions that are generated by them, thereby changing their underlying belief network and alleviating their overall symptoms (
98).
Discussion
We outline a CBT approach to narcissistic self-esteem dysregulation that most mental health professionals can easily adapt into their practice. Narcissistic traits can be understood as a set of habitual thoughts, feelings, and behaviors that emerge because of maladaptive beliefs about oneself that essentially set unrealistic expectations for oneself and how one should be treated. When unmet, such expectations lead to rapid and extreme oscillations in self-esteem that generate strong negative emotions and require excessive and destructive reactions to restore self-esteem. However, this cycle can be regulated through cognitive and behavioral interventions that help patients modify their automatic thoughts and approach feared situations and emotions. These exercises can bring beliefs into a healthy connection with reality, relieving patients of their symptoms.
Although several treatments have been developed to aid people affected by narcissistic dysregulation (
37–
43), cognitive-behavioral perspectives are scarce (although not nonexistent) (
99). We believe that the current formulation provides several advances beyond prior work. In particular, our model unites the perspective that self-esteem dysregulation is at the heart of NPD (
12–
15) with classic components of CBT theory (
58). In particular, we articulate how rapid self-esteem oscillations typical of narcissistic fragility can be understood through self-perpetuating cycles of cognitive-affective-behavioral dysregulation that emerge from and reinforce maladaptive belief systems
. This formulation opens the psychological processes that underlie NPD to modification through classic CBT techniques and to scientific study. Both of these advances are key for the study and treatment of NPD. Further refining a CBT formulation of NPD will allow both scientific and clinical efforts to make greater headway in understanding and treating NPD. This is especially promising, given the power that CBT has in effectively treating many other forms of psychopathology (
73,
74).
Another key strength of the current model is its potential for understanding “narcissism” as a dimensional (rather than categorical) and transdiagnostic phenomenon. Scholars have questioned categorical taxonomies of psychopathology and instead advocated for identifying the dimensions that might vary continuously in a population and be shared across several disorders (
32–
34,
100,
101). Our model is consistent with this approach, as self-esteem (dys)regulation is a phenomenon that can vary continuously across people and emerge in several forms of psychopathology beyond NPD. In our model, everyone experiences self-esteem threats and has ways to restore self-esteem, and this system merely becomes dysregulated in NPD. We encourage additional attention to the processes that dysregulate the self-esteem system, as we believe this can help clarify what leads to NPD. We also encourage exploration of self-esteem and its dysregulation in other clinical disorders (e.g., borderline personality disorder, depression, perfectionism, obsessive-compulsive disorder, and social anxiety disorder).
It is crucial to keep in mind several limitations of our model as it stands. First and foremost, it remains largely theoretical (emerging from a synthesis of prior research and clinical observation) and, as such, has little direct empirical validation. Research is needed to establish key assumptions of the model (e.g., Do people with NPD endorse maladaptive beliefs concerning self-esteem? Do symptoms of NPD function to regulate distress and restore self-esteem?) and to test the potential use of CBT interventions to treat NPD. A second major limitation is that core beliefs are well known to be highly resistant to modification (
102). This means that the CBT formulation articulated here might require incorporating additional tools and techniques, such as those of schema therapy, which has been shown to be effective in the treatment of personality disorders (
103). This might be especially important in the treatment of NPD, as people who are highly ashamed of feeling inferior or incompetent are likely to use destructive reactions to restore self-esteem in the context of treatment (
19,
99,
104). Borrowing techniques from dialectical behavior therapy could establish additional tools that help patients and therapists work together to address narcissistic reactions during treatment (
54). A third limitation concerns the possibility that self-esteem dysregulation may only be one component of NPD, and full treatment of this disorder could require additional interventions. Other important future directions include more closely connecting the model proposed here to classic studies of self-esteem and its development (
4,
5,
13,
14,
20,
105–
108), investigating the utility of CBT-adjacent techniques such as motivational interviewing and mindfulness-based techniques in treating narcissistic dysregulation (
109,
110), and charting how self-esteem dysregulation develops within an individual across the lifespan (
106,
111–
113).
In all, a cognitive-behavioral formulation of narcissistic self-esteem dysregulation could help patients diagnosed as having NPD change underlying beliefs and come to greater intrapersonal and interpersonal functioning. This model may be general enough to address transdiagnostic issues with self-esteem dysregulation, but additional clinical and empirical research are needed.